By Sadaf Saleem Uppal1, Abdul Khaliq Naveed2, Asifa Majeed3, Mazhar Shafiq4, Kiran Namoos1, Saeeda Baig5
AFFILIATIONS:
- Department of Biochemistry, Shalamar Medical and Dental College, Lahore.
- Department of Biochemistry, CMH Lahore Medical College.
- Department of Biochemistry and Molecular Biology, Army Medical College, Rawalpindi.
- Department of Radiology, CMH Kohat, 5Department of Biochemistry, Ziauddin University, Karachi, Pakistan.
ABSTRACT
Background: The polycystic ovarian syndrome (PCOS), a well-known endocrine-metabolic disease, is caused by the interaction of environmental, genetic and metabolic factors. A cross-sectional, comparative study was planned to evaluate high sensitivity C-reactive protein (hs-CRP), insulin and lipid profile in non-obese and obese PCOS patients.
Methods: Seventy-two women diagnosed with PCOS as per Rotterdam criteria, were placed in three groups in accordance with the body mass index: Group 1 (normal weight), Group 11 (overweight), and Group 111 (obese). Blood glucose, hs-CRP, serum insulin, lipid profile was estimated and insulin resistance was calculated. Data was analyzed using version 20 of SPSS. Analysis of variance (ANOVA) was used to compare the numeric variables among three groups of PCOS women and p-value < 0.05 was considered statistically significant.
Results: Significantly, higher levels of insulin (13.03 ± 0.22), triglyceride (1.74 ± 0.96) and hs-CRP (7.24±4.11) were detected in obese PCOS women. The levels of fasting blood glucose (4.61±0.54) were also raised. Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) (2.69±0.79) showed insulin resistance in obese PCOS women (p=0.004). The obese group had significantly lower HDL-Cholesterol levels (0.82±0.09). Levels of total cholesterol (4.69±0.97) and LDL-Cholesterol (3.08±0.64) were increased but results were non-significant. These results indicate obesity leads to insulin resistance, dyslipidemia with low grade inflammation in PCOS.
Conclusion: Frequency of insulin resistance, dyslipidemia and low-grade inflammation was found significantly higher in young obese PCOS women. Obesity may have an important role in the aetiology as well as the complications associated with PCOS.
Keywords: Polycystic Ovarian Syndrome; hs-CRP; Insulin Resistance; Dyslipidemia; Body Mass Index.
The polycystic ovarian syndrome (PCOS), a well-known endocrine as well as metabolic disorder, affects 5-10% of fertile age women1. It is proposed that interaction of environmental, genetic, metabolic, endocrine and neurological factors lead to progression and pathogenesis of PCOS2. Rotterdam standards for diagnosis of PCOS are based on the occurrence of three findings i.e., ovulatory dysfunction, hyperandrogenism, and polycystic ovaries on ultrasonography3.
Adverse metabolic disorders associated with PCOS include low-grade inflammation, dyslipidemia, insulin resistance, cardiovascular problem and diabetes4,5. Insulin resistance (IR) is the main feature of PCOS with its occurrence in > 70 % of women. The outcomes of IR are incorrect signaling of metabolic pathways with intact steroidogenic and mitogenic activity, supporting hyperandrogenemia the main clinic factor of PCOS6.
Lipid abnormalities, common in women with PCOS, are related with IR and may be a predictor of myocardial infarction7. Women with PCOS may have a high risk of development of cardiovascular disease (CVD). This may relate with the penalties of IR such as hypertension, dyslipoproteinemia, low-grade inflammation, higher oxidative stress, impair hemostasis and myocardial energetics7.
PCOS is a metabolic issue associated with imbalance of hormones and this may affect the health of women and may be related with mutable complications. The occurrence of PCOS in our country is less well described. Some studies have focused on metabolic characteristics. Central obesity is common in PCOS and it is proposed that cells of visceral fat may release molecules of inflammation. It is therefore a need to locate a clear link between dyslipidemia, IR and inflammation in PCOS. This study was designed to measure and compare hs-CRP and insulin levels as well as lipid profile in non-obese and obese women with PCOS.
Present study was carried out on n=72 women with polycystic ovarian syndrome (PCOS) of age between 15-49 years after approval from the Ethical Committee of Army Medical College (Letter No: 02/CREAM-A/Sadaf; Dated: 13/03/2014). These women were enrolled by non-probability purposive sampling in the study. The patients were selected as per Rotterdam criteria for diagnosis of PCOS. Exclusion criteria included women with CVD, diabetes and inflammatory disease. Consented women were separated into three groups based on values of BMI. Group I included 30 normal weight PCOS women (BMI range 18.5 to 24.9 kg/m2), a total of 21 overweight women (BMI range 25 to 29.9 kg/m2) and 21 obese PCOS women (BMI equal to and more than 30 kg/m2) were included in group II and group III respectively6.
