By Naseem Munshi1, Badaruddin Sahito2, Muhammad Khalid Arain3, Sobia Aziz4, Remsha Sattar4
AFFLIATIONS:
- Ziauddin Medical University, Karachi, Pakistan.
- Civil Hospital Karachi, Karachi, Pakistan.
- National Medical Centre, Karachi, Pakistan.
- Ziauddin Hospital (North Campus), Karachi, Pakistan.
Background: Osteoarthritis involves degeneration of articular cartilage seen with increasing age. The knee joint, the most common joint that falls prey to attacks of osteoarthritis, has 30% incidence in population above 60 years. Total knee arthroplasty (TKA) is the main surgical option for orthopaedics. Though it corrects the deformity and relieves pain, yet it is not the treatment of choice in younger population. This study aimed to validate the effects of proximal fibular osteotomy (PFO) as a newer technique in managing medial compartment knee osteoarthritis.
Methods: The diagnosed patients for medial compartment knee joint osteoarthritis were selected for study from Dr. Ziauddin University hospital of Karachi. Excluded were aged less than 40 years, or with BMI more than 30, and patients with tri-compartmental arthritis. Medial and lateral joint spaces along with Oxford knee score were measured and recorded pre- and post-operatively. Patients underwent PFO after giving written and informed consent.
Results: Total number of patients selected was 30 for this study; 21 (70%) females, and 9 (30%) males (mean age 58.8 years). Mean pre-operative measured medial joint space on standard antero-posterior (AP) radiograph was 0.442± 0.04 cm. Mean recorded pre-operative Oxford knee score was 23.87±3.74 mm. Improvement was observed in mean postoperative medial joint space to 0.572± 0 .066 cm and mean post-operative Oxford knee score to 40.2±5.8mm.
Conclusion: This study concludes that PFO significantly improves joint function in patients with medial compartment osteoarthritis knee and may delay the need for total knee arthroplasty, if carried out at an appropriate stage.
Keywords: Osteotomy; Osteoarthritis; Total Knee Arthroplasty.
Osteoarthritis involves degeneration of articular cartilage seen with increased age1. The knee joint is one of the most common joints that falls prey to attacks of osteoarthritis, with 30% incidence in population above 60 years, in which knee varus deformities are consistent findings in patients diagnosed with knee Osteoarthritis (OA) 2,3. It occurs most commonly in the medial compartment of the knee since it bears 60 to 80% of the load because the axis is typically medially deviated4.
The causes are multifactorial with increased risk with age, race, body mass index (BMI) and sedentary lifestyle1,5-7. It can be source of severe pain and immobility amongst the patients which can also affect the quality of life. This, in turn, is an indication of surgery. Previously, Total Knee Arthroplasty (TKA) was the main surgical option for orthopaedic surgeons. Though it provides pain relief and correction of deformity still it is not the preferred treatment of choice in younger population8. Another alternative to TKA is uni-compartment knee arthroplasty. This procedure is associated with a short recovery period by decreasing complications. However, it is also linked to higher reoperation rates9. Another preferred technique especially amongst young patients is High Tibial Osteotomy (HTO) 10. HTO can be a technically challenging procedure with certain complications, which include neuro-vascular injury, iatrogenic fracture, and non-union11. Furthermore, these patients may eventually require a revision to TKA12-13.
Thus, an innovative treatment has emerged namely Proximal Fibular Osteotomy (PFO) 14. This procedure is relatively safer, simpler, and cost-effective procedure compared to other frequently done procedures. With significant improvement in post-operative ambulation, improved lower limb alignment in some patients with severe varus knee, this procedure may in turn replace the need for TKA especially in patients with severe co morbidities15,16. In order to evaluate the short-term effects of this procedure on joint function and quality of life in patients, this study was designed to validate the effects of proximal fibular osteotomy as a newer technique in managing medial compartment knee osteoarthritis.
The present case series was conducted at Dr. Ziauddin Medical Hospital of Karachi from March 2015 to March 2017. Inclusion criteria included patients with medial compartment knee joint OA with an indication of surgery, who were over 40 years old and BMI<30. We also included patients with failed conservative management and hence were a good candidate for surgery. However, patients with inflammatory joint disease, deformity of the valgus knee, bi-compartmental or tri-compartmental osteoarthritis, morbid obesity, or having knee joint infectious pathology were not included.
