By Ayesha Zafar1, Sana Tariq2, Afshan Bhatti3, Lubna Razzak4
AFFLIATIONS:
- Department of Physiology, HITEC Institute of Medical Sciences, Rawalpindi, Pakistan.
- Department of Research and Development, Tabba Kidney Institute, Karachi, Pakistan.
- Department of Obstetrics and Gynecology, Shaheed Mohtarma Benazir Bhutto Medical University, Larkana, Sindh, Pakistan.
- Department of Urogynecology, Tabba Kidney Institute, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-3/012
How to cite: Zafar A, Tariq S, Bhatti A, Razzak L. Association of Overactive Bladder Symptoms with Basal Metabolic Index: Physiological Traits as a Treatment Option. Pak J Med Dent. 2022;11(3): 75-81. doi: 10.36283/PJMD11-3/012
Background: An overactive bladder is characterized by a persistent urge to urinate, leading to spontaneous urination. Treatment of overactive bladder with mild to moderate exercises and lifestyle changes has been recommended. This study aimed to understand the association of the Basal Metabolic Index with overactive bladder symptoms and the effect of exercise on Over Active Bladder (OAB) in young females.
Methods: This is a prospective cohort study, Overactive Bladder Symptom Score (OABSS) was used to determine OAB symptoms, 8-14 times a day whereas and participants with positive results for overactive bladder symptoms were counselled for lifestyle changes such as water intake timings, and pelvic floor muscle exercise. After 3 months of 4 times, a week exercises and lifestyle modifications, the OABSS questionnaire was filled again. Paired sample t-test and chi-square test were used to analyze the significance of the data.
Results: A total of 380 participants were included in the study (mean age 23.7±3.9 years). According to age they were divided into 2 categories of 20-25 years and 25-30 years. The most-reported urinary symptom was increased frequency in 172 participants it was 8-14 times a day whereas, in 45 respondents results indicated frequency of more than 15 times a day. After 3 months OABSS presented significant improvement in symptoms. Furthermore, 288 (60%) participants were cured and 92 (24%) indicated improved results.
Conclusion: Moderate to severe symptoms of overactive bladder reported 32% occurrence among females of age groups between 20 to 30 years. This is indicating BMI is an independent risk factor and considers exercise as the first best treatment option for young patients.
Keywords: Overactive Bladder; BMI; Pelvic Floor Muscles; Exercise; Treatment.
Overactive Bladder (OAB) is characterized by a persistent urge to urinate, which can lead to spontaneous urination, OAB causes small amounts of urine to flow out automatically, from a few drops to a full dose. According to the Research Center on Aging Trusted Sources, the disease is most common in women and people over the age of 40. However, this condition can strike at any age. According to a study published in the Annals of Internal Medicine, more than 10% of women in the study, who was 22 years old, had OAB. Overactive bladder syndrome (OAB) 1.
OAB has the potential to adversely affect the normal quality of life, sexual function, sleep, and mental health. Urinary incontinence with or without urination, which is often accompanied by frequency and nocturnal, is described by international researchers2. Several studies have looked at the rise of OAB in industrialized countries and examined its impact on health quality, with varying results. The prevalence of low urinary tract infection (LUTS) and OAB were evaluated in one of the largest human-based studies ever conducted. The EPIC project was a telephone survey of people over the age of 18 conducted in five countries: Canada, Germany, Italy, Sweden, and the United Kingdom. The researchers used a computer-assisted telephone interview, followed by a questionnaire that examined patient-specific areas such as demographics and comorbidities. The study included about 19,000 people and found that the overall frequency of OAB was 11.8%, with similar levels for men and women3.
The prevalence of various symptoms in the community was assessed using the LUTS and OAB methods. According to the EPIC study, 10.8% of men and 12.8 percent of women have LUTS although it was more common for women (66.6 percent vs 62.5 percent). The sex difference is noticeable when storage and the signs of emptiness are separated. Women (59.2%) were more likely than men to have symptoms of constipation (51.3 %) 4. According to LUTS defining OAB, 12.8 percent of women and 10.8 percent of men reported having it. This study contradicts the widely accepted belief that OAB symptoms only affect adults5. However, the prevalence of OAB symptoms seems to increase with age6. Urinary incontinence (UI) is also well researched, with a wide range of spreads. Women had higher levels of urinary incontinence, while men had greater urinary incontinence (desire, mixed)7. The research study looked at the frequency of the study population, which varied greatly depending on the selected condition. It was usually seen as urinating too often during the day. The study found that 31% of men and 25% of women with OAB symptoms were more likely to use the system with the majority falling between five and eight discharges each day8.
