By Yasir Sindhi1, Altaf Hussain Hashmi1, Ghazala Usman2, Aliya Zaman3,4, Mudassir Hussain1, Usman Qamar1
AFFILIATIONS:
- Department of Urology, Sindh Institute of Urology and Transplantation (SIUT).
- Department of Community Medicine, Jinnah Sindh Medical University.
- Government Hospital Korangi.
- Muhammad Medical College, Mirpur Khas, Sindh, Pakistan.
ABSTRACT
Background: Despite the emergence of many novel minimally invasive techniques including percutaneous nephrolithotomy, ureteroscopy, extracorporeal shock wave lithotripsy, many urologists still prefer open surgery for the management of ureteric stones. The present study compared the efficacy of extracorporeal shockwave lithotripsy (ESWL) with ureteroscopy (URS) for the treatment of distal ureteral calculi.
Methods: A single-blinded, randomized controlled trial, which was conducted between January 2018 to June 2019 at the Sindh Institute of Urology and Transplantation, Karachi, Pakistan. All patients diagnosed with unilateral, solitary, and distal ureteral stones were randomized in two groups. The patients in Group A underwent with ESWL and group B underwent ureteroscopy. The outcome of procedures was assessed after 3 months. Data was analyzed via Statistical Package for the Social Sciences (SPSS version 25). Chi-squared test was applied to compare the clinical efficacy of both techniques. A p<0.05 was considered as statistically significant.
Results: Out of 106 patients, majority were females n=61(58%). Overall, the mean age of population was 41.9 ± 10.4 years, and the mean stone size was 13.1 ± 4.3 mm. Both the groups were almost comparable with respect to age and size of stones. There was a significant difference in outcome of both the procedures, as the residual stones were more in ESWL and URS i.e., 64.0% vs. 33.9% (p=0.019).
Conclusion: In hospitals, both of the techniques are suitable for treatment purpose. However, the present results suggest that URS is a more effective procedure than ESWL (p=0.019) for treating ureteral stones and should be utilized as the first-line treatment for distal ureteral calculi.
Keywords: Lithotripsy; Ureteroscopy; Ureteral Calculi.
Ureterolithiasis is a common disease with an estimated prevalence of 10-15% in Pakistan1,2. The most common site where most of these ureteric calculi are found is the distal ureter3. Stones of size less than 5 mm have usually excreted out simultaneously with the spontaneous expulsion rate ranging from 71-98%. However, for distal ureteral stone greater than 5 mm, immediate intervention is usually required4-6.
Despite the emergence of many novel minimally invasive techniques including percutaneous nephrolithotomy (PCNL), ureteroscopy (URS), extracorporeal shock wave lithotripsy (ESWL), many urologists still prefer open surgery for the management of ureteral stones7,8. Hence, the issue of the optimum first-line treatment remains unresolved. ESWL and URS are two of the most usedinterventions7.
ESWL is the new non-invasive form of treatment for ureteric stones. With this treatment, the patient is subjected to a series of shock waves formed by a device known as lithotripter. The calculus is broken into minute fragments by focusing the shock waves with the help of the X-rays. Following the procedure, the fragments pass out of the body in the urine within a few weeks9.
Since ESWL is a completely non-invasive procedure, it has been associated with shorter hospitalization days and a lower complication rate. Nevertheless, ESWL is an advanced and costly technique and not every surgeon can perform it due to limited resources and patient’s financial constraints. ESWL often requires multiple treatment sessions, which proves to be a nuisance for the patient10.
On the other hand, ureteroscopic surgery provides a more rapid stone clearance with prompt comfort to the patient and is cost effective albeit it demands anesthesia, longer duration of hospitalization, and a higher incidence of complications11,12. Nevertheless, the decision to use either ESWL or ureteroscopy depends on several factors including the series of procedures required to get rid of all stones, the duration of the hospitalization, the anesthesia requirement, the expertise of the surgeon and the availability of the equipment at the health-care centre. The current study was conducted to explore the different treatment modalities for the management of distal ureteral stones to determine which could be utilized as the first-line treatment for the patients in our local setting. Therefore, the objective of our study was to assess and compare the efficacy of ESWL and ureteroscopy for the treatment of distal ureteral stones.
