By Fouzia Zeeshan Khan1, Fatima Fasih1, Samina Baig2, Ambreen Fatima1, Erum Bibi2, Sahar Iqbal1
AFFLIATIONS:
- Department of Pathology, Dow International Medical College, Dow University of Health Sciences (DUHS), Karachi, Pakistan.
- Microbiology Section, Dow Diagnostic Reference and Research Laboratory (DDRRL), Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-3/004
ORCID iD: 0000-0002-3312-5809
How to cite: Khan FZ, Fasih F, Baig S, Fatima A, Bibi E, Iqbal S. Frequency of Human Immune Deficiency Virus (HIV) Infections at Tertiary Care Hospital of Karachi from 2017-2019. Pak J Med Dent. 2022;11(3):17-23. doi: 10.36283/PJMD11-3/004
Background: Human immunodeficiency virus (HIV) is the world’s most serious health problem. Pakistan is included among high prevalent countries and two outbreaks of HIV have been reported one in 2018, in Sargodha (Kot Momin) and the other largest so far in 2019 in Larkana, first time infecting children as well. Therefore, a study was designed to find out the frequency as well as risk factors involved in the transmission of HIV.
Methods: This was a retrospective cross-sectional study (n=28,679), conducted in the Microbiology laboratory of Dow Diagnostic Reference and Research Laboratory (DDRRL), Karachi, Pakistan from 1st January 2017 to 31st December 2019. Serum samples were screened for the presence of HIV antigen and antibody by using HIV combo ARCHITECT i2000 SR, chemiluminescent immunoassay (CMIA). The Chi-square was used to analyze the data and a p-value of <0.05 was considered statistically significant.
Results: The total HIV-positive samples were 198 (0.69%). The mean age was 30.39 ± 10.1 with a predominance of males 158 (79.8%) followed by females 39(19.7%) and trans-genders 1(0.5%). The most prevalent ethnic background was Sindhi 40(20.2%) followed by Urdu speaking 32(16.2%). The major risk factors were sexual contact (25%) and surgical procedure (13%). The research found the highest incidence reported in Malir District (17.12%) followed by East (13.63%) and West (11.6%) of Karachi. The most significant association (p<0.001) of HIV was found with age.
Conclusion: The male population from the Malir district of Sindhi ethnicity had a high frequency of HIV. Moreover, sexual contact and surgical procedures were found major risk factors for HIV.
Keywords: Human Immunodeficiency Virus (HIV); Risk Factors; Sexually Transmitted Diseases; Epidemic.
Human immunodeficiency virus (HIV) is the world’s most serious health problem. HIV causes acquired immunodeficiency syndrome1. It adversely affects the human immune system and reduces CD4/T cells. These individuals are more susceptible to get opportunistic infections2. HIV infection is transmitted through body fluids from HIV patients such as blood, breast milk and vaginal and semen secretions3. There are enduring myths that HIV can be transmitted through shaking hands, hugging, kissing, sharing personal objects, food or water, coughing/sneezing, sweat, sharing clothes, and through insects’ bite4. Inadequate knowledge can lead to a misperception of disease among people. The first case of HIV was found 39 years ago in west-central Africa5.
According to global HIV and AIDS statistics, worldwide around 36.7 million individuals were infected with HIV in 2018. The HIV infection has spread in Pakistan all along, with an increasing number of deaths since 19876. Pakistan is among the four countries in Asia, including Afghanistan, Bangladesh and the Philippines, where the predictable number of emerging HIV infections has been growing yearly since 1990 7. There are many contributing factors, which impose a great challenge to healthcare clinicians to fight against HIV epidemic. Pakistan is a densely populated country with a low literacy rate. Lack of awareness regarding family planning, lack of contraceptive uses, increase in homosexuality, unchecked transfusion of blood and other body fluids, intravenous drug addiction and needle prick injury are the leading risk factors in spreading HIV/AIDS8. Moreover, inefficient sterilization practices during medical and surgical procedures as well as poor healthcare waste management systems are also important contributing factors to the spread of HIV infection9. Therefore, it is required to take precautions and immediate actions to limit the spread of HIV /AIDs in Pakistan. Moreover, a multifaceted approach should be adopted along with a substantial emphasis on education to fight against social obstruction and carelessness. This study aimed to assess the frequency of HIV and associated risk factors.
This retrospective observational study (n=28,679) was carried out in the Microbiology Section, Dow Diagnostic Reference, and Research Laboratory (DDRRL) from1st January 2017 to 31st December 2019. The study was started after getting approval from the Institutional Review Board (IRB-176/DUHS/Approval/2020/) of Dow University of Health Sciences.