The importance of basal metabolic index, obesity, and central obesity has been identified in many studies indicating excessive risk of OAB in obese females9,12. Moderate lifestyle changes, such as alteration of fluid intake timings and mild exercise including pelvic floor muscle strengthening exercises are known to improve OAB symptoms in young females more efficiently than in older patients13-15. Therefore, this study aimed to assess the frequency of Overactive bladder and understand the association of the Basal Metabolic Index with lower urinary tract symptoms and overactive bladder symptoms in young females. In Pakistan, this is a less evaluated topic and this research will work as a significant piece of evidence in the literature. This study will enable healthcare providers to assess the significance of exercise in treating overactive bladder symptoms in young females.
This is a prospective cohort study, conducted on the campuses of Suvastu School of Nursing and Health Sciences, Karachi. The study duration was from June 2021 to October 2021, females within the age limits of 20 years to 30 years were asked to join the study. The sample size was calculated with the help of the world health organization’s sample size calculator, the total female population within the age limits of 20-30 years in Pakistan was 19581.9, 95% confidence interval indicating a minimum sample size of 377. An informed consent along with exclusion criteria was provided to willing participants, females with positive pregnancy, lactating mothers, diagnosed with Urinary tract symptoms, and any renal or urinary disorder were excluded from the study. upon successful approval from participants, the primary investigator recorded the weight and height of all participants. afterward, a pre-structured questionnaire with two sections was given, section one consists of demographic details, and section two had overactive bladder symptoms score questionnaire.
The OABSS (overactive bladder symptom score) was developed to evaluate the frequency of different urinary symptoms present in early overactive bladder disease, this questionnaire has its calculation Likert scale for questions16,17. The overall result of OABSS was an accumulated score of all responses. The participants were asked to write down their responses, the participants with positive results for overactive bladder symptoms or lower urinary tract symptoms were educated about lifestyle changes such as water intake timings and pelvic floor muscle exercise. After 3 months of 4 times, a week exercises and lifestyle modifications, the OABSS questionnaire was asked to be answered again. Analysis of data included demographic details and OABSS scores before and after the intervention were entered and edited in the statistical package of social sciences (SPSS) version 21. Dependent variables were analyzed for frequency and percentages, while to evaluate the association of two variables paired sample t-test was performed. The significance of the data was checked with the chi-square test, p-value <0.005 was considered significant.
A total of 380 participants were included in the study, age was divided into 2 categories 20-25 years and 25-30 years. Thus, 218 (57.4%) participants were 20-25 years old while 162 (42.6%) were 25-30 years old, the mean age of study participants was 26.8 ± 3.2 years (Figure 1).
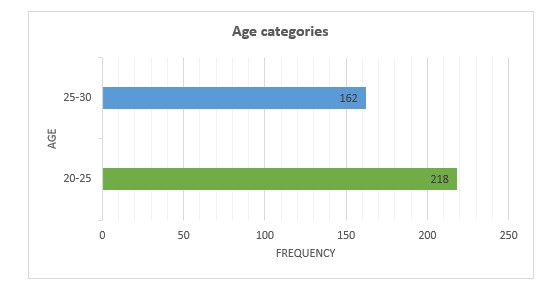
Figure 1: Age distribution of study participants.
The Basal Metabolic Index results were categorized into four standard categories, Underweight, Normal, overweight, and obese with 20 (5.3%), 317 (83.3%), 32 (8.4%), and 11 (2.96%) participants respectively. Although the maximum number of participants is within the normal weight range, overweight and obese participants were also in remarkable quantity. The questions of OABSS included frequency of urination in a single day (after waking up till sleep), Nocturia frequency per night, Urgency was described as not being able to hold urine for a longer time and having sudden or strong urge to urinate, urge incontinence was described as leakage of few drops of urine to hold the urge and incontinence was described as involuntary leakage of urine drops while laughing, coughing, sneezing, or holding weights, etc. The most-reported urinary symptom was increased frequency with 172 participants 8-14 times a day and 45 participants indicated > 15 times a day frequency of urination. Similarly, nocturia was reported at least once per night in 134 (%) participants.
