By Faiza Sharif, Ashfaq Ahmad, Syed Amir Gilani
AFFLIATIONS:
New Campus, the University of Lahore, Lahore, Pakistan.
ABSTRACT
Background: Lumbar Spinal stenosis is the narrowing of the spinal canal at any lumber level. Lumbar spinal stenosis has multiple severities and both conservative and operative treatment options. The objective of the current study was to compare the results of operative and conservative approaches in spinal stenosis treatment.
Methods: This cross-sectional study was conducted from January 2019 to June 2019. The data was collected from different hospitals in Lahore (Ittefaq, General, Jinnah, and Hameed Latif). Participants (n=121) of both genders, pre-diagnosed with Lumbar spinal stenosis and symptoms history of 10 weeks (confirmed on imaging) were included. Interventions were decompressive surgery and conventional conservative management. The outcome measures were body pain, functional activities, and the Oswestry Disability Index. An independent sample t-test was used to compare the results between the two groups. A p≤ 0.05 was considered statistically significant.
Results: The patients undergoing surgery had statistically significant (p=0.00) advantages of surgery compared to the non-surgical group at 3 months. The 25(36%) of patients remained the same after conservative treatment with 51(72%) having pain radiation and 47(66%) with neurological deficit. The effect of treatment for body pain was 7.8 (95%CI, 8.6, 6.9), physical function −1.3 (95%CI, −0.6, −2.2), and Oswestry Disability Index was −3.4 (95%CI, −2.7, −4.1).
Conclusion: Patients who had surgery of spinal stenosis showed marked improvements in body pains, functional activities, and Oswestry disability index compared to conservatively treated. Patients, health care providers, and other stakeholders may get benefit from the findings of this study.
Keywords: Spinal Stenosis; Laminectomy; Physical Therapy.
Lumbar Spinal stenosis is the narrowing of the spinal canal at any lumber level. This narrowing causes unrestricted pressure on peripheral nerves and spinal cord1 which in turn results in excruciating pain, numbness, and lower limb weakness2. Patients with lumbar spinal stenosis most often have lower back pain radiating into the leg, and these symptoms appear while walking. This pathology is degenerative and severely compromises normal functional activities, the ability to walk normally, and ultimately compromises the quality of life3.
Lumbar spinal stenosis has a wide range of treatment options because the disease has many levels of severities4. A comprehensive physical examination, physical manipulations, radiographic studies and imaging are of utmost importance in making clinical diagnosis5. At present, conservative management i.e. an important initial step in managing lumbar spinal stenosis, can give temporary relief for a short period of time6. Physical therapy management can help patients for up to six months or a year, despite its increasing use in recent years, the use of non-steroid anti-inflammatory medicines, pain killers and corticosteroid injections prove to be little beneficial7,8. Lumbar spinal stenosis has been labeled as are current indication for spine surgery in patients older than 60 years of age. Indications for spinal surgery seem to differ widely depending on the severity of symptoms. Patients having spinal stenosis usually are asymptomatic on radiographs, therefore careful screening of patients is an especially important and clinical correlation between radiographic findings and symptoms plays a key role in management9,10.
At present, patients with spinal stenosis have both surgical and non-surgical treatments available. The choice of surgical treatment depends on the patient’s quality of life and severity of stenosis6,11, whereas non-surgical conservative treatment is usually done to relieve major clinical symptoms of instability caused by degeneration, although it provides temporary relief to the patients. It can be complicated to decide which treatment is better than other12,13. Spinal surgery to treat spinal stenosis has been used extensively for the past few decades, therefore there are multiple complex surgical procedures14. The procedure of laminectomy to decompress neural structures has been increased in addition to lumbar fusion. This has reduced the risk of instability and deformity later in life. Lumbar fusion surgery is another surgical procedure, which is widely used now a day15.
However, it is very difficult to compare and conclude between these treatments because the diagnosis and treatment options are very intricate and these are based on decisions relying on the patient’s signs and symptoms, radiological findings, and comorbidities in every patient. The clinical guidelines of North American Spine Society (NASS) in 200816 described that no intervention for lumbar spinal stenosis is beneficial in improving a patient’s condition due to the natural disease history and also decompression surgery is more effective than other interventions in patients having moderate to severe symptoms of lumbar spinal stenosis17.