The non-parametric data of HIV screening were retrieved from the medical record (laboratory data software) of the Microbiology section. It included samples from different collection centers both within and outside the city. The sera of registered cases were screened for HIV combo by using ARCHITECT i2000 SR. The ARCHITECT HIV Ag/Ab Combo assay is a chemiluminescent immunoassay (CMIA) used for simultaneous detection of human immunodeficiency virus p24 antigen and antibodies to HIV-1 and HIV-2 in human serum and plasma. The presence or absence of HIV-1 p24 antigen or HIV-1/HIV-2 antibodies in the specimen is determined by comparing the chemiluminescent signals to the reaction cutoff signals determined from ARCHITECT Ag/Ab Combo calibration.
Samples with signals to cutoff values >1 were considered nonreactive. In the case of a positive sample, the patient’s history was acquired along with a fresh sample for repeat testing. All HIV-positive sera were sent to the HIV Sindh referral laboratory for confirmation. The study included only all samples registered for detection of HIV infection irrespective of age and gender. The research excluded samples registered for repeat testing of HIV detection and having a lack of demographic information. The Statistical Package for Social Science (SPSS version 20) software was used for frequencies and percentages of demographics of positive cases. The Chi-square was used to analyze the data and a p-value of <0.05 was considered statistically significant.
Of the total 28,679 cases, 198 (0.69%) were HIV positive with a mean age of 30.39 ± 10.162. The most affected age group was group 2 (Table 1). The majority were Pakistani with a predominance of males (79.8%). The most common ethnic group was Sindhi (20.2%) and Urdu speaking (16.2%).
Table 1: Distribution of human immunodeficiency virus (HIV) based on gender and age group of subjects.
| Age Grouping | Negative
n=28480 |
Positive
n=198 |
p-Value
|
||
| Male
n (%) |
Female
n (%) |
Male
n (%) |
Female
n (%) |
||
| Group 1
(0-20 years) |
1,261(4.42%) | 1229(4.31%) | 17(0.05%) | 4(0.01%) | <0.001 |
| Group 2
(21-40 years) |
8,405(29.51%) | 11385(39.97%) | 119(0.41%) | 26(0.09%) | |
| Group 3
(41-60 years) |
2,946(10.34%) | 1609(5.64%) | 24(0.08%) | 9(0.03%) | |
| Group 4
(>60 years) |
950(3.33%) | 695(2.44%) | 0 | 0 | |
Among them, 121 (61.1%) were married. Affected cases belong to different professions including field workers, office employees, jobless individuals, domestic women and students (Table 2).
Table 2: Demographic characteristics of human immunodeficiency virus (HIV) positive cases with frequency and percentage distribution.
| Categories | Frequency n (%) | |||||
| Gender | Male | Female | Transgender | |||
| 158(79.8) | 39(19.7) | 1(0.5) | ||||
| Marital Status | Single/Unmarried | Separation | Married | Second marriage | Widow | |
| 69(34.8) | 1(0.5) | 121 (61.1) | 02 (1.0) | 5(2.5) | ||
| Nationality | Pakistani | Afghani | ||||
| 195 (98) | 03 (02) | |||||
| Ethnicity | Sindhi | Punjabi | Pashto | Seraiki | Memon | |
| 40(20.2) | 13(6.56) | 31(15.6) | 03(1.5) | 02(1.0) | ||
| Urdu speaking | Afghani | Hindko | Balochi | Any other | ||
| 32(16.2) | 03(1.5) | 01(0.5) | 17(8.5) | 56(28.28) | ||
| Profession | Office workers | Field workers | Jobless | House women | Student | Labor |
| 20 (10) | 99(50) | 18 (9.09) | 19 (9.6) | 11 (5.5) | 31(15.65) | |
The highest risk factor was sexual contact (25.25%) (Figure 1). This study population belonged to various districts, including Central, East, Malar, South, West, and Korangi and 79 were from outside the Karachi city (Figure 2).
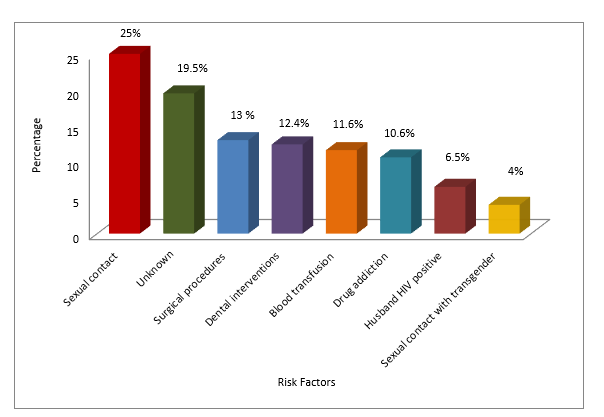
Figure 1: Risk factors reported in the human immunodeficiency virus (HIV) positive cases.