Blood sample was collected from women with PCOS for estimation of hs-CRP, blood sugar, serum insulin, triglyceride (TG), total cholesterol (TC), HDL-Chol and LDL-Chol (lipid profile) in the fasting state. Lipid profile and blood glucose were estimated by Auto- analyser using standard kits. Serum insulin and hs-CRP were measured by the technique of ELISA. To calculate Insulin resistance (IR) HOMA–IR, the given formula was used7.
HOMA-IR = Blood glucose X serum insulin / 405
In addition, Friedewald’s formula was used to calculate LDL-cholesterol: LDL-c (mg/dL) = TC (mg/dL) – (HDL-c (mg/dL) + TG (mg/dL) /5).
Data was analyzed using version 20 of SPSS. Qualitative variables were stated as Mean±SD. Analysis of variance (ANOVA) was used to compare the numeric variables among three groups of PCOS women and p-value < 0.05 was considered statistically significant.
Among three groups of polycystic ovarian syndrome (PCOS) women based on their BMI, majority (54%) of the women were less than 30 years of age. Fifty-one (71%) out of 72 women were married and among them 41(57%) women had infertility (Table 1). The difference was observed in the clinical presentation of women with PCOS both within as well as among the groups as given in Figure 1.
Table 1: Demographic data of the women patients with polycystic ovarian syndrome (PCOS).
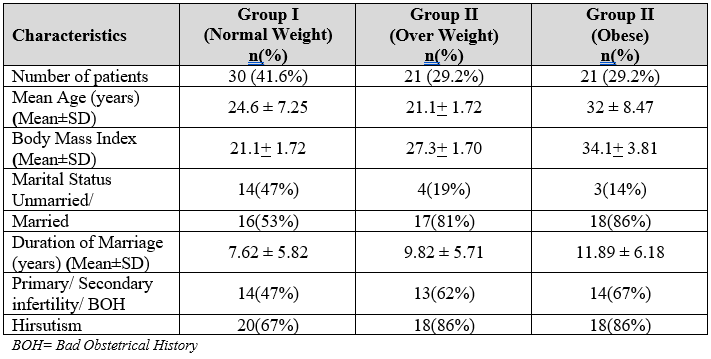
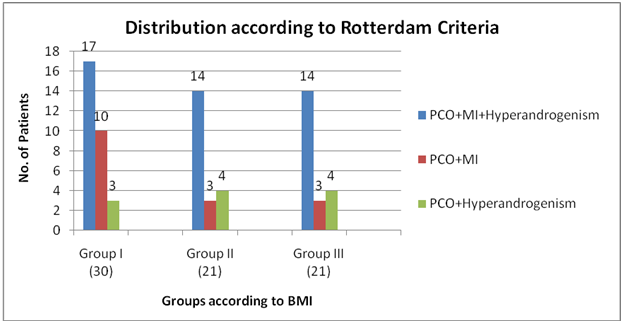
Figure 1: Selection of polycystic ovarian syndrome (PCOS) patients in three groups according to Rotterdam Criteria, (PCO= Polycystic ovaries; MI= Menstrual Irregularities).
Biochemical parameters among the three groups showed considerable differences. Table 2 displays the Mean±SD (SE) and significance (ANOVA) of the biochemical parameters measured in the three PCOS women groups. The distinction in the blood glucose levels among the three groups of PCOS women was non-significant. However, PCOS women belonging to obese group had significantly elevated serum insulin levels and values of IR (p-value 0.004) compared to normal and overweight PCOS women.
Table 2: Biochemical parameters of the patients with polycystic ovarian syndrome (PCOS).