Table 1: Overactive bladder symptoms score pre- and post-interventions.
| Parameters | Pre-Intervention | Post-Intervention | p-Value | |
| Frequency of urination | <7 time / a day | 163 (42.8%) | 366 (96.3%) | 0.005 |
| 8-14 time / a day | 172 (45.2%) | 14 (3.6%) | ||
| >15 time / a day | 45 (11.8%) | 0 | ||
| Nocturia | 0 time / night | 246 (64.7%) | 310 (81.5%) | 0.002 |
| 1 time / night | 134 (35.2%) | 70 (18.4%) | ||
| Urgency | not at all | 233 (61.3%) | 309 (81.3%) | 0.0001 |
| < 1 per week | 13 (3.42%) | 52 (13.6%) | ||
| 2-4 times a day | 134 (35.2%) | 19 (5%) | ||
| Urge incontinence | not at all | 366 (96.3%) | 372 (97.8%) | 0.06 |
| Once in a week | 14 (3.68%) | 8 (2.1%) | ||
| Incontinence | not at all | 378 (99.4%) | 378 (99.4%) | 0.1 |
| Once in a week | 2 (0.5%) | 2 (0.5%) | ||
Urgency and urge incontinence were reported positive in 134 (%) and 14 (%) participants respectively. Incontinence was described as involuntary leakage of urine drops while laughing, coughing, sneezing, holding weight, etc., reported in 2 (%) participants only. Overall results of OABSS were calculated after accumulating responses to all 5 questions, the questionnaire has the categories associated with results. The overall result of ≤ 5 is considered as No symptoms if all the answers are recorded without extreme values, 6 – 7 indicated mild symptoms, 8 – 9 were moderate symptoms category and 10 was indicated as severe symptoms category (Table 1).
Participants with Mild, moderate, and severe symptoms were educated about lifestyle changes benefits and pelvic floor muscle exercises and asked to perform these exercises at least once a day for 15 mins. After 3 months OABSS was scored again by the same participants and presented significant improvement in symptoms. Since 288 (60%) participants were cured with only pelvic floor muscle exercises and lifestyle changes, 92 (24%) indicated improved results (Figure 2).
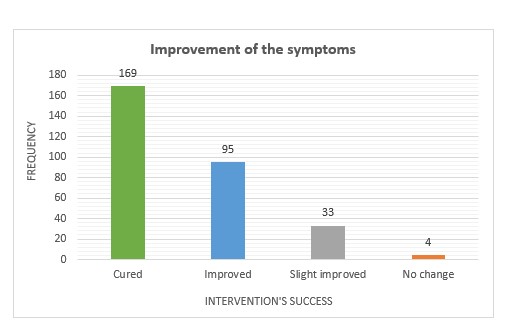
Figure 2: Post-intervention success according to the improvement of the symptoms of overactive bladder (OAB).
The actual changes in overall results of OABSS are described in Figure 2, indicating the enormous success of behavioral and physical activities on overactive bladder symptoms. The importance of BMI for overactive bladder symptoms has been discussed in Table 2, indicating excessive positive symptoms in overweight and obese young females as compared to normal-weight participants, indicating a significant p-value of <0.005 (Table 2).
Table 2: Association of symptoms with basal metabolic index.