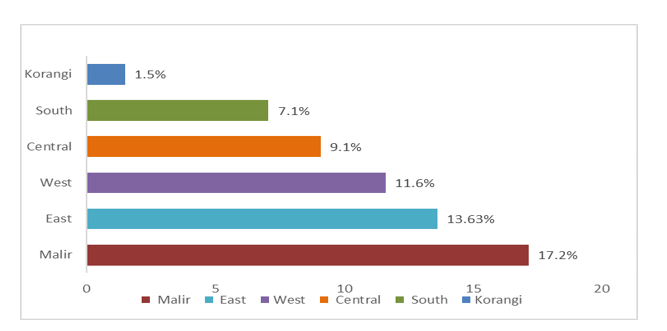
Figure 2: Distribution of human immunodeficiency virus (HIV) positive cases among different districts of Karachi.
The current study reported male predominance having HIV with a mean age group of 30.39±10.162, as endorsed by another study10. Sindh showed the highest prevalence in the current study with a predominance in the Malir district. The distribution of places among HIV cases directly corresponds to the national data8. The recent outbreak of HIV in Sargodha and Larkana represents a very distressing situation10. The human immunodeficiency virus (HIV) is a worldwide threat. It is estimated that 37.9 million people are suffering from HIV-1 11. During 2005, more than 4 million people were affected and 3 million people died from the disease2. According to the Centers for Disease Control and Prevention (CDC), thirty-eight thousand new cases have been recognized annually in the following decade3.
In 1987, the first case of HIV was detected in Pakistan raising its rank among the highly saturated epidemic countries4. Pakistan hit the peak worldwide ranking with an average of 17.6% by reporting an increasing number of cases from 8,360 to 45,990 from 2005 to 2015. It is estimated that 130,000 HIV-positive people are living in Pakistan5. In 2018, an outbreak of HIV in Sargodha near Kot Momin was reported. It was misdiagnosed with Hepatitis B or C or Tuberculosis but due to treatment failure, patients were directed to the District Headquarter Hospital in Sargodha for final diagnosis. Approximately, 1.29% of the dwellers of the village were HIV positive6,7.
Furthermore, in 2019, the largest outbreak of HIV in Larkana was reported with the involvement of children being recorded for the first time8. It is a common observation that medical and social networks are reluctant to talk about HIV/AIDS in a contented environment, which adversely affects planning strategies to combat HIV/AIDS in Pakistan12. Social humiliation associated with the disease further worsens the scenario13. Less awareness regarding health issues and dependence on non-professional Hakeem and traditional therapists resulted in intense progression and worsening of the disease. Economic, public and political negligence is the most important contributing factors in intensifying its magnitude14.
The national surveillance data notified three main causes of the spread of HIV in the country including sexual contact, injectable drugs and insecure blood transfusions15-18. Concerning these risk factors, sexual contact was predominant in this study19. Sexual transmission constitutes more than 70% of collective cases of HIV. Discussions about such problems are considered taboo and publicly such talks are condemned.5 It is necessary to indicate that the epidemic of HIV in Pakistan largely involves drug abusers, comprising approximately 38% of registered cases6,20. This study also reported that 18% of HIV patients, which consequently persuaded us to share that the easy availability of injectable drugs (i.e., narcotics) should be discouraged as it is also one of the main causes of HIV infection. This study helps to acknowledge the relationship between the uncontrolled sale of narcotics/opioids and the recent HIV outbreak in Pakistan.
The current study declared that 8% of HIV cases as a result of sexual relationships with transgenders. Integrated Biological and Behavioral Survey reported that the frequency of HIV-positive cases included 38.4% drug inducers, 7.1% transgender, and 2.2% female sex workers21,22. The increasing trend of the occurrence of HIV in sex workers, drug abusers and transgenders could be due to difficulty in getting employment. HIV/AIDS 2017 United Nations survey, stated that the use of condoms was extremely low among transgenders (24%) and men who have sex with men (22%) 23. Psychological stress and a high rate of drug dependence play an important role in acquiring HIV about sexual behavior in transgenders24. The current study claimed that a higher prevalence of HIV is due to unchecked blood transfusion and reuse of syringes, which is in harmony with the results of another study23. Transmission of HIV through contaminated blood is on the rise.