A randomized controlled trial was conducted between January 2018 to June 2019 at the Urology Department of Sindh Institute of Urology and Transplantation, (SIUT), Karachi, Pakistan. Ethical approval was procured from the institutional review board. Informed written consent was obtained from all patients prior to the study (reference number IRB/2017/-315). A sample size of 106 (53 in each group) was calculated by taking the percentage of efficacy in ureteroscopy (URS) group 94.1% and in extracorporeal shock wave lithotripsy (ESWL) group 73.5%, level of significance was 5% with the power value of 90% for the study. All adult patients between the age of 25 and 60 years, diagnosed with a single stone, which is a radiopaque on X-rays, is located at the distal ureteric region, and is between 5 mm to 20 mm were included in the study. Patients with kidney anomalies including solitary or horseshoe kidney, coagulopathy, multiple ureteric stones were excluded from the study. Pregnant women and morbidly obese patients were also excluded. After ethical review committee approval, all patients satisfying the inclusion criteria visiting the Urology Stone Clinic were enrolled in the study. Informed written consents were obtained by the patients prior to the initiation of the treatment process. The principal investigator explained about the purpose, procedure, risks, and benefits of the study to all patients. Patients with even numbers were assigned to the group A, who underwent ESWL and those with odd numbers were in group B, who underwent URS.
ESWL performed using a third-generation electromagnetic lithotripter. All patients were settled in a prone position and stones were localized using fluoroscopy. All patients were given preprocedural analgesia and post procedure analgesia and antibiotics. URS was performed by an experienced urologist having at least 10 years-experience, using a Tip-flexible Semi-rigid Ureterorenoscope FR 8, (Karl Storz)12. Stones were disintegrated with Swiss LithoClast® pneumatic lithotripters while the surgeon decided ureteric stent placement.
All patients were given empirical antibiotic therapy and post procedure antibiotics and analgesics. Patients in both groups followed to assess the result of two procedures. The follow up schedule was the same for all patients i.e., maximum 3 sessions were done, and final outcome was seen at 3 months. Plan abdominal radiograph and ultrasound was performed on each visit. All data were collected on computerized pre-structured proforma.
Data was analyzed and entered with the help of Statistical Package for the Social Sciences (SPSS version 25). Categorical variables were included the gender and efficacy of the treatment. Descriptive statistics were used to summarize continuous variables. The Chi-squared test was applied to assess the success of treatment and evaluate the outcome in both groups. Stratification with respect to demographics and clinical features were done, and post stratification Chi-squared tests were applied. A p<0.05 was taken as statistically significant.
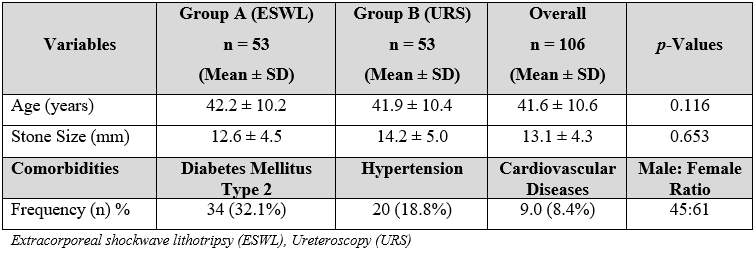
A mean age of 42.2 ± 10.2 years was observed in group A (ESWL) and 41.9 ± 10.4 years in group B (URS). In addition, 45 (42%) of the patients were male and 61 (58%) were female. The overall mean ± SD stone size was 13.1 ± 4.3 mm; 12.6 ± 4.5 and 14.2 ± 5 mm in group A and B respectively (Table 1).
Table 1: Descriptive statistics and clinical profile of the patients.
We observed complications at follow-up visit 14 days postoperatively in both groups. We found that of the 53 patients who underwent ureteroscopy, 6 (11.3%) experienced flank pain at 14-day follow-up while only 2 patients (3.7%) patients in ESWL. Incidence of urinary tract infection was more frequently observed in patients who underwent URS compared to those who underwent ESWL, 3 (5.7%) and 1 (1.9%), respectively. Other complications observed were lower urinary tract symptoms including obstructive symptoms such as poor stream, hesitancy, and dribbling. Furthermore, 4 patients (7.5%) in the URS group and 10 patients (18.8%) in the ESWL group experienced the voiding symptoms (Figure 1).
