By Shahbaz Khan Panhwar, Saddam Mazar, Imtiaz Hashmi, Muhammad Sohail Rafi, Nida Hameed
AFFILIATIONS:
- Department of Orthopedics and Spine Surgery, Dr. Ziauddin University Hospital, Karachi, Pakistan.
Background: Prolapse lumbar intervertebral disc (PLID) is a localized disc displacement outside its margins is the most common source of sciatica pain, involving 1%-5% of the population annually. Standard management includes conservative management initially for a period of around 6 weeks. In general, microdiscectomy (MD) is considered a standard procedure for symptomatic cases, with approximately 60%-80% of satisfactory results. In this study, we aimed in describing experience of MD in patients diagnosed with PLID.
Methods: This retrospective study has been conducted at Dr. Ziauddin University hospital, Karachi; Pakistan. The medical records from 2018 to 2020, of microdiscectomy for prolapsed intervertebral lumbar disc were studied. All patients of 18 years or more admitted with symptomatic PLID, and proceeded to single level MD have been included. The regular pre-operative work-up, surgical technique and post-operative management was followed. Data collection was performed using a standard proforma. Utilizing SPSS version 23.0, all statistical analyses were carried out a p <0.05 was considered statistically significant.
Results: Mean age of patients was 43 to 42 years and Male: Female ratio was 1.6:1 and pre-operative neurological deficit was observed in 28 (42.4%) patients. Most common affected disc spaces were L4-L5 35(53%) and L5-S1 26 (39.4%). Left side disc Prolapse was found more affected as 39(59.1%) cases reported among the total. Visual analog scale (VAS) score dropped from more than 5 to no pain after surgery.
Conclusion: Microdiscectomy is a safe treatment in prolapsed intervertebral lumbar disc for patients with failed conservative therapy and reported excellent outcomes with earlier surgical intervention.
Keywords: Discectomy; Intervertebral Disc Displacement; Radiculopathy.
Prolapsed Lumbar Intervertebral Disc (PLID) is defined as a localized disc material displacement outside the normal margins of intervertebral disc space1 and is frequent source of sciatic pain, affecting 1% to 5% of the population per year with prevalence of 4.8% among men over 35 years of age and 2.5% among women over this age2. Clinical examination of patient correlating with Magnetic resonance imaging (MRI) findings should be basis for diagnosis of PLID2.
Pathogenesis of sciatica pain is often multifactorial, involving stimulation of nerve endings of annulus fibrosus, direct compression of nerve roots (with or without ischemia) and sequence of inflammatory cascade triggered by extruded nucleus3. Until and unless the disc is contained, there is minimal inflammatory cell infiltration but as soon as disc becomes non-contained (extruded) there is influx of inflammatory cells due to rupture of posterior longitudinal ligament exposing disc to epidural vascular space causing release of inflammatory mediators which irritate the nerve by chemical toxicity and cause sciatic pain3. Subsequently, until and unless there is contained disc, pain is caused by mechanical compression while in non-contained it is due to inflammatory mediators causing chemical irritation of nerve root along with mechanical compression. Standard protocol of PLID management involves an initial effort at conservative therapy for a minimum of six weeks, comprising of bed rest, physiotherapy, non-steroidal anti-inflammatory drug (NSAID’s) and pregabalin with some role of corticosteroids to reduce inflammation especially if tried using single shot transforaminal epidural injection3,4.
If conservative management is not eminent in achieving the required positive outcomes as reflected with pain relief and improvement in patient reported outcomes, or if the patient presents with the neurologic deficit, e.g., foot drop4,5. Then surgical intervention is proceeded which comprises of open lumbar discectomy, microdiscectomy (conventional) or microscopic and endoscopic discectomy from most invasive to minimally invasive approaches6,7.
There has been a lot of debate over the last few years about the balance of benefits between early surgery and extended conservative treatment, having said that early surgery gives better outcomes with reference to recovery of neurological deficit and pain as patient-reported outcome measures (PROMs) 3,8. MD is often thought-about a common operation to remove the herniated part of a disc that puts pressure on a nerve. It has a long history and many spine surgeons have intensive experience9,10. In 60-80 percent of patients, satisfactory outcomes have been reported after lumbar discectomy especially in relation to radiculopathy11. In this study, we aimed at describing our experience of MD in patients diagnosed with PLID in relation to level affected, laterality, clinical and imaging findings and patient reported outcomes.