Surgery for lumbar spinal stenosis has been more effective as compared to conservative treatment, but up to the researcher’s knowledge, no such comparative studies have been done in Pakistan for the management of spinal stenosis. Therefore, this study aimed to compare the results of different operative and conservative approaches in the management and treatment of lumbar spinal stenosis.
This cross-sectional study was conducted from January 2019 to June 2019. The data was collected from different hospitals in Lahore (Ittefaq, General, Jinnah, and Hameed Latif) and compiled at the University of Lahore. The ethical review board of faculty of allied health sciences, University of Lahore approved the study. The study used a non-probability convenient sampling technique and a total of 121 participants of both genders, with neurogenic claudication of radiating pain in legs for at least 10 weeks were included in the study. Each patient signed informed consent. The radiographic findings also confirmed the diagnosis of spinal stenosis at one or multiple levels. The total sample was determined using the following equation, which kept the error margin equivalent to 5% and the significance level equal to 95%. Sample size calculation in the World Health Organization (WHO) edition 2.0.21 of the health studies by using 95% significance level, 1.76% population proportion and5%expected margin of error14. Patients with ankylosing spondylitis, spinal tumors, cauda equina and lumbar instability symptoms were excluded. The conservative management options were physical therapy, chiropractic, Nonsteroidal anti-inflammatory drugs (NSAIDs), epidural injections and analgesics.
The surgical procedure was posterior decompressive laminectomy and non-surgical procedure was “conventional care”, which included physical therapy, patient education, and a home exercise plan with the administration of NSAIDs if tolerated by the patients. The outcome measures were Short form survey (SF-36) body pain, functional activities and the Oswestry disability index measured at 3 months. The difference in the mean values changes from baseline between operative and conservative treatment groups. The SF-36 scores have a range of 0-100, with lower scores demonstrate more severe symptoms; the Oswestry Disability Index ranges from 0-100, with higher scores indicates higher severe symptoms. Treatment comparisons were made at the designated follow uptime. Data was collected through standard questionnaires3 months after treatment of surgical and conservative treatments and SPSS (Software Statistical Package for Social Science) version 24.0 was used as a statistical tool. An independent sample t-test was used to compare the treatment results between surgical and conservative groups. A p≤ 0.05 was considered statistically significant.
A total of 121 participants were divided into two groups, surgical group (50) and conservative non-surgical group (71). Most of the patients in both groups were males 50(70%). The mean age (SD) of surgical group was 64.7 years and the conservative group was 67.6 years with a mean body mass index (BMI) of 29.6 and 28.4 respectively. In both groups, patients had comorbid diseases like hypertension, diabetes, and osteoarthritis. Patients were unable to perform straight leg raise and pain radiating towards leg with 42(84%) positive Straight Leg Raise (SLR) and 47(94%) pseudoclaudication experienced surgery later. Since, n=61(86%) of the patients in the operative group had severe symptoms of lumbar spinal stenosis. The most common site for spinal stenosis was L4-L5. Interventions were posterior decompressive surgery and conventional conservative management. The outcome measures (Table 1) were body pain, functional activities and the Oswestry disability index measured 3 months after either treatment.
Table 1: Characteristics of patients describes the demographic details and comorbidities of the patients at baseline.
| Treatment Received | ||
| Characteristics | Operative (n=50) % | Conservative
(n=71) % |
| Mean age | 64.7 | 67.6 |
| Males | 35(70) | 50(70) |
| Marital status (married) | 44(88) | 66(92) |
| Work status | ||
| Full/part time | 8(16) | 7(10) |
| Retired | 38(76) | 55(78) |
| Disabled | 3(6) | 6(8) |
| Others | 1(2) | 3(4) |
| Body mass index (BMI)kg/m2 | 29.6 | 28.4 |
| Comorbidities | ||
| Hypertension | 33 (66) | 61(86) |
| Diabetes | 11(22) | 9(13) |
| Osteoporosis | 6(12) | 1(4) |
| Time since most recent pain>10 weeks | 36(72) | 44(62) |
| Satisfaction with symptoms – very satisfied | 39(78) | 48(68) |
| Outcome | ||
| Getting improved | 43(86) | 41(57) |
| Staying about the same | 5(10) | 25(36) |
| Getting worse | 2(4) | 5(7) |
| Pseudoclaudication if any | 47(94) | 38(54) |
| SLR or Femoral Tension | 42(84) | 33(47) |
| Pain radiation – any | 45(90) | 51(72) |
| Any Neurological Deficit | 43(86) | 47(66) |
Both groups had almost the same age group i.e., 64.7 and 67.6 respectively (Table 1) with a greater number of male patients in both groups. The patients receiving surgical treatments had severe pain, poor function and disability compared to the conservative group. Patients who had surgery were more satisfied with the improvement of their signs and symptoms when compared with the non-operative group. Level of stenosis among operative and conservative groups is shown in Figure 1.