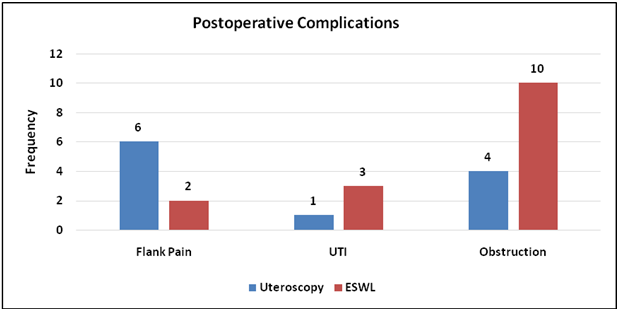
Figure 1: Complications in URS (n=53) and ESWL (n=53) group at 14-day follow-up visit.
Extracorporeal shock wave lithotripsy (ESWL), ureteroscopy (URS), urinary tract infection (UTI)
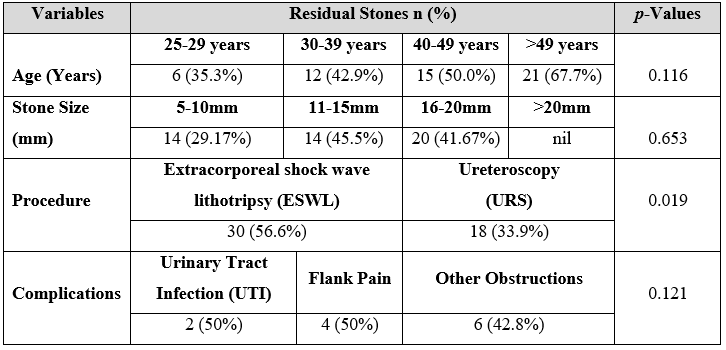
In the present study, 6 patients between the ages of 25-29 years, 12 patients between the ages of 30-39 years, 15 patients between the ages of 40-49 years, while 21 patients aged 50 years or older had a residual stone after their procedures. Despite the increase in frequency in older patients, the difference remained statistically insignificant (p=0.116) (Table 2).
URS was found to be more effective than ESWL as in 18 (33.9%) patients residual stone was observed in URS group in comparison to ESWL group in which residual stone was observed in majority 30 (56.6%) of patients (p=0.019). No significant association was observed between age groups and residual stone (p=0.116). The relationship between stone size and residual rate was not significant (p=0.653) (Table 2).
Table 2: Association of age, stone size, and procedure with the presence of residual stones.
In the present study, ureteroscopy (URS) was found to be more effective as in only 33.9% patients who underwent URS, a residual stone was observed in comparison to the extracorporeal shock wave lithotripsy (ESWL) group in which a residual stone was observed in majority 30 (56.6%) of the patients (p=0.019).
Undoubtedly, there has been a remarkable development and miniaturization of endoscopic devices has been very attractive to surgically oriented urologists13. A 2007 consensus guidelines on management of ureteral stones claimed that the overall success rate of URS is superior to ESWL in distal ureteric stones14. Ureteric stones are a common disease prevalent in Pakistan and a major problem for tertiary care hospitals. Despite the huge burden of ureteric stones in our population, only a few local studies have been conducted in our setting2,16,17. The ever-occurring advancement in endourological management of ureteral stones raises the question about the optimal management of distal ureteric stone among urologists. Several treatments are available for ureteral stone clearance. ESWL and URS are the most widely used methods for this purpose globally. The literature has been inconsistent in determining the optimum technique for the treatment of distal ureteral stones.
In accordance with our study, Islam and Malik also reported a greater success rate with URS compared to ESWL18. Similarly, in another study by Lee et al. 7 (31.8%) patients were stone free after ESWL while the stone free rate for URS was 35% 19. In short, the authors did not support SWL for the management of upper ureteral stones larger than 15 mm. However, in contrast to our study, Rahman et al. reported a ureteric stone clearance of 80% with ESWL and also associated ESWL with a low rate of complications hence, recommended ESWL as a safe procedure for ureteric stone clearance20. In our study only minor complications were observed including voiding symptoms, flank pain, and UTI. None of the patients developed any severe complications. Marchetti et al. reported similar observations albeit in pediatric population21.