The main reason could be the use of substandard and non-validated screening instruments and methods. The recent event of Kot Imrana is quite exceptional that raised the occurrence of 1.29% to 13.38% in six months where there was an obvious depiction of using the same syringe on multiple patients. A quack, who was responsible for this also, died of HIV later in 2018 25. The national Safe Blood Transfusion Program is implementing guidelines for the safe transfusion of blood. According to these regulations, the license will be issued to only those blood banks which ensure good quality screening and safety of the blood products20. This study showed a prominent incidence of HIV due to the lack of use of sterilized instruments during surgical and dental procedures, endorsed by the most recent outbreak of HIV in Larkana, which demonstrated malpractice of healthcare professionals. Ansari et al. reported 26% and 40% of HIV cases from invasive surgical and dental procedures respectively21.
In this study, 43% of HIV-positive patients did not know the cause of their disease. Most of them were naive and did not have any knowledge about the route of transmission and the consequences of HIV. The negative behavior of society leaves disastrous effects on the well-being and health of HIV-positive patients25. The burden of HIV is more in married people as compared to the unmarried, the widows and the divorced in the present study. However, other studies contradicted to the findings22. There is an inverse relationship between HIV-positive individuals to the literacy levels in the present study, which agrees with another report26. HIV status is affected by the low level of education in developing countries. Pakistan is among the vulnerable countries with a low literacy rate, higher levels of poverty and huge resistance to awareness of sex education. Therefore, it is required to take effective measures and immediate actions to limit the spread of HIV /AIDs. A multipronged approach should be adopted along with a substantial emphasis on education to fight against social obstruction and carelessness.
There is an urgent need to identify HIV transmission areas and implementation of safe infection control practices. Health authority bodies should investigate fake health practitioners, especially in low socioeconomic and low literacy rate areas where people are at greater risk.
The mode of transmission as sexual contact and surgical procedures were found major risk factors for HIV. It was found that Sindhi males from Malir had a high frequency of HIV. Therefore, the National AIDS Control Programme of the Government of Pakistan should initiate HIV awareness programs, especially among males, screening methods and infection control strategies that will help in combating the spread of the infection.
The authors would like to acknowledge the Department of Microbiology (Dow University of Health Sciences, Karachi) for the provision of the data.
The authors declare no conflict of interest.
Ethical approval was obtained from the Dow University institutional review committee with the reference code: IRB-176/DUHS/Approval/2020/.
The consent was taken before the sample collection.
The research is a self-funded project.
FZK conceived the idea, collected the data and approved the manuscript. FF did the literature review, drafting of the manuscript and critical review. SB also collected the data and performed analysis and manuscript writing. AF critically reviewed the manuscript and interpretation of data. EB searched the data for literature review and assisted in data collection and analysis. SI reviewed the literature and initial drafting of the manuscript.
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844-845. doi:10.1001/jama.2019.1343
- Simon V, Ho DD, Karim QA. HIV/AIDS epidemiology, pathogenesis, prevention, and treatment. Lancet. 2006;368(9534):489-504. doi: 10.1016/S0140-6736(06)69157-5
- Centers for Disease Control and Prevention [Internet]. U.S. Department of Health and Human Services; 2019 [cited 2022 Mar 5]. Available from: https://www.cdc.gov/hiv/statistics/overview/index.html
- Alarming surge in HIV/AIDS cases in five districts of Punjab [Internet]. The Dawn; 2019 [cited 2022 Mar 10]. Available from: https://www.dawn.com/news/1487667#:~:text=FAISALABAD%3A%20The%20number%20of%20HIV,(PACP)%20for%20free%20medicines.