This retrospective study was conducted at Dr. Ziauddin University Hospital, Karachi, Pakistan. The medical records of patients on whom Microdiscectomy (MD) for lumbar disc herniation was performed, were studied from 2018 to 2020. All patients of 18 years or more were admitted with medical findings of symptomatic lumbosacral disc herniation, and proceeded to single level MD have been included.
All patients were administered general anesthesia for these surgeries. Patients were placed on an operation table in a knee-chest position. Chest, knee and pelvic cushions were placed, with hips and knees flexed to provide maximum reduction of lumbar lordosis and increase interlaminar space. Patient is secured with 2-3 belts around the chest, abdomen and pelvic regions. Aseptic measures were carried out and all patients underwent hand scrub with Pyodine Scrub, for at least 5 minutes. Disposable drappings were placed in aseptic measures with operative site sealed with Ioban®.
At this stage, a 25G needle between the required level spinous processes was utilized to confirm the level, under fluoroscopy. A midline skin incision of 2 to 4 cm was utilized for the procedure. It was given between the spinous processes, above and below the marked level. Fascia was incised followed by sub- periosteal dissection exposing lamina of the superior and inferior levels and laterally till facet joint. All sequestered/extruded disc material pieces were removed. Ligamentum flavum was incised using blade #11 medially, and it is cut cautiously in layers till the change in its color was observed. Flavum was removed using Kerrison Rongeur, and space was widened to appropriate size. Appropriately sized laminotomies were performed to get access to the disc space and to avoid excessive nerve root retraction. After retraction of the thecal sac and nerve root, the annulus was opened with a small cruciate incision. Pituitary rongeur was then passed through this incision and disc was removed. It was performed by multiple insertions in attempt to remove the disc. Hemostasis secured by coagulating epidural vessels and standard closure was performed.
All the patients with a history of previous lumbar spine surgery, multiple level PLID, concomitant spinal stenosis and patients with surgical spinal fusion were disqualified from study.
Structured proforma was employed to tabulate information on patient demographics, presenting clinical manifestations, physical examination, MRI findings, details of non-surgical treatment, side and level affected, presence of Modic changes were observed, and presence of sphincter incontinence was recorded.
Utilizing SPSS version 23.0, for Windows operating system, statistical analyses were carried out. The data collected in the pre-coded form was entered. Continuous variables were expressed as mean +/- (SD). Chi-square testing and Fischer’s exact tests, as appropriate, were employed for comparison of categorical variables. A statistically important p-value <0.05 for all tests was considered statistically significant.
Sixty-six patients fulfilled our inclusion criteria. The calculated mean age of patients was 43.42 years and M: F ratio of 1.6:1 was calculated. Mean duration of surgery was 40 minutes (range 20-60 minutes) and average blood loss was 10 ml (range 10-40 ml). Pre-operative neurological evaluation revealed that 28 (42.4%) patients presented with some neurological deficit while 38 (57.6%) had no deficit. Sphincter incontinence was present in 3(4.5%) of cases while 63(95.5%) had no sphincter problem (Table 1).
Table 1: Descriptive statistics for different variables of the study.
| Variables | Parameters | n(%) | Mean± Standard Deviation | p-Value |
|
Gender |
Male | 43(65.2) | – | |
| Female | 23(34.8) | |||
|
Side of Disc Herniation |
Right | 27(40.9) | 1.59 ±.495 | <0.05 |
| Left | 39(59.1) | |||
|
Level of Disc Herniation |
L2-L3 | 3(4.5) | – |
<0.05 |
| L3-L4 | 2(3.0) | |||
| L4-L5 | 35(53.0) | |||
| L5-S1 | 26(39.4) | |||
|
Laterality of Herniated Disc |