Ethical review board approval was obtained for the study. All patients included were evaluated clinically and radiologically. A weight-bearing X-ray in antero-posterior (AP) and lateral views was done of the diseased knee. Similarly, pre- and post-operatively joint spaces (medial and lateral) were measured and recorded. Pre- and post-operative values of Oxford knee score were recorded at monthly intervals (12 question analysis) 17. Proximal fibular osteotomy (PFO) was done after receiving written, informed consent, and anaesthesia fitness for the procedure.
Surgical procedure entails placing patient in a supine position following administration of spinal anaesthesia. Pre-operative intravenous antibiotic prophylaxis was given during induction of anaesthesia. A tourniquet was placed on the thigh and standard prep and draping was done. A small buttress was fixed to the operating table, supporting the heel in 90° knee flexion. The fibular head was identified and marked, before the incision was given, to avoid potential damage to the common peroneal nerve as well as to the soft tissue structures attachments of tibia, which are crossing the knee joint. At the level of proximal third of fibula, a single lateral incision of 3cm-5cm was made. In between the peroneus and soleus muscles fascia was then incised along the septum. The fibula was exposed by separating the muscles. A 2cm-3cm section of the fibula was detached 6 to 10 cm below the caput fibulae by using an oscillating saw followed by osteotome. Following the removal of fibular segment, ends of the fibula from where the segment was removed, were sealed with bone wax. A generous volume of normal saline was used for the irrigation of surgical wound, muscles, fascia, and skin were then sutured in layers. Aseptic dressing was done. Data was analysed using IBM SPSS Statistics for Windows, Version 23.0. (IBM Corp., Armonk, NY). Paired t test was applied and p value less than 0.05 was considered statistically significant.
Thirty patients with mean age of 58.81 years (range 54 to 63 years), were included in this study. Twenty-one (70%) were females including17 (81%) in the range of 54-60 years, whereas, 4 (19%) in the range of 61-65 years. There were 9 (30%) males in which 6 (66.6) were in the range of 54-60 years, whereas 3 (33.4%) were in the range of 61-65 years. Significant pain alleviation and improved joint function was observed in all the patients using the oxford knee scoring system with an average increase of 20-25 points (compared to pre-operative evaluation) at 2 years of follow up post operatively (Table 1).
Table 1: Oxford Knee score of patients undergoing Proximal Fibular Osteotomy (PFO).
| Variables | Mean ± SD/Frequency | p-Value |
| Age | 58.81± 2.81 | |
| Male | 9 | |
| Female | 21 | |
| Medial Joint Space
Pre-operative Post-operative |
0.44±0.02 0.57±0.02 |
<0.0001* |
| Oxford Knee Score
Pre-operative Post-operative |
24.00±3.63
40.57±1.59 |
<0.0001* |
*Significant at p<0.05
Likewise, weight bearing lower limb X-rays confirmed an increase in the medial knee joint space from 0.44±0.02 pre-operatively to 0.57±0.02 post-operatively with significant p-value of <0.0001 (Figure 1 and 2). There was an increase in the Oxford knee score from 24.00±3.63 pre-operatively to 40.57±1.59 post-operatively with significant p-value of <0.0001 (Table 2).
Table 2: Pre and post values regarding age and gender of patients according to Medial joint space and Oxford Knee.
| Gender | n | Age | Medial Joint Space | p-Value | Oxford Knee Score | p-Value | ||
| Pre-op
Mean±SD |
Post-op
Mean±SD |
Pre-op
Mean±SD |
Post-op
Mean±SD |
|||||
| Male (n=9) | 6 | 54 – 60 | 0.44 ±0.02 | 0.60±0.02 | <0.0001* | 24.33±3.61 | 40.17 ±0.75 | <0.0001* |
| 3 | 61 – 65 | 0.43±0.03 | 0.55 ±0.05 | 0.003* | 22.57±3.81 | 39.85 ±5.81 | 0.055 | |
| Female
(n=21) |
17 | 54 – 60 | 0.45±0.02 | 0.58 ±0.02 | <0.0001* | 23.94 ±373 | 41.06 ±1.85 | <0.0001* |
| 4 | 61 – 65 | 0.44 ±0.02 | 0.55 ±0.01 | 0.004* | 24.75±1.26 | 39.75 ±0.96 | <0.0001* | |
*Significant at p<0.05

Figure 1: Visible improvement in the medial compartment of joint space after the procedure i.e., Proximal Fibular Osteotomy (PFO): (a) Pre-operative, (b) Post-operative.