- Melesse DY, Shafer LA, Shaw SY, Thompson LH, Achakzai BK, Furqan S, et al. Heterogeneity among sex workers in overlapping HIV risk interactions with people who inject drugs: a cross-sectional study from 8 major cities in Pakistan. Medicine. 2016;95(12): 1-9. doi: 10.1097/MD.0000000000003085
- Ahmed A, Hashmi FK, Khan GM. HIV outbreaks in Pakistan. Lancet HIV. 2019;6(7):1. doi: 10.1016/S2352-3018(19)30179-1
- Ochani RK, Shaikh A, Asad A, Batra S. HIV outbreak in Pakistan–a wake-up call? Pak J Surg Med. 2020;1(2):98-99. doi: 10.37978/pjsm.v1i2.182
- Mansoor E, Azam N, Niazi SK, Sheikh N, Baig MA, Azim MT, et al. Rising HIV seroconversion rates & associated risks among employees of organization ‘X’: A case control study, Pakistan, 2017. Pak J Med Sci. 2020; 36(6): 1349-1354. doi: 10.12669/pjms.36.6.1735
- Letho Z, Yangdon T, Lhamo C, Limbu CB, Yoezer S, Jamtsho T, et al. Awareness and practice of medical waste management among healthcare providers in National Referral Hospital. PLoS One. 2021;16(1):1-10. doi: 10.1371/journal.pone.0243817
- Risher KA, Cori A, Reniers G, Marston M, Calvert C, Crampin A, et al. Age patterns of HIV incidence in eastern and southern Africa: a modelling analysis of observational population-based cohort studies. Lancet HIV. 2021;8(7):e429-e439. doi: 10.1016/S2352-3018(21)00069-2
- Pakistan NACP [Internet]. AIDS Epidemic Modelling Exercise for Pakistan; 2017 [cited 2022 Mar 10]. Available from: https://nacp.gov.pk/repository/whatwedo/surveillance/Book.pdf
- Abdullah MA, Shaikh BT, Ghazanfar H. Curing or causing? HIV/AIDS in health care system of Punjab, Pakistan. PLoS One. 2021;16(7):1-9. doi: 10.1371/journal.pone.0254476
- Li Z, Morano JP, Khoshnood K, Hsieh E, Sheng Y. HIV-related stigma among people living with HIV/AIDS in rural Central China. BMC Health Serv Res. 2018;18(1):1-7. Doi: 10.1186/s12913-018-3245-0
- Qureshi N, Shaikh BT. Myths, fallacies and misconceptions: applying social marketing for promoting appropriate health seeking behavior in Pakistan. Anthropol Med. 2006;13(2):131-139. doi: 10.1080/13648470600738716
- Khan AA, Khan A, Bokhari A. The HIV epidemic in Pakistan. J Pak Med Assoc. 2010;60(4):300-307.
- Dar HA, Mubashir A, Adil M, Farzeen A, Naseer H, Ayub G, et al. Revisiting the AIDS epidemic in Pakistan: where we stand and what we must aim for. AIDS Res Hum Retroviruses. 2017;33(10):985-992. doi: 10.1089/aid.2017.0042
- Zaheer HA, Waheed U. Blood safety system reforms in Pakistan. Blood Transfusion. 2014;12(4):452. Blood Transfus. 2014; 12(4): 452-457. doi: 10.2450/2014.0253-13
- Rabold EM, Ali H, Fernandez D, Knuth M, Schenkel K, Asghar RJ, et al. Systematic review of reported HIV outbreaks, Pakistan, 2000–2019. Emerg Infect Dis. 2021; 27(4): 1039-1047. doi: 10.3201/eid2704.204205
- Altaf A, Pasha S, Vermund SH, Shah SA. A second major HIV outbreak in Larkana, Pakistan. J Pak Med Assoc. 2016;66(12):1510-1511.
- Drug Regulatory Authority of Pakistan Act [Internet]. Drug Regulatory Authority of Pakistan; 2012. Available from: http://www.na.gov.pk/uploads/documents/1352964021_588.pdf
- Ansari JA, Salman M, Safdar RM, Ikram N, Mahmood T, Zaheer HA, et al. HIV/AIDS outbreak investigation in Jalalpur Jattan (JPJ), Gujrat, Pakistan. J Epidemiol Glob Health. 2013;3(4):261-268. doi: 10.1016/j.jegh.2013.06.001
- Cloete A, Strebel A, Simbayi L, Van Wyk B, Henda N, Nqeketo A. Challenges faced by people living with HIV/AIDS in Cape Town, South Africa: Issues for group risk reduction interventions. AIDS research and treatment. 2010;2010:1-8. doi: 10.1155/2010/420270
- Davlidova S, Abidi SH, Ali S. Healthcare malpractice and continuing HIV outbreaks in Pakistan. BMJ Glob Health. 2019;4(6):1-3. doi: 10.1136/bmjgh-2019-001920
- Nemoto T, Operario D, Keatley J, Nguyen H, Sugano E. Promoting health for transgender women: Transgender Resources and Neighborhood Space (TRANS) program in San Francisco. Am J Pub Health. 2005;95(3):382-384. doi: 10.2105/AJPH.2004.040501
- Zaid M, Ali M, Afzal MS. HIV outbreaks in Pakistan. Lancet HIV. 2019;6(7):418-419. doi: 10.1016/S2352-3018(19)30180-8
- Maan MA, Hussain F, Jamil M. Prevalence and risk factors of HIV in Faisalabad, Pakistan–A retrospective study. Pak J Med Sci. 2014; 30(1): 32-35. doi: 10.12669/pjms.301.4176
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