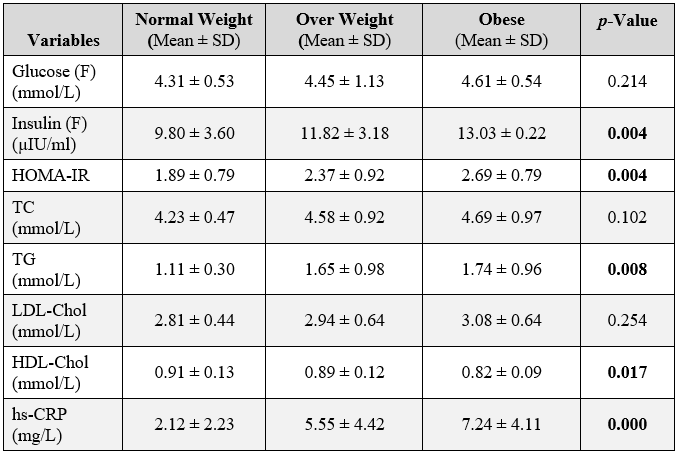
HOMA-IR (Homeostatic Model Assessment for Insulin Resistance), Total Cholesterol (TC), Triglyceride (TC), Low-Density Lipoprotein (LDL), High-density Lipoprotein (HDL), High-sensitivity C-reactive Protein (hs-CRP)
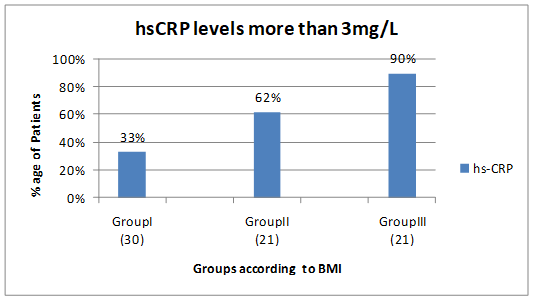
Figure 2: Patients with high-sensitivity C-reactive protein (hs-CRP) levels (>3mg/L) in the three groups of polycystic ovarian syndrome (PCOS) women.
Among three groups of PCOS women, statistically significant difference between the levels of triglyceride and HDL-Chol was observed whereas non-significant difference was observed between the levels of LDL-Chol and total cholesterol. Significantly, higher levels of serum hs-CRP were found in the obese group in comparison to the other two groups. Figure 2 shows the percentage of patients with hs-CRP levels >3mg/L in the three groups.
Obesity, in general and visceral adiposity, in particular, amplifies and deteriorates metabolic as well as reproductive outcomes in women with PCOS. Results of the present study proposed that obesity might be the linkage between inflammation and disturbed lipid profile in PCOS syndrome. In this study, we observed the condition of low-grade inflammation in obese group of PCOS women. Obesity in association with IR and hyperandrogenism influence dyslipidemia via excessive synthesis of VLDL, impair lipolysis and default insulin-signaling pathway8. Besides, testosterone also sways dyslipidemia via receptor of androgen mediated IR and up-regulation of genes of HDL catabolism9. Obesity associated IR and hyperinsulinemia motivates steroidogenesis in ovary, blocks the synthesis of androgen transporter protein and causes high free androgens levels that may lead to accumulation of visceral fat10.
The probable inflammatory mechanisms are accountable for the low-level inflammation which link insulin resistance with the metabolic complications of the PCOS syndrome has been studied11. A good predictor of inflammation is CRP, which indicates individualistically the risk of CVD12. They may contain mediators of oxidative stress, cytokines and markers of inflammation of endothelium like hs-CRP, homocysteine, tumor necrosis factors and interleukins, etc. High interleukins stimulate liver CRP secretion and results in increased rate of inflammation, imbedded tool for development of diseases like atherosclerosis, insulin resistance, metabolic syndrome and diabetes. American Heart Association has classified serum hs-CRP levels <1mg/L, 1-3mg/L and >3mg/L as little, moderate, and high-risk groups for risk of CVS respectively12,13. Hs-CRP levels in three groups of PCOS women in this study showed highly significant difference. The reported levels of serum CRP greater than 2 mg/L are in response to inflammation, insulin resistance, central obesity, and coronary heart disease14. The obese women with PCOS showed high levels of hs-CRP compared to PCOS women belonging to the other two groups.
This study exhibited a positive relationship between hs-CRP levels and BMI. Previous studies have also shown similar association15. However, upsurge in the levels of hs-CRP has been seen in women with PCOS regardless of BMI16. The present study shows interrelationship between dyslipidemia and the levels of hs-CRP (marker of inflammation) particularly in the obese PCOS women. In the present study, dyslipidemia was significantly high in obese as well as overweight PCOS women. Excess weight and obesity, worldwide, are recognized as a cause of many major chronic syndromes. Among these, some characteristics of PCOS are attributed to obesity including complications of pregnancy, hirsutism, hyperandrogenism and infertility17.