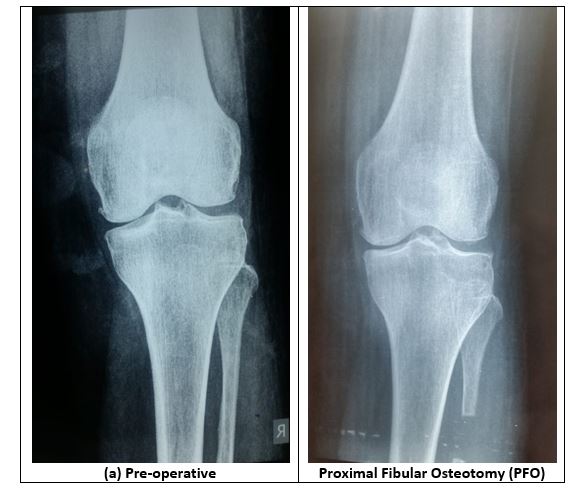
Figure 2: Visible improvement in the medial compartment of joint space after the procedure i.e., Proximal Fibular Osteotomy (PFO): (a) Pre-operative, Proximal Fibular Osteotomy.
Significant pain alleviation and improved joint function was observed in all the patients using the oxford knee scoring system with an average increase of 20-25 points (compared to pre-operative evaluation) at 2 years of follow up post operatively. Likewise, weight bearing lower limb X-rays confirmed an increase in the medial knee joint space from 0.44±0.02 pre-operatively to 0.57±0.02 post-operatively with significant p-value of <0.0001. There was an increase in the Oxford knee score from 24.00±3.63 pre-operatively to 40.57±1.59 post-operatively with significant p-value of <0.0001.
Osteoarthritis of the knee is one of the leading causes of disability in older patients. There are multiple options available for the knee joint Osteoarthritis (OA) management, including both conservative and surgical options. Conservative options include analgesics, physical therapy, intra-articular injections of steroid or platelet-rich plasma, and viscosupplementation agents whereas; surgical options include high tibial osteotomy (HTO), autologous chondrocyte implantation, arthroscopic lavage, and total knee arthroplasty (TKA).
With time, High Tibial Osteotomy (HTO) was discovered to be an effective treatment option for osteoarthritis of the medial compartment of the knee joint18,19. This was accompanied with prolonged recovery, and increased risks of non-union or delayed union, peroneal nerve paralysis and wound infection20.
The advent of a novel treatment option for medial compartment osteoarthritis of the knee joint, PFO, has helped a lot in the field of orthopaedics and traumatology. Modernization necessitates orthopaedic surgeons to get past through the traditional rules and use critical thinking. In clinical practice, there is emphasis on discovering the new methods of previously existing procedures. The pilot study of using PFO for management of patients with medial compartment knee osteoarthritis (OA) is an excellent example14.
Younger patients have a longer life expectancy and are more active, their post-operative demands are considerably higher than older patients are. Therefore, a procedure is essential which is cost effective, easy to execute, gives better functional results, requires a shorter recovery time, and provides the affected patients a good quality of life21.
The theory behind the cause of medial compartment OA is an uneven distribution of weight across both tibial plateaus with more stress transmitted on the medial side. As there is rise in grading of knee OA, femoral neck-shaft valgus angle decreases and there is increased bowing of the femoral shaft laterally, thereby, decreasing the condylar shaft angle22. The mechanical axis shifts medially on the femoral side, looking towards the tibial side, tibial plateau compression leads to the medial plateau becoming steep, greater than bowing of the tibia. Bowing of the tibia ensues from moderate grade of knee OA that in turn causes progression of medial knee OA more because of medial tibial compression23. PFO acts by eliminating the tri-cortical support laterally and shifting the stress from the medial to the lateral compartment with subsequent relief of pain, which in turn provides a good functional outcome20-22.