Paracentral | 19(28.8) | 2.23±.973 | <0.05 |
| Axillary | 19(28.8) | |||
| Central | 22(33.3) | |||
| Foraminal | 6(9.1) | |||
| Modic Degenerative Changes | Present | 16(24.2) |
1.76±.432 |
<0.05 |
| Absent | 50(75.8) | |||
|
Cranial-Caudal Migration |
Cranial | 5(7.6) | 2.55±.637 | <0.05 |
| Caudal | 20(30.3) | |||
| No migration | 41(62.1) | |||
|
Visual Analogue Scale Leg Pain |
5-6 = severe pain | 19(28.8) | 4.05±.793 | <0.05 |
| 7-8 = very severe | 25(37.9) | |||
| 9-10 = worst pain possible | 22(33.3) | |||
|
Neurological Deficit |
Present | 28(42.4) | 1.58±.498 | <0.05 |
| Absent | 38(57.6) | |||
| Urinary-Fecal Incontinence | Present | 3(4.5) | 1.95±.210 | <0.05 |
| Absent | 63(95.5) | |||
| Early Onset Post-Op Sciatica | Present | 6(9.1) | 1.91±.290 | <0.05 |
| Absent | 60(90.9) | |||
The level of disc prolapse was confirmed on MRI scan. Most commonly affected disc spaced were L4-L5 (35 cases, 53%), L5-S1 (26 cases, 39.4%), L2-L3 (3 cases, 4.5%) and L3-L4 (2 cases, 3.0%). In relations to the radiculopathy and MRI correlated findings Right sided disc prolapse was present in 27(40.9%) while left side was involved in 39(59.1%) of cases. Central disc protrusion was present in 22(33.3%) followed by paracentral (19, 28.8%) and axillary type (19, 28.8%). Cranial migration was found in 5(7.5%) of cases while caudal migration of disc was present in 20 (30.3%) of cases and no migration in 41(62.1%) of cases. Modic changes were present in 16(24.2%) and normal end plates in 50(75.8%) cases. Most of our patients had VAS score >5 at the time of presentation which dropped to no pain after surgery except for 6 patients (9.1%), who developed same radicular pain which was relieved on per oral steroids (prednisolone 15mg TDS 3-4 days, and pregabalin 75mg BD).
In addition, the results indicated the higher pain scale (43) for males when compared with the pain scale (23) for females as shown in Figure 1.
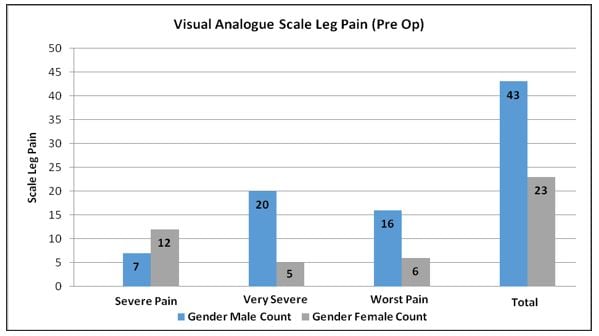
Figure 1: Comparative pain scales between males and females in pre-operative phase.
Significant association was found between gender and visual analogue scale leg pain with p=0.008. However, no significant association was found (Table 2) among early onset post-op sciatica, urinary-fecal incontinence, cranial-caudal migration, level of disc herniation with gender (p= 0.656, 0.276, 0.060, 0.976 respectively).
Table 2: Comparison of gender with clinical parameters.
| Variables | Clinical Parameters | Male | Female | p-Value | |
|
Visual Analogue Scale Leg Pain |
Severe pain | 7 | 12 | *0.008 | |
| Very severe | 20 | 5 | |||
| Worst pain possible | 16 | 6 | |||
| Early Onset Post-Op Sciatica | Early post-op sciatica present | 5 | 1 | 0.656 | |
| Absent early post-op sciatica | 38 | 22 | |||
| Urinary-Fecal Incontinence | |||||
| Incontinence present | 1 | 2 | 0.276 | ||
| Incontinence absent | 42 | 21 | |||
| Cranial-Caudal Migration | Cranial | 3 | 2 | 0.060 | |
| Caudal | 9 | 11 | |||
| No migration | 31 | 10 | |||
| Level of Disc Herniation | L2-L3 | 2 | 1 | 0.976 | |
| L3-4 | 1 | 1 | |||
| L4-5 | 23 | 9 | |||
| L5-S1 | 17 | 12 |
Chi-squared and Fisher’s exact test was used for comparison and * p value = 0.05 considered as significant.
In this study, we seek to highlight our experience with MD in patients diagnosed with PLID in relation to the level affected, laterality, clinical and imaging findings, and the outcomes reported by the patient. Our study demonstrated that most of the patients presented initially with a VAS score >5 that decreased to no pain after surgery and left side PLID was involved in 39(59.1%) of cases more than right side. The specific event leading to a herniated disc remains unknown. The first-line care for most patients with lumbar disc herniation should be non-operative therapy12. The benchmark management remains to be the operative care13. Compared to conservative treatment, surgery is shown to offer substantially quicker pain relief, although the effect disappears after a year.