| Parameters | Underweight | Normal | Overweight | Obese | p-Value | |
| Frequency of urination | <7 times/day | 8 (2.1%) | 142 (37.3%) | 7 (1.8%) | 3 (0.7%) | 0.0001 |
| 8 to 14 times/day | 8 (2.1%) | 131 (34.4%) | 17 (4.4%) | 3 (0.7%) | ||
| >15 times/day | 4 (1.05%) | 5(1.3%) | 8 (2.1%) | 23 (6%) | ||
| Nocturia | 0 times/night | 14 (3.6%) | 177 (46.5%) | 25 (6.5%) | 9 (2.3%) | 0.09 |
| 1 times/night | 6 (1.5%) | 5 (1.3%) | 39 (10.2%) | 98 (25.7%) | ||
| Urgency | not at all | 12 (3.1%) | 216 (56.8%) | 5 (1.3%) | 0 | 0.0001 |
| < 1 per week | 1 (0.2%) | 6 (1.5%) | 4 (1%) | 2 (0.5%) | ||
| 2-4 times a day | 7 (1.8%) | 74 (19.4%) | 23 (6%) | 9 (2.3%) | ||
| Overall score | No symptoms | 13 (3.4%) | 30 (7.89%) | 2 (0.5%) | 2 (0.5%) | 0.0001 |
| Mild symptoms | 3 (0.7%) | 162 (42.6%) | 12 (3.15) | 1 (0.2%) | ||
| Moderate symptoms | 2 (0.5%) | 7 (1.8%) | 41 (10.7%) | 48 (12.8%) | ||
| Severe symptoms | 2 (0.5%) | 1 (0.2%) | 6 (1.5%) | 36 (0.2%) | ||
The purpose of this study was to evaluate the frequency of overactive bladder symptoms in young females and assess the impact of short-term pelvic floor muscle training and lifestyle changes on positive symptoms. This is a highly prevalent disorder in young females, the current study indicated approximately 32% frequency of overactive bladder with moderate to severe symptoms in females aged between 20 to 30 years, research from the Netherlands mentioned a 12% prevalence rate in 1393 participants sample size18. The characterization of the overactive bladder has been described as urgency (sudden urge to urinate), increased frequency (urinating for more than 8 times a day), and urge incontinence (sudden and involuntary loss of urine). The age group indicating an increased risk of overactive bladder symptoms is known as childbearing age, pregnancy is an independent risk factor of OAB and young females already suffering from mild symptoms may experience severe OAB after conception and delivery.
In present study, the frequency of overweight and obese participants with reported OAB symptoms is like the data gathered by the national institute of the health of the United States of America, that data showed 97 million obese population and an increased prevalence of overactive bladder symptoms in the obese population19. Another study evaluated the body fat percentage and linked OAB symptoms with excessive body fat percentage, results showed a 57.7% frequency of positive OAB symptoms in the extra body fat population category as compared to the reduced body fat population14. The importance of pelvic floor muscle exercise and liquid intake alterations in the identified resolution of OAB symptoms has been evaluated and assessed in many studies, and the importance of lifestyle changes and exercise on overactive bladder symptoms recorded an improvement in symptoms. As overactive bladder symptoms in young females who are studying and of childbearing age may affect mental health, and quality of life, reduce confidence and social interactions, create embarrassment, and in severe cases may harm the marital and sexual life of the patient. Many studies have been assessed the disturbance created by overactive bladder symptoms in the sexual and marital lives of females specifically in underdeveloped countries like Pakistan where treatment of females considered a financial burden. Psychological well-being is remarkably compromised with an increase in overactive bladder symptoms, females avoid going out of the house, not being able to find toilets in public places, and going to toilets in family gatherings make it embarrassing for patients to secure a confident attitude20-24.
Interventions for mild to moderate OAB symptoms are fewer as patients do not find it important to get health care advice, ignoring mild symptoms, knowledge of OAB and its treatment options are major reasons for increased incidences of severe OAB. Many health care providers indicate prevailing options of treatments such as Medications and surgery as patients present with progressed disease and the option of mild treatment options are usually gone. Unfortunately, many young females do not seek medical help or address these problems as a disorder or worth getting treatment for but suffer in silence until the condition worsens25. Delayed presentation requires invasive treatment options, awareness of overactive bladder symptoms and associated risk factors should be available for young females, and healthy habits such as exercise should be promoted to avoid excessive symptoms. This research indicates the value of lifestyle modification and mild exercises to maintain good bladder wall muscle strength and control lower urinary tract symptoms along with overactive bladder severity. Study participants have indicated complete oblivious to overactive bladder terminology and associated risk factor, although a major quantity of participants showed positive results upon initial; assessment of the OAB assessment tool.