Number of studies have observed dyslipidemia in obese and overweight women and found its association with insulin resistance. A study demonstrated that abnormalities of lipid metabolism is a characteristic feature of obesity and may be related with pro-inflammatory inclination, that originate in adipose tissue and directly affect endothelium18. The link between obesity, dyslipidemia, and metabolic syndrome has a role in the occurrence of IR in peripheral tissues. The increase in release of fatty acid from liver, resist the anti-lipolytic function of insulin19,20.
According to our study, obese women with PCOS had significantly raised serum insulin levels and values of insulin resistance (IR) compared to normal weight and overweight PCOS women21. Our study is inconsistent with a previous study, which also observed significantly high level of insulin resistant with non-significantly high level of blood glucose22. Some researchers suggest that obesity exert a synergetic effect on the development of PCOS, with an altering effect on sensitivity of insulin and on gonadotrophin secretion and may increase the risk of CVD and diabetes23. Additionally, a study found IR significantly related with BMI in PCOs women. However, BMI < 29 kg/m2 in some women can be a predictor of non-IR24.
In the present study, fasting blood glucose levels were within the normal range among the three groups of PCOS women. However, serum levels of insulin and values of HOMA-IR were raised significantly in overweight and obese groups as compared to normal weight PCOS women25. These results show predisposition towards IR and its compensated hyperinsulinemia. Hyperinsulinemia was responsible for normal glucose levels in these patients26. These observations exhibited a robust association between obesity and IR, another study reported similar findings27.
Many drug treatment strategies have been unsuccessfully applied for treatment of PCOS in obese women. However, lifestyle modifications have been found as best interventions for PCOS treatment focusing on diet control and concurrent exercise leading to weight loss. Weight loss as less as 5 to 10% considerably improved PCOS symptoms and spontaneous ovulation and early pregnancy was also observed28.
Research in obese women with PCOS at molecular level can help in better understanding of the syndrome and assist in controlling obesity, hyperinsulinemia, as well as correcting inflammation hyperandrogenism related with it29. The women should be guided to lose weight loss prior to conception to improve live birth rate in obese. The treatment of obesity should include lifestyle modifications including workouts with a close watch on healthy eating. The pharmacological intervention or bariatric surgery should be the last options.
Presence of obesity in young PCOS women intensifies insulin resistance, dyslipidemia, low grade inflammation and may have a significant role in the aetiology as well as the complications linked with PCOS. It is suggested that molecular level research should be implemented to get an insight into the genetic origin of the disease. Moreover, early weight control in life can greatly reduce the burden on both the health and economic conditions of PCOS in future generations.
The authors would like to acknowledge the Radiology and Gynecology Department of HITEC Hospital for their immense contribution in PCOS patient’s selection and sampling.
The authors declare no conflict of interest.
The ethical committee of Army Medical College had approved this study (Letter No: 02/CREAM-A/Sadaf; Dated: 13/03/2014).
Patients’ consents were taken prior to the experimentations.
MS collected the patients according to Rotterdam criteria and did sampling, SSU and KN performed the biochemical analysis, SSU and AM analyzed and interpreted the patient data, SSU, AM and SB were the major contributors in writing the manuscript, AKN reviewed and finalized the manuscript.
- Bellver J, Rodríguez-Tabernero L, Robles A, Martínez F, Landeras J, García-Velasco J, et al. Polycystic ovary syndrome throughout a woman’s life. J Assist Reprod Genet. 2018;35(1):25-39.
- 2. Sanchez-Garrido MA, Tena-Sempere M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol Metab. 2020; 35:1-16
- 3. William T, Mortada R, Forter S. Diagnosis and treatment of polycystic ovary syndrome. Am Fam Physician. 2016;94(2):106-113.
- McCartney CR, Marshall JC. Polycystic ovary syndrome. N Engl J Med. 2016;375:54-64.
- Alves AC, Valcarcel B, Mäkinen VP, Morin-Papunen L, Sebert S, Kangas AJ, et al. Metabolic profiling of polycystic ovary syndrome reveals interactions with abdominal obesity. Int J Obes. 2017;41(9):1331-1340.
- Zhang J, Bao Y, Zhou X, Zheng L. Polycystic ovary syndrome and mitochondrial dysfunction. Reprod Biol Endocrinol. 2019;17(1):1-5.
- Wild RA, Rizzo M, Clifton S, Carmina E. Lipid levels in polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril. 2011;95(3):1073-1079.
- Osibogun O, Ogunmoroti O, Michor ED. Polycystic ovary syndrome and cardiometabolic risk: Opportunities for cardiovascular disease prevention. Trends Cardiovasc Med. 2020;30(7):399-404.
- Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, et al. Polycystic ovary syndrome, insulin resistance, and obesity: navigating the pathophysiologic labyrinth. Int J Reprod Med. 2014;2014:1-17.
- Lim SS, Davies MJ, Norman RJ, Moran LM. Overweight, obesity and central obesity in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(6):618-637.
- Blumenfeld Z. The possible practical implication of high CRP levels in PCOS. Clin Med Insights Reprod Health. 2019;13:1-3
- Stępień M, Stępień A, Wlazeł RN, Paradowski M, Banach M, Rysz J. Obesity indices and inflammatory markers in obese non-diabetic normo- and hypertensive patients: a comparative pilot study. Lipids Health Dis. 2014;13(1):1-10.
- Ellulu MS, Patimah I, Khaza’ai H, Rahmat A, Abed Y. Obesity and inflammation: the linking mechanism and the complications. Arch Med Sci. 2017;13(4):851-863.
- Riaz M, Basit A, Fawwad A, Ahmadani AY, Zafar AB, Miyan Z, et al. Frequency of insulin resistance in patients with polycystic ovary syndrome: A study from Karachi, Pakistan. Pak J Med Sci. 2010; 26(4):791-794.
- Akram T, Hasan S, Imran M, Karim A, Arsalan M. Association of polycystic ovary syndrome with cardiovascular risk factors. Gynecol Endocrinol. 2010; 26(1):47-53.
- Stang J, Huffman LG. Position of the academy of nutrition and dietetics: Obesity, reproduction, and pregnancy outcomes. J Acad Nutr Diet.2016; 116(4):677-691.
- Fernström M, Fernberg U, Hurtig-Wennlöf A. Insulin resistance (HOMA-IR) and body fat (%) are associated to low intake of fruit and vegetables in Swedish, young adults: the cross-sectional lifestyle, biomarkers and atherosclerosis study. BMC Nutr. 2019;5(1):1-9.
- Repaci A, Gambineri A, Pasquali R. The role of low-grade inflammation in the polycystic ovary syndrome. Mol Cell Endo. 2011; 335(1):30-41.
- Kamath DY, Xavier D, Sigamani A, Pais P. High sensitivity C-reactive protein (hsCRP) and cardiovascular disease: An Indian perspective. Indian J Med Res. 2015;142(3):261-268.
- Dayal D, Jain H, Attri SV, Bharti B, Bhalla AK. Relationship of high sensitivity C-reactive protein levels to anthropometric and other metabolic parameters in Indian children with simple overweight and obesity. J Clin Diagn Res. 2014;8(8):5-8.
- Kalyan S, Goshtesabil A, Sarray S, Joannou A, Almawi WY. Assessing C reactive protein/albumin ratio as a new biomarker for polycystic ovary syndrome: a case–control study of women from Bahraini medical clinics. BMJ Open. 2018;8(10):1-7.
- Beatriz Motta A. The role of obesity in the development of polycystic ovary syndrome. Curr Pharmaceut Des. 2012;18(17):2482-24891.
- Flock MR, Green MH, Kris-Etherton PM. Effects of adiposity on plasma lipid response to reductions in dietary saturated fatty acids and cholesterol. Adv Nutr. 2011;2(3):261-274.
- Klop B, Elte JW, Cabezas MC. Dyslipidemia in obesity: mechanisms and potential targets. Nutrients. 2013;5(4):1218-1240.
- Al-Jefout M, Alnawaiseh N, Al-Qtaitat A. Insulin resistance and obesity among infertile women with different polycystic ovary syndrome phenotypes. Scientific Rep. 2017;7(1):1-9.
- Álvarez‐Blasco F, Luque‐Ramírez M, Escobar‐Morreale HF. Obesity impairs general health‐related quality of life (HR‐QoL) in premenopausal women to a greater extent than polycystic ovary syndrome (PCOS). Clin Endocrinol. 2010;73(5):595-601.
- Chiware TM and Ayers JWT. Body mass index and insulin resistance in polycystic ovarian syndrome. Fertil Steril. 2013;100(3):351-352.
- El-Mazny A, Abou-Salem N, El-Sherbiny W, El-Mazny A. Insulin resistance, dyslipidemia and metabolic syndrome in women with polycystic ovary syndrome. Int J Gynaecol Obst. 2010; 109(3): 239-241.
- Glueck CJ, Goldenberg N. Characteristics of obesity in polycystic ovary syndrome: etiology, treatment, and genetics. Metabol. 2019;92:108-120.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