Hence, no surgical procedure is without complications, whether invasive or noninvasive. Apart from some mild complications associated with ESWL like renal colic, bleeding, gastrointestinal tract side effects, and slight blood pressure changes, some more dreadful complications were observed in previous studies indicating that ESWL is not safe in all patients22,23. There are some conditions when ESWL is absolutely contraindicated including pregnancy, untreated coagulopathy, refractory hypertension, obstruction distal to the calculus, and fever associated with a urinary tract infection. The current study did not observe any postoperative complications in any group.
The stone size can contribute to the prognosis and the overall patient outcome. In our research study, the larger stone sizes were associated with a higher incidence of a residual stone irrespective of the procedure. However, the difference was statistically insignificant. La Rosette reported that ESWL was safer for the management of mid and lower ureteral stones of sizes less than 50 mm2 but for larger stones, they claimed URS to be safer24.
Another study by Ghalayini, reported a higher efficacy with fewer complications and quick recovery in patients who were treated with ureteroscopy compared to patients who underwent ESWL for the treatment of distal ureteral calculi25. In contrast to the present study, Izamin et al. reported that there was no significant variation in the success rates and quality of life (QOL) of patients after procedure between URS and ESWL26. The reason for the evident difference between the two procedures can be attributed to the larger size of stones, older age, comorbidities, recurrence of stones, inexperienced surgeon or staff, or the unavailability of the equipment. Further research should focus on stratification of patients and exploring the possible associations with treatment failure.
In the end, the current study has assessed the success rate of ESWL and URS suggested that URS was more successful than ESWL (success rate: 66.0% vs. 43.4% respectively) with respect to the treatment of distal ureteric calculi. Therefore, the authors of the present study recommend URS as the first-line treatment for patients presenting with distal ureteral calculi.
Ureteroscopy (URS) is a more effective and alternative procedure than ESWL for treating ureteral stones and should be used for the treatment of distal ureteral calculi in patients in our setting.
We thank all our patients who gave consent to participate in the study.
The authors declare no conflict of interest.
The Institutional Review Board under the reference number: IRB/2017 /-315 approved the research study.
All patients signed the informed written consent prior to the study.
All authors contributed equally and substantially in this research manuscript.
- Scales Jr CD, Smith AC, Hanley JM, Saigal CS, Urologic diseases in America project. Prevalence of kidney stones in the United States. Eur Urol. 2012;62(1):160-165.
- Ludwig WW, Matlaga BR. Urinary stone disease: diagnosis, medical therapy, and surgical management. Med Clin. 2018;102(2):265-277.
- Meissnitzer M, Meissnitzer T, Hruby S, Hecht S, Gutzeit A, Holzer-Frühwald L, et al. Comparison of prone vs. supine unenhanced CT imaging in patients with clinically suspected ureterolithiasis. Abdom Radiol. 2017;42(2):569-576.
- Lay AH, Raman JD, Pearle MS. Surgical management of ureteral stone disease. Evid Based Urol. 2018:171-183.
- Tan J, Singh P, Huang E, Han HC. Spontaneous expulsion of giant bladder stone: Case report. J Med Cases. 2018;9(2):58-60.
- Janssen KM, Brand TC, Bailey MR, Cunitz BW, Harper JD, Sorensen MD, et al. Effect of stone size and composition on ultrasonic propulsion ex vivo. Urol. 2018;111:225-229.
- Pradère B, Doizi S, Proietti S, Brachlow J, Traxer O. Evaluation of guidelines for surgical management of urolithiasis. J Urol. 2018;199(5):1267-1271.
- Shafi H, Moazzami B, Pourghasem M, Kasaeian A. An overview of treatment options for urinary stones. Caspian J Intern Med. 2016;7(1):1-6.
- Zumstein V, Betschart P, Abt D, Schmid HP, Panje CM, Putora PM. Surgical management of urolithiasis–a systematic analysis of available guidelines. BMC Urol. 2018;18(1):1-8.