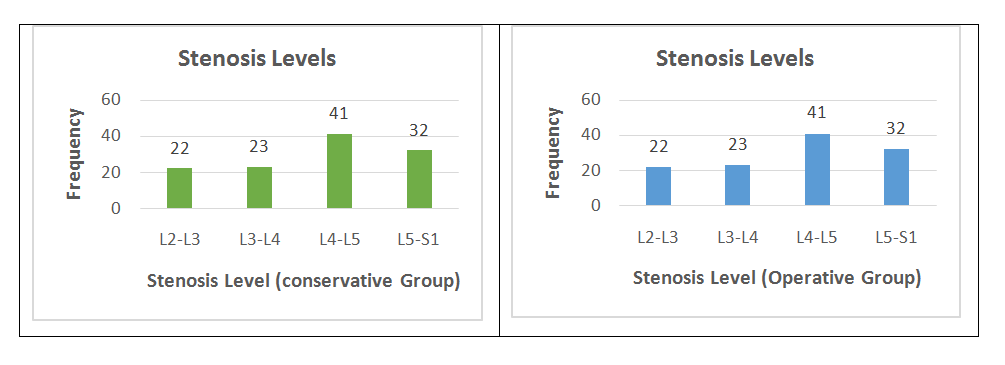
Figure 1: Level of stenosis among operative treatment group and conservative treatment group.
The mean time for lumbar surgery was 110 minutes. No significant difference was seen in the intraoperative complications. The most common postoperative complication was dural tear 5(10%). Intra-operative complications of aspiration, nerve root injury, vascular injury or surgical procedure at the wrong site were not reported. For 8 weeks post-operatively; (Table 2) none of the bone graft complications, leakage of CSF, nerve root injury, cauda equina injury were reported.
Table 2: Operative procedure and complications.
| Procedure | n=50 |
| Posterior Decompression laminectomy | 44(88%) |
| Surgery time | 110 mins |
| Laminectomy level | |
| L2-L3 | 1(2%) |
| L3-L4 | 7(14%) |
| L4-L5 | 41(82%) |
| L5-S1 | 1(2%) |
| Post-operative mortality (death within 3 months of the surgery) | 0(0%) |
| Intra-operative complications | |
| Dural tear/leakage of spinal fluid | 5(10%) |
| Other | 1(2%) |
| None | 44(88%) |
| Post-operative complications | |
| Wound hematoma | 1(2%) |
| Wound infection | 1(2%) |
| Others | 4(8%) |
Surgical patients had statistically significant effects in treatment than the conservative group for all outcome measures (Bodily Pain, Physical Function, and Oswestry Disability Index) (Table 3). Patients’ after 3 months postoperatively indicate major improvement in operative group as compared to the conservative group (p=<0.001).
Table 3: Analysis of outcome measures after 3 months of treatments received.
| Outcome Measures | Operative
(n=50) |
Conservative
(n=71) |
Effect of Treatment (95%CI) | p- Value |
| SF-36 Bodily Pain (BP)
(0-100) |
23.2 ± 2.3 | 15.4 ± 2.2 | 7.8(8.6, 6.9) | 0.00 |
| SF-36Physical Function (PF) (0-100) | 16.2± 2.3 | 17.6± 2.2 | −1.3(−0.6, −2.2) | 0.001 |
| Oswestry Disability Index (ODI) (0-100) | −16.1 ± 1.9 | −12.7 ± 1.8 | −3.4(−2.7, −4.1) | 0.00 |
The results of the present study showed that surgery is more effective than conservative management for spinal stenosis. These results are similar to a study carried out by A Delitto et al. which concluded surgery as a more effective treatment in terms of improvement in pain and physical function 4 years post-operatively19. Another randomized controlled trial was done to find the long-term results of lumbar spinal surgery which showed better results in pain reduction and function improvement postoperatively20.