Limitations of the study are less time for exercise, as a longer period of exercise and follow-up may indicate much better results. Hesitation to consult with a healthcare provider, understanding of which specialty is dealing with overactive bladder issues, and availability of non-invasive treatment options were marked as major reasons behind not seeking medical help for overactive bladder symptoms. A multi-center, larger sample size study is essential for a better understanding of the prevalence and risk factors assessment of OAB. Awareness of OAB and treatment options such as exercise and lifestyle modifications are required on a governmental level. A symptom assessment tool for the Asian young population is required to specify overactive bladder symptoms, this scale may help in clinical practices and research purposes, as inclusive assessment of medical treatment for OAB needs consistent and effective patient-based result assessments26. In the absence of objective clinical indicators, patient-reported outcomes signify the most applicable and significant method of assessing the impact of disease and its treatment27. Continuous awareness sessions are required on governmental levels to establish a better and more accurate understanding of problems related to overactive bladder and treatment options in the early stages. Appreciating behavioral therapies can be a significant initiative to eliminate the risk of progressed disease in young females.
Mild to moderate physical exercise including pelvic floor muscle exercise reduces the symptoms of overactive bladder, for example, increased frequency of urination and stress incontinence, lifestyle modifications represent positive effects too. To control bladder sphincter and OAB symptoms, exercises and lifestyle alterations are recommended along with consultation with the health care provider in extreme cases to avoid any social, psychological, sexual, and physiological difficulties.
The authors would like to thank the Suvastu School of Nursing and Health Sciences, Karachi for the facilitation and smooth conduction of the research.
The authors declared no conflict of interest.
Ethics approval was obtained from the Suvastu Nursing and Medical Institute, Karachi.
Informed consent was signed by all participants.
AZ did the manuscript writing and data entry. ST designed the objective and performed the data analysis. LR did the text proofreading and AB finally approved the manuscript after the critical evaluation.
- Bhide AA, Tailor V, Fernando R, Khullar V, Digesu GA. Posterior tibial nerve stimulation for overactive bladder—techniques and efficacy. Int Urogynecol J. 2020;31(5):865-870. doi: 10.1007/s00192-019-04186-3
- Rovner ES, Raymond K, Andruczyk E, Juul KV. Low‐dose desmopressin and tolterodine combination therapy for treating nocturia in women with overactive bladder: a double‐blind, randomized, controlled study. Low Urin Tract Symptoms. 2018;10(3):221-230. Doi: 10.1111/luts.12169
- Yeowell G, Smith P, Nazir J, Hakimi Z, Siddiqui E, Fatoye F. Real-world persistence and adherence to oral antimuscarinics and mirabegron in patients with overactive bladder (OAB): a systematic literature review. BMJ Open. 2018;8(11):1-8. doi: 10.1136/bmjopen-2018-021889
- Ganz ML, Smalarz AM, Krupski TL, Anger JT, Hu JC, Wittrup-Jensen KU, et al. Economic costs of overactive bladder in the United States. Urology. 2010;75(3):526-532. doi: 10.1016/j.urology.2009.06.096
- Booth J, Connelly L, Dickson S, Duncan F, Lawrence M. The effectiveness of transcutaneous tibial nerve stimulation (TTNS) for adults with overactive bladder syndrome: a systematic review. Neurourol Urodyn. 2018;37(2):528-541. doi: 10.1002/nau.23351
- Brown O, Siddique M, Mou T, Boniface ER, Volpe KA, Cichowski S. Disparity of racial/ethnic representation in publications contributing to overactive bladder diagnosis and treatment guidelines. Female Pelvic Med Reconstr Surg. 2021;27(9):541-546. doi: 10.1097/SPV.0000000000000992
- Chuang YC, Liu SP, Lee KS, Liao L, Wang J, Yoo TK, et al. Prevalence of overactive bladder in China, Taiwan and South Korea: Results from a cross‐sectional, population‐based study. Low Urin Tract Symptoms. 2019;11(1):48-55. doi: 10.1111/luts.12193