- Batra R, Batra P, Bokariya P, Kothari R. Role of extracorporeal shock wave lithotripsy in management of upper ureteric stones. Afr J Urol. 2018;24(3):186-190.
- Somani BK, Giusti G, Sun Y, Osther PJ, Frank M, De Sio M, et al. Complications associated with ureterorenoscopy (URS) related to treatment of urolithiasis: the clinical research office of endourological society URS global study. World J Urol. 2017;35(4):675-681.
- Holden T, Pedro RN, Hendlin K, Durfee W, Monga M. Evidence-based instrumentation for flexible ureteroscopy: a review. J Endourol. 2008;22(7):1423-1426.
- Desai M, Sun Y, Buchholz N, Fuller A, Matsuda T, Matlaga B, et al. Treatment selection for urolithiasis: percutaneous nephrolithomy, ureteroscopy, shock wave lithotripsy, and active monitoring. World J Urol. 2017;35(9):1395-1399.
- Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck C, Gallucci M, et al. 2007 guideline for the management of ureteral calculi. J Urol. 2007;178(6):2418-2434.
- Tan YM, Yip SK, Chong TW, Wong MY, Cheng C, Foo KT. Clinical experience and results of ESWL treatment for 3093 urinary calculi with the Storz Modulith SL 20 lithotripter at the Singapore General Hospital. Scand J Urol Nephrol. 2002;36(5):363-367.
- Tipu SA, Malik HA, Mohhayuddin N, Sultan G, Hussain M, Hashmi A, et al. Treatment of ureteric calculi-use of Holmium: YAG laser lithotripsy versus pneumatic lithoclast. J Pak Med Assoc. 2007;57:440-443.
- Pirzada AJ, Anwar A, Javed A, Memon I, Mohammad A. Role of alpha-1 blocker in expulsion of stone fragments after extracorporeal shock wave lithotripsy for renal stones. J Ayub Med Coll Abbottabad. 2011;23(2):125-129.
- Islam M, Malik A. Ureteroscopic pneumatic versus extracorporeal shock wave lithotripsy for lower ureteral stones. J Coll Physicians Surg Pak. 2012;22(7):444-447.
- Lee YH, Tsai JY, Jiaan BP, Wu T, Yu CC. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopic lithotripsy for management of large upper third ureteral stones. Urol. 2006;67(3):480-484.
- Rahman MM, Shamim IA, Kormokar U, Chowdhury SA, Gupta SD. Outcome of extracorporeal shock wave lithotripsy in the treatment of mid ureteric stones. Bangladesh Med J. 2014;43(2):72-78.
- Marchetti KA, Lee T, Raja N, Corona L, Kraft KH, Wan J, et al. Extracorporeal shock wave lithotripsy versus ureteroscopy for management of pediatric nephrolithiasis in upper urinary tract stones: multi-institutional outcomes of efficacy and morbidity. J Pediatr Urol. 2019;15(5):516-e1-e8.
- Nussberger F, Roth B, Metzger T, Kiss B, Thalmann GN, Seiler R. A low or high BMI is a risk factor for renal hematoma after extracorporeal shock wave lithotripsy for kidney stones. Urolithiasis. 2017;45(3):317-321.
- Fankhauser CD, Hermanns T, Lieger L, Diethelm O, Umbehr M, Luginbühl T, et al. Extracorporeal shock wave lithotripsy versus flexible ureterorenoscopy in the treatment of untreated renal calculi. Clin Kidney J. 2018;11(3):364-369.
- La Rosette D. Treatment of mid-and lower ureteric calculi: extracorporeal shock-wave lithotripsy vs laser ureteroscopy. A comparison of costs, morbidity and effectiveness. Br J Urol. 1998;81(1):31-35.
- Ghalayini I, Al-Ghazo M, Khader Y. Extracorporeal shockwave lithotripsy versus ureteroscopy for distal ureteric calculi: efficacy and patient satisfaction. International Braz J Urol. 2006;32(6):656-667.
- Izamin I, Aniza I, Rizal A, Aljunid S. Comparing extracorporeal shock wave lithotripsy and ureteroscopy for treatment of proximal ureteric calculi: a cost-effectiveness study. Med J Malaysia. 2009;64(1):12-21.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