However, a systematic review conducted by Zaina et al. concluded that it is not clear which treatment is better than the other in spinal stenosis management and surgical treatment, more over surgery has many side effects than conservative treatment. The above study results are in contrast to the current study21. Similarly, Masakazu and Minetama et al. conducted a study to find out the long-term comparative effects of surgical and conservative treatments for spinal stenosis and found out that there is no significant difference between both groups in all outcome measures except physical function 22,23.
Contrary to our study, Patel et al. found a significant role of conservative managements currently used to treat lumbar spinal stenosis. The conservative therapies having positive results include minimal invasive decompression and spinal cord stimulation. Drugs used to treat lumbar spinal stenosis such as systemic prostaglandin analogs and epidural drugs such as calcitonin showed early results but need further evaluation for clinical use24. Another contrasting study of this study was done by Oka et al. which compared the effectiveness of different conservative treatments (pharmacology, exercise, and acupuncture. They concluded that acupuncture is more effective than physical exercise and pharmacological treatment for lumbar spinal stenosis23.
However Jung et al. concluded in a prospective study that patients of lumbar spinal stenosis without any instability respond to conservative treatment and reported less pain and more functional improvement through 1 year as compared to surgical treatment25.
In lumbar spinal stenosis patients without instability, non-surgical treatment resulted in less pain improvement and functional recovery through 1 year. The limitations of this study were the small sample size and the follow-up time was also short. It is recommended to conduct more studies on a larger scale with a large sample size and follow-up time up to 4 years postoperatively to see the long terms advantages of surgical and conservative treatments for spinal stenosis.
Studies with detailed protocols and descriptions of non-surgical treatments are lacking in the literature. Research into treatment for lumbar spinal stenosis may be much improved by the development of standard diagnostic criteria and clinical outcomes. Most likely, the highest cost-effectiveness would be achieved, if the patient could be correctly selected for one or the other treatment option, which warrants further research on the identification of predictive factors for treatment success.
Surgical approaches have marked effects compared to conservative approaches in the treatment and management of Lumbar spinal stenosis. Patients who had surgery showed significant improvements in body pains, functional activities and the Oswestry disability index than patients who were treated conservatively. Patients, health care providers and other stakeholders would benefit from the findings of this study.
We are especially thankful to Ittefaq, General, Jinnah, Hameed Latif Hospitals for their assistance and facilitation in collecting the data.
The authors declare no conflict of interest.
The study was approved from the Faculty of Allied Health Sciences, The University of Lahore Ethical Review Committee (IRB-UOL-FAHS/725/2019).
Both verbal and written Informed consent was taken from all patients.
The study was conceived and designed by FS. She was also responsible for data collection, analysis, interpretation, manuscript writing, and data management. AA helped in writing this manuscript and monitored the accuracy and integrity of this article. SAG supervised and provided intellectual support for the manuscript conception and study design. He also critically analyzed the article.
- Siccoli A, Marlies P, Schröder ML, Staartjes VE. Machine learning–based preoperative predictive analytics for lumbar spinal stenosis. Neurosurg Focus. 2019; 46(5): E5:1-9.
- Lønne G, Fritzell P, Hägg O, Nordvall D, Gerdhem P, Lagerbäck T, et al. Lumbar spinal stenosis: comparison of surgical practice variation and clinical outcome in three national spine registries. Spine J. 2019;19(1):41-49.
- Lafian AM, Torralba KD. Lumbar spinal stenosis in older adults. Rheum Dis Clin. 2018; 44(3): 501-512.
- Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016; 352: h6234:1-13.
- Tobert DG, Harris MB. Degenerative lumbar spinal stenosis and spondylolisthesis. InPrinciples of orthopedic practice for primary care providers 2018 (pp. 47-59). Springer, Cham.
- Zweig T, Enke J, Mannion AF, Sobottke R, Melloh M, Freeman BJ, et al. Is the duration of pre-operative conservative treatment associated with the clinical outcome following surgical decompression for lumbar spinal stenosis? A study based on the Spine Tango Registry. Eur Spine J. 2017;26(2):488-500.
- Hammerich A, Whitman J, Mintken P, Denninger T, Akuthota V, Sawyer EE, et al. Effectiveness of physical therapy combined with epidural steroid injection for individuals with lumbar spinal stenosis: a randomized parallel-group trial. Arch Phys Med Rehabil. 2019;100(5):797-810.