- Iyer S, Lozo S, Botros C, Wang C, Warren A, Sand P, et al. Cognitive changes in women starting anticholinergic medications for overactive bladder: a prospective study. Int Urogynecol J. 2020;31(12):2653-2660. doi: 10.1007/s00192-019-04140-3
- Kaaki B, Gupta D. Medium-term outcomes of sacral neuromodulation in patients with refractory overactive bladder: A retrospective single-institution study. PLoS One. 2020;15(7):1-11. doi: 10.1371/journal.pone.0235961
- Lightner DJ, Gomelsky A, Souter L, Vasavada SP. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: AUA/SUFU guideline amendment 2019. J Urol. 2019;202(3):558-563. doi: 10.1097/JU.0000000000000309
- Khullar V, Sexton CC, Thompson CL, Milsom I, Bitoun CE, Coyne KS. The relationship between BMI and urinary incontinence subgroups: results from EpiLUTS. Neurourol Urodyn. 2014;33(4):392-399. doi: 10.1002/nau.22428
- Wang SG, Yang SS, Chang SJ. Association between obesity and lower urinary tract symptoms among children and adolescents: A community-based study. Front Pediatr. 2021;9:1-7. doi: 3389/fped.2021.609057
- Pomian A, Lisik W, Kosieradzki M, Barcz E. Obesity and pelvic floor disorders: a review of the literature. Med Sci Monit. 2016; 22: 1880-1886. doi: 10.12659/MSM.896331
- Hagovska M, Švihra J, Buková A, Dračková D, Horbacz A. The impact of different intensities of exercise on body weight reduction and overactive bladder symptoms-randomised trial. Eur J Obstet Gynecol Reprod Biol. 2019;242:144-149. doi: 10.1016/j.ejogrb.2019.09.027
- Hagovska M, Švihra J, Buková A, Dračková D, Horbacz A, Nagyová I. Effect of an exercise programme for reducing abdominal fat on overactive bladder symptoms in young overweight women. Int Urogynecol J. 2020;31(5):895-902. doi: 10.1007/s00192-019-04157-8
- Homma Y, Kakizaki H, Yamaguchi O, Yamanishi T, Nishizawa O, Yokoyama O, et al. Assessment of overactive bladder symptoms: comparison of 3-day bladder diary and the overactive bladder symptoms score. Urology. 2011;77(1):60-64. doi: 10.1016/j.urology.2010.06.044
- Hung MJ, Chou CL, Yen TW, Chuang YC, Meng E, Huang ST, et al. Development and validation of the Chinese Overactive Bladder Symptom Score for assessing overactive bladder syndrome in a RESORT study. J Formos Med Assoc. 2013;112(5):276-282. doi: 10.1016/j.jfma.2011.09.020
- Van der Vaart CH, De Leeuw JR, Roovers JP, Heintz AP. The effect of urinary incontinence and overactive bladder symptoms on quality of life in young women. BJU Int. 2002;90(6):544-549. doi: 10.1046/j.1464-410X.2002.02963.x
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291(23):2847-2850. doi:10.1001/jama.291.23.2847
- Vispute SS, Smith JD, LeCheminant JD, Hurley KS. The effect of abdominal exercise on abdominal fat. J Strength Cond Res. 2011;25(9):2559-2564. doi: 10.1519/JSC.0b013e3181fb4a46
- Spettel S, Frawley HC, Blais DR, De E. Biofeedback treatment for overactive bladder. Curr Bladder Dysfunct Rep. 2012;7(1):7-13. doi: 10.1007/s11884-011-0117-4
- Andrade AD, Anam R, Karanam C, Downey P, Ruiz JG. An overactive bladder online self-management program with embedded avatars: a randomized controlled trial of efficacy. Urology. 2015;85(3):561-567. doi: 10.1016/j.urology.2014.11.017
- Reisch R. Interventions for overactive bladder: review of pelvic floor muscle training and urgency control strategies. J Womens Health Phys Therap. 2020;44(1):19-25. doi: 10.1097/JWH.0000000000000148
- Rashid S, Babur MN, Khan RR, Khalid MU, Mansha H, Riaz S. Prevalence and associated risk factors among patients with overactive bladder syndrome in Pakistan. Pak J Med Sci. 2021; 37(4): 1185-1189. doi: 10.12669/pjms.37.4.4262
- Bo K, Fernandes AC, Duarte TB, Brito LG, Ferreira CH. Is pelvic floor muscle training effective for symptoms of overactive bladder in women? A systematic review. Physiotherapy. 2020;106:65-76. doi: 10.1016/j.physio.2019.08.011
- Kelleher C, Chapple C, Johnson N, Payne C, Homma Y, Hakimi Z, et al. Development of an overactive bladder assessment tool (BAT): a potential improvement to the standard bladder diary. Neurourol Urodyn. 2018;37(5):1701-1710. doi: 10.1002/nau.23479
- Raju R, Linder BJ. Evaluation and treatment of overactive bladder in women. Mayo Clin Proc. 2020; 95(2):370-377. doi: 10.1016/j.mayocp.2019.11.024
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