In 2015, Zhang reported that PFO decreases pain and improves function of knee joint in osteoarthritis14. Compared to HTO, it is less commonly associated with major complications which include infection, deep vein thrombosis (DVT), insufficient correction, intra-articular fractures, peroneal nerve injury, compartment syndrome, and knee stiffness23,24. In addition to this, HTO requires prolonged period of non-weight bearing walking until union of osteotomy site. Furthermore, PFO unlike other treatment options has no requirement of insertion of supplementary implants. All these advantages make PFO an ideal treatment option in most developing countries like Pakistan that lack financial and health resources20.
PFO leads to a declined lateral fibular support and ultimately the rectification of the varus deformity, which helps shifting the loading force from medial compartment more laterally. This alleviates the pain and provides significant regain of function24. PFO done at the level of about 4-7 cm distal to fibular head decreases the risk of injury to peroneal nerve, favouring PFO over HTO. Mean Oxford Knee Score (OKS) increased by 20-25 points (as compared to pre-operative evaluation) at 2 years of follow-up postoperatively. Likewise, VAS scores decreased significantly as well from severe to mild. In our settings, patients were mobilized on the same day. And hence it was found to have significant improvement of quality of life in our patient population23,24.
Despite PFO being a simple procedure, it too has some pitfalls. During the procedure, potential injury to the peroneal nerve should be avoided. In this study, 4 (3.6%) patients complained of numbness in the ipsilateral lower leg due to common peroneal nerve injury (n=2) and superficial peroneal nerve (n=2). Due to this, it is recommended to take a postero-lateral approach during the procedure via space between the peroneus longus, brevis and soleus muscle to reduce the risk of iatrogenic nerve injury at a level of 6 cm before the fibular bed25.
PFO is a relatively newer technique hence; there is a paucity of data in the literature on its effectiveness. A well performed fibular osteotomy (in terms of accurate height from the fibular head, the length of the fibular chunk removed, and peroneal nerve protection) is essential for a good outcome26,27. Although, PFO was found to be an effective technique in our patient population, we need a relatively larger sample size and longer follow up period in order to assess the effectiveness in the treatment of medial compartment osteoarthritis.
Significant pain alleviation and improved joint function was observed in all the patients using the oxford knee scoring system with an average increase of 20-25 points (as compared to pre-operative evaluation) at 2 years of follow up post operatively. Likewise, weight bearing lower limb X-rays confirmed an increase in the medial knee joint space. There was an increase in the Oxford knee score. Hence, this study demonstrates that the novel procedure, proximal fibular osteotomy (PFO) is a safe and simple intervention that significantly improves joint function in medial compartment osteoarthritis knee, providing early ambulation, which delays the need for total knee arthroplasty.
The authors wish to show appreciation to the hospital staff and doctors for their kind help and co-operation throughout this period.
The authors declare that there is no conflict of interest.
Ethics approval was obtained from the Ethical Review Board of the institution.
All the participants included in this study submitted the written and informed consents.
NM, BS and MKA designed the study and performed the mentioned surgeries. NM and RS collected the data and performed the analysis. RS also assisted in this and performed the data analysis and interpretation. NM and RS also helped in this process. SA and RS performed writing and editing. All authors reviewed the results and approved the final version of the manuscript.
- Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM. Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Care Res. 1995;38(8):1134-1141.
- Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Care Res. 1987;30(8):914-918.
- Huda N, Islam MS, Kumar H, Pant A, Bishnoi S. Proximal fibular osteotomy for medial compartment knee osteoarthritis: is it worth? Indian J Orthop. 2020;54:47-51.
- Shanmugasundaram S, Kambhampati SB, Saseendar S. Proximal fibular osteotomy in the treatment of medial osteoarthritis of the knee–A narrative review of literature. Knee Surg Relat Res. 2019;31(1):1-7.
- Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26(3):355-369.
- Vincent KR, Conrad BP, Fregly BJ, Vincent HK. The pathophysiology of osteoarthritis: a mechanical perspective on the knee joint. PM R. 2012;4(5):S3-S9.