- Minetama M, Kawakami M, Ishimoto Y, Nagata K, Teraguchi M, Kitagawa T, et al. Two-year follow-up of physical therapy versus surgical therapy for patients with lumbar spinal stenosis: GP077. Spine J Meet Abstr. 2017: p. 219.
- Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Eng J Med. 2016;374(15):1413-1423.
- Aichmair A, Burgstaller JM, Schwenkglenks M, Steurer J, Porchet F, Brunner F, et al. Cost-effectiveness of conservative versus surgical treatment strategies of lumbar spinal stenosis in the Swiss setting: analysis of the prospective multicenter Lumbar Stenosis Outcome Study (LSOS). Eur Spine J. 2017;26(2):501-509.
- Dobkin BH. Provocative walking test of strength for diagnosis, management, and outcome assessment of symptomatic lumbar spinal stenosis. Neurorehabil Neural Repair. 2019; 33(12):1003-1007.
- Pazarlis K, Punga A, Schizas N, Sandén B, Michaëlsson K, Försth P. Study protocol for a randomised controlled trial with clinical, neurophysiological, laboratory and radiological outcome for surgical versus non-surgical treatment for lumbar spinal stenosis: the Uppsala Spinal Stenosis Trial (UppSten). BMJ Open. 2019; 9(8): e030578:1-6.
- Weber C, Lønne G, Rao V, Jakola AS, Solheim O, Nerland U, et al. Surgical management of lumbar spinal stenosis: a survey among Norwegian spine surgeons. Acta Neurochir. 2017;159(1):191-197.
- Machado GC, Maher CG, Ferreira PH, Harris IA, Deyo RA, McKay D, et al. Trends, complications, and costs for hospital admission and surgery for lumbar spinal stenosis. Spine. 2017;42(22):1737-1743.
- Machado GC, Ferreira PH, Yoo RI, Harris IA, Pinheiro MB, Koes BW, et al. Surgical options for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016;11: CD012421.
- Watters III WC, Baisden J, Gilbert TJ, Kreiner S, Resnick DK, Bono CM, et al. Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008;8(2):305-310.
- Inoue G, Miyagi M, Takaso M. Surgical and nonsurgical treatments for lumbar spinal stenosis. Eur J Orthop Surg Traumatol. 2016; 26(7): 695-704.
- Amir Y, Halfens R, Lohrmann C, Schols J. Pressure ulcer prevalence and quality of care in stroke patients in an Indonesian hospital. J Wound Care. 2013; 22(5): 254-60.
- Delitto A, Piva SR, Moore CG, Fritz JM, Wisniewski SR, Josbeno DA, et al. Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Ann Intern Med. 2015;162(7):465-473.
- Brøgger HA, Maribo T, Christensen R, Schiøttz-Christensen B. Comparative effectiveness and prognostic factors for outcome of surgical and non-surgical management of lumbar spinal stenosis in an elderly population: protocol for an observational study. BMJ Open. 2018; 8(12): e024949:1-9.
- Zaina F, Tomkins‐Lane C, Carragee E, Negrini S. Surgical versus non‐surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016; (1):1-31.
- Minetama M, Kawakami M, Nakagawa M, Ishimoto Y, Nagata K, Fukui D, et al. A comparative study of 2-year follow-up outcomes in lumbar spinal stenosis patients treated with physical therapy alone and those with surgical intervention after less successful physical therapy. J Orthop Sci. 2018;23(3):470-476.
- Oka H, Matsudaira K, Takano Y, Kasuya D, Niiya M, Tonosu J, et al. A comparative study of three conservative treatments in patients with lumbar spinal stenosis: lumbar spinal stenosis with acupuncture and physical therapy study (LAP study). BMC Complement Altern Med. 2018;18(1):1-7.
- Patel J, Osburn I, Wanaselja A, Nobles R. Optimal treatment for lumbar spinal stenosis: an update. Curr Opin Anaesthesiol. 2017; 30(5): 598-603.
- Jung JM, Hyun SJ, Kim KJ, Kim CH, Chung CK, Kim KH, et al. A prospective study of non-surgical versus surgical treatment for lumbar spinal stenosis without instability. J Clin Neurosci. 2020;80:100-107.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