In terms of pain management and neurological improvement, there is no treatment modality that is superior to the rest, nor is there a surgical procedure specifically superior to simple discectomy14. There is no room for percutaneous care practices in these situations; treatment is surgical intervention15. With the exception of these emergency cases, effective management is recommended for at least six weeks in the event of ineffectiveness of comprehensive medical treatment. The purpose is the treatment of radicular pain; there is an uncertain outcome on the associated low back pain. Patient selection is very critical in the context of this functional surgery15.
Microdiscectomy (MD) was first published by Yasargil 1977 is considered a gold standard management in Prolapsed Intervertebral Disc (PID)6. Katayama et al. compared the results of open conventional discectomy versus MD and concluded no difference between surgical outcomes however; MD gave higher magnification and decreased incision length and tissue stripping7. In MD, there was decreased use of opioids and return to Activity of Daily Life (ADL) was earlier. The reasonably successful outcome range (75-80 percent) has been reported to represent a precise and reasonable target for both spine surgeons and medical economists following PLID surgical intervention 16.
The prevalence of lumbar disc herniation in magnetic resonance imaging (MRI) studies is 30 percent, only 1-2 percent of individuals are clinically affected during their lives. In males and during the fourth and fifth decades of life, symptomatic lumbar disc herniation is more common17. The affected age group in our study mainly was found to be between30 to 45 years, the most of which being bread earners for their families in our society. The incidence is highest at L4-L5 and L5-S1 levels in 90 percent of the cases8, whereas we observed in 92.4% of cases that is comparable to study done by Akbar and Mahar9, where it is 86.4% of cases. This may be due to lumbar spine anatomy, because extraforaminal space in the upper segment of lumbar spine is proportionally larger compared to the lower lumbar levels, other contributing factors to disc herniation encase increased range of mobility of lower segments leading to disc degeneration and prolapse earlier18. It is seen that left sided disc prolapse is more common than right side disc prolapses (59.1% vs. 40.9%).
Several techniques reported to be better for shorter hospital stay and blood loss, but not different in terms of the necessity of post-operative analgesics, recurrence and re-operation rate19. Bredow et al. compared post-operative analgesic requirement, functional outcome and VAS score in a randomized control trial with macro and micro discectomy and found a difference in operation time, blood loss, hospital stay, but none of them were clinically significant 20. Shorter hospital stays, less blood loss and procedure time are not associated with improved clinical results and are not an indicator of sciatica or recurrence21.
Microdiscectomy is commonly, seen as a safe operation with a particularly low incidence of surgical complications. Despite being the world’s most successful spinal operation, studies have indicated that 10 to 15 percent of patients fail to achieve the desired outcome11. The outcome of lumbar discectomy in elderly patients was indicated by Fujii et al. to be as successful as in younger patients. Our results are consistent with the research by Fujii et al 17. Physiotherapy could have a beneficial effect after lumbar spine surgeries on the clinical and functional outcomes22. Bed rest is no more successful care than watchful waiting for patients with symptoms and signs of lumbosacral radicular syndrome23. In the case of Cauda Equina syndrome, a motor deficit lower than or equivalent to 3/5 or hyperalgic radicular pain immune to full medical treatment, including opioid medications, is indicated in emergency circumstances24.
One research reveals that relatively straightforward therapeutic adjustments result in decreased absenteeism of illness for ‘first-time’ sufferers’ only25. The content and timing of pain management therefore tend to be critical. Therefore, properly administered early intervention can minimize sick leave and avoid chronic problems, thereby saving significant resources26.
We would like to illustrate some weaknesses of our research study. First, data was collected retrospectively and during implementation of rigorous clinical pathways, concluded in collecting detailed patient information, the authors were still unable to calculate variables, such as pre- and post-operative Oswestry Disability Indices, that might be of interest to readers. Our research population consisted exclusively of those patients who failed non-operative treatment, commonly documented to be successful in more than 80% of the patients with neuralgia (sciatica) 12.
Microdiscectomy (MD) is a safe treatment in patients who do not improve on conservative therapy, with excellent outcomes for prolapsed lumbar intervertebral discs (PLID). Promising outcomes are provided by early post-operative physiotherapy that includes dural stretching to prevent epidural fibrosis leading to recurrent pain caused by nerve irritation and to develop paravertebral muscles to prevent disc prolapse at other spinal levels. The earlier the surgical intervention is performed, better the outcomes are observed regarding pain, neurological deficit and sphincter problem.
The authors would like to extend their gratitude to the staff of the hospital their help in patient management during research work.
The authors declare no conflict of interest.
Consents were obtained from the patients of the study.