- Subash Y, Naidu GK, Subash DY, Naidu DG. The role of proximal fibular osteotomy in the management of medial compartment osteoarthritis of the knee. Int J Orthop Sci. 2018;4:369-372.
- Schnurr C, Jarrous M, Güdden I, Eysel P, König DP. Pre-operative arthritis severity as a predictor for total knee arthroplasty patients’ satisfaction. Int Orthop. 2013;37(7):1257-1261.
- Wilson HA, Middleton R, Abram SG, Smith S, Alvand A, Jackson WF, et al. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis. BMJ. 2019;364:1-17.
- LaPrade RF, Spiridonov SI, Nystrom LM, Jansson KS. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy. 2012;28(3):354-364.
- Sprenger TR, Doerzbacher JF. Tibial osteotomy for the treatment of varus gonarthrosis: survival and failure analysis to twenty-two years. J Bone J Surg. 2003;85(3):469-474.
- Seo SS, Nha KW, Kim TY, Shin YS. Survival of total knee arthroplasty after high tibial osteotomy versus primary total knee arthroplasty: a meta-analysis. Medicine. 2019;98(30):1-9.
- Rai AK, Saurabh A, Shekhar S, Kunwar A, Verma V. Proximal fibular osteotomy for pain relief and functional improvement in patients of osteoarthritis of knee. Int Surg J. 2019;6(7):2368-2372.
- Zhang YZ. Innovations in orthopedics and traumatology in China. Chin Med J. 2015; 128(21): 2841-2842.
- Wang X, Wei L, Lv Z, Zhao B, Duan Z, Wu W, et al. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res. 2017;45(1):282-289.
- Utomo DN, Mahyudin F, Wijaya AM, Widhiyanto L. Proximal fibula osteotomy as an alternative to TKA and HTO in late-stage varus type of knee osteoarthritis. J Orthop. 2018;15(3):858-861.
- Oxford Knee Score [Internet]. Oxford Knee Score – Orthopaedic Scores 2021 [cited 2020 Dec 6]. Available from: http://www.orthopaedicscore.com/scorepages/oxford_knee_score.html
- Mont MA, Alexander N, Krackow KA, Hungerford DS. Total knee arthroplasty after failed high tibial osteotomy. Orthop Clin North Am. 1994;25(3):515-525.
- Qin D, Chen W, Wang J, Lv H, Ma W, Dong T, et al. Mechanism and influencing factors of proximal fibular osteotomy for treatment of medial compartment knee osteoarthritis: a prospective study. J Int Med Res. 2018;46(8):3114-3123.
- W-Dahl A, Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients: a Swedish Register Study. Acta Orthop. 2010;81(2):161-164.
- Sukumaran S, Ashokan C, Nagendran K, Kathirazhagan S. Is proximal fibular osteotomy a boon or bane for medial compartment osteoarthritis? Our experience. Int J Orthop Sci. 2019;5(2):1001-1004.
- Misra RK, Batra AV. Clinical and functional outcomes of proximal fibular osteotomy on varus deformity and medial compartment knee osteoarthritis. J Arthritis. 2019;8(3):1-4.
- Giagounidis EM, Sell S. High tibial osteotomy: factors influencing the duration of satisfactory function. Archives of orthopaedic and trauma surgery. 1999;119(7-8):445-449.
- Harshwardhan H, Laddha GK, Gupta P. Outcome assesment of proximal fibular osteotomy in medial compartment knee osteoarthritis. Int J Orthop Sci. 2020;6:183-185.
- Yang ZY, Chen W, Li CX, Wang J, Shao DC, Hou ZY, et al. Medial compartment decompression by fibular osteotomy to treat medial compartment knee osteoarthritis: a pilot study. Orthopedics. 2015;38(12):1-5.
- Ahmed M, Bux M, Kumar M, Ahmed N, Hussain G, Ishtiyaque Sr M. Proximal fibular osteotomy in the management of osteoarthritis of medial compartment of knee joint. Cureus. 2020;12(6):1-6.
- Matsumoto T, Hashimura M, Takayama K, Ishida K, Kawakami Y, Matsuzaki T, et al. A radiographic analysis of alignment of the lower extremities–initiation and progression of varus-type knee osteoarthritis. Osteoarthritis Cartilage. 2015;23(2):217-223.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