SKP had conceptualized the idea, written the manuscript and performed the data analysis. SM did the data collection, contributed in manuscript writing and data analysis. NH also assisted in data collection and data analysis. IAH and MSR had also conceptualized the idea and reviewed the clinical research write-up.
- Kreiner DS, Hwang SW, Easa JE, Resnick DK, Baisden JL, Bess S, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014;14(1):180-191.
- Arts MP, Kuršumović A, Miller LE, Wolfs JF, Perrin JM, Van de Kelft E, et al. Comparison of treatments for lumbar disc herniation: systematic review with network meta-analysis. Medicine. 2019;98(7)1-9.
- Vialle LR, Vialle EN, Suárez Henao JE, Giraldo G. Lumbar disc herniation. Rev Bras Ortop. 2015;45(1):17-22.
- Zahid H, Ali I, Choudhary N, Rashid J, Mehmood K. Microscopic discectomy outcomes in lumbar disc herniation patients. Pak J Neurol Surg. 2019;23(2):142-145.
- Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Young JY, Clabeaux DE, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg Spine. 2002;96(1):34-44.
- Yasargil MG. Microsurgical operation of herniated lumbar disc. In Lumbar Disc Adult Hydrocephalus 1977 (pp. 81-81). Springer, Berlin, Heidelberg.
- Katayama Y, Matsuyama Y, Yoshihara H, Sakai Y, Nakamura H, Nakashima S, et al. Comparison of surgical outcomes between macro discectomy and micro discectomy for lumbar disc herniation: a prospective randomized study with surgery performed by the same spine surgeon. Clin Spine Surg. 2006;19(5):344-347.
- Hejazian SE, Dadpour M. Frequency of instrumentation in lumbar spinal stenosis and lumbar disc herniation. Iran J Neurosurg. 2016;2(2):6-9.
- Akbar A, Mahar A. Lumbar disc prolapse: management and outcome analysis of 96 surgically treated patients. J Pak Med Assoc. 2002;52(2):62-65.
- Schneck CD. The anatomy of lumbar spondylosis. Clin Orthop Relat Res. 1985; (193):20-37.
- Morgan-Hough CV, Jones PW, Eisenstein SM. Primary and revision lumbar discectomy: a 16-year review from one centre. J Bone Joint Surg Br. 2003;85(6):871-874.
- Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. SAS J. 2009;3(1):30-40.
- Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A. Current concepts for lumbar disc herniation. Int Orthop. 2019;43(4):841-851.
- Delgado-López PD, Rodríguez-Salazar A, Martín-Alonso J, Martín-Velasco V. Lumbar disc herniation: Natural history, role of physical examination, timing of surgery, treatment options and conflicts of interests. Neurocirugia. 2017;28(3):124-134.
- Riouallon G, Wolff S. Surgical treatment of lumbar disc herniations. Rev Prat. 2016;66(4):393-396.
- Omidi-Kashani F, Ghayem Hasankhani E, Kachooei AR, Rahimi MD, Khanzadeh R. Does duration of preoperative sciatica impact surgical outcomes in patients with lumbar disc herniation? Neurol Res Int. 2014;2014:1-5.
- Fujii K, Henmi T, Kanematsu Y, Mishiro T, Sakai T. Surgical treatment of lumbar disc herniation in elderly patients. J Bone Joint Surg Br. 2003;85(8):1146-1150.
- Shrestha D, Shrestha R, Dhoju D, Kayastha SR, Jha SC. Study of clinical variables affecting long term outcome after microdisectomy for lumbar disc herniation. Kathmandu Univ Med J (KUMJ). 2015;13(4):333-340.
- Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25(22):2940-2953.
- Bredow J, Eysel P, Oikonomidis S. Postoperative management of stress and rehabilitation after lumbar spine surgery. Orthopade. 2020;49(3):201-210.
- Frymoyer JW. Back pain and sciatica. N Engl J Med. 1988;318(5):291-300.
- Vroomen PC, De Krom MC, Knottnerus JA. Predicting the outcome of sciatica at short-term follow-up. Br J Gen Pract. 2002;52(475):119-123.
- Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Lack of effectiveness of bed rest for sciatica. N Engl J Med. 1999;340(6):418-423.
- Moulton HN, Lurie JD. Management of sciatica: a shared-decision. AME Med J. 2018; 3: 43-46.
- Peul WC, Van Houwelingen HC, van den Hout WB, Brand R, Eekhof JA, Tans JT, et al. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007;356(22):2245-2256.
- Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW, Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ. 2008;336(7657):1355-1358.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
