By Zawwar Raza1, Zahid Mehmood1, Syed Asad Mehdi Rizvi2, Zoha Khan2, Imshaal Musharaf2, Shoaib Malik3, Abdul Rab1, Afrasiab Khalid2, Neyha Navaid2, Warisha Hanif2, Laiba Shamim2
- Surgical Ward, Jinnah Post Graduate Medical Centre, Karachi, Pakistan
- Jinnah Sindh Medical University, Karachi, Pakistan
- Anaesthesia Department, Jinnah Post Graduate Medical Centre, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-2/006
How to cite: Raza Z, Mehmood Z, Rizvi SAM, Khan Z, Musharaf I, Malik S, Rab A, Khalid A, Navaid N, Hanif W, Shamim L. Delay in management of Acute Peritonitis and its effect on 30-day mortality. Pak J Med Dent. 2024;13(2): 31-39. Doi: 10.36283/PJMD13-2/006
Background: Peritonitis is a grievous surgical emergency, characterized by the inflammation of the peritoneum and a major cause of morbidity and mortality in surgical situations. This study investigated the delayed presentation impact on 30-day mortality in emergency laparotomies for peritonitis patients in Karachi.
Methods: This longitudinal study was employed on 148 peritonitis patients at Jinnah Postgraduate Medical Centre, selected through non-probability convenient sampling. The study included secondary peritonitis-diagnosed patients of all ages and genders admitted from December 2022 to August 2023. Data encompassed pre-hospital experiences, care received at our center, and previous medical consultations. National Exploratory Laparotomy Audit (NELA) score estimated the 30-day mortality rate. SPSS version 26.0 was used, with qualitative variables presented as percentages and frequencies, considering p<0.05 significant.
Results: The majority of our patients were male 106(71.6%) with ages 19-30(41.2%). Among admitted patients, 59(40.3%) had primary education while 41(28%) had none, indicating educational disparities. Financial constraints were evident, with 45(30.2%) earning less than 15,000PKR monthly. The mean delay in presenting to the first practitioner was 2.98 days. Local general practitioners were consulted by 59.1% before reaching our facility. Total delay time correlated significantly with the NELA score (p<0.001). Extended travel distances (72.4% traveled far) correlated with delayed presentation (p=0.019). Differences in systolic blood pressure and respiratory rate were noted between mortality and non-mortality groups (p-value<0.05).
Conclusion: The study underscores the substantial contribution of delayed presentation to mortality in peritonitis patients undergoing emergency laparotomy. Addressing such issues could potentially enhance patient outcomes and reduce mortality in emergency surgeries.
Keywords: Peritonitis, General Surgery, Mortality, Morbidity, Laparotomy.
Peritonitis is defined as inflammation of the peritoneum. Bacterial peritonitis and intra-abdominal abscess are the two major manifestations of intra-abdominal infections. Peritonitis is a significant cause of morbidity and mortality in surgical settings1. The spectrum of causative factors of peritonitis is variable in different parts of the world2. Five billion people lack access to safe and affordable surgical care with the greatest burden falling on individuals from low-and middle-income countries. Only 6% of surgical procedures are performed in the poorest countries where 30% of the world’s population lives. The unmet surgical need is greatest in sub-Saharan Africa and South Asia3. Coexisting premorbid illness and postoperative complications were found to be associated with death3.
The Three Delays Model, originally developed in the context of maternal mortality in low-income settings, provides a useful framework to examine factors influencing the timeliness of care4. According to this model, adverse outcomes from complications are attributable to delay. The delays are classified into three categories: delay in decision to seek care, delay in reaching care, & delay in receiving adequate health care4.
Peritonitis can be diagnosed clinically, based mostly on history and physical examination. The main symptom in all cases is abdominal pain. These patients are managed surgically, and the time of intervention can vary depending on healthcare facilities, availability of resources, patients’ consent to surgery, etc. Many risk prediction tools have been developed (e.g., P-POSSUM, NELA risk score) to aid risk stratification by clinicians. According to the study by Azim et al, it was noted that NELA had an AUC of 0.861 and uses variables that are tested for every patient in our hospital setup. It uses multiple data points (including age, gender, physiological variables, malignancy, and ASA status) to estimate the probability of 30-day mortality status5.
The National Emergency Laparotomy Audit (NELA) is a scale that takes into account multiple variables, age, co-morbidities, and many other variables. NELA score is a risk calculation tool that estimates the risk of death within 30 days of emergency abdominal surgery. This was calculated using the NELA calculator and data for each of the NELA variables was collected from the emergency department. To calculate NELA scores, we also calculated the ASA scores. The ASA (American Society of Anesthesiology) score is a metric to determine if someone is healthy enough to tolerate surgery and anesthesia. Our study correlated NELA scores with 30-day mortality reported in our patient population.
However, after the intervention, its effects may be long-lived and can affect patients’ survival. For the above-said reason, a correlation between delay in management and mortality was assessed and gave us a better understanding of whether timely intervention can have an impact on patients’ mortality. This research evaluated the potential effect of delay to identify factors leading to it and investigated whether there is a perceptible difference in 30-day mortality rates based on the timing of the intervention.
In our research study conducted at the General Surgery wards of Jinnah Postgraduate Medical Centre, Karachi, from December 2022 to August 2023, we employed a longitudinal study. The inclusion criteria for this study were designated as diagnosed secondary peritonitis patients of all ages and genders who were admitted to Jinnah Postgraduate Medical Centre during the study period of 9 months. All patients with incomplete data, who did not consent to the study and those with immunodeficiency disorders were excluded, as well as those patients who died before or during surgical intervention. We used non-probability convenient sampling. Ethical approval was taken from the Institutional Review Board and Ethical Committee in document NO.F.2-81/2023-GENL/168/JPMC. Informed consent was taken from all patients. A sample size of 148 was calculated using the WHO sample size calculator.
Data collection involved gathering information from patients hospitalized with clinical peritonitis, focusing on their history, examination findings, symptom onset, factors causing delay in seeking and getting healthcare, and disease prognosis. Each admitted post-operative patient was interviewed regarding the course of the disease and the relevant timeline to estimate each delay. A detailed history regarding each potential variable such as visiting quacks and their experience at the neighborhood clinic was documented via these interviews. Emergency room vitals, sub-vitals, and biochemical analyses from labs were collected from the emergency department at JPMC. A 30-day follow-up call was also made to each patient or his attendant to enquire about mortality and subsequently, the patients were divided into two groups as per their 30-day mortality status on the follow-up call.
The first delay that needs to be accounted for is from the start of the symptoms to finally deciding to seek care. After the decision to go to a medical practitioner is finalized, the patient needs to decide upon the logistical framework to start the required amount of care. A few such measurable variables include the expected transportation to the hospital, financial restraints, etc. In this regard, we inquired the patients regarding when they decided to seek care, and the day they went to reach a medical practitioner. The difference between these was counted as the logistical delay.
Delay in reaching care was the total number of days between the first point of care and the time the surgery was performed. The third delay which is due to ineffective healthcare practices is studied at two separate levels, The first of it when the patient goes to a local medical practitioner and keeps on receiving care that isn’t relevant. Delay in receiving care after reaching a tertiary care setup was measured as the total number of hours between the time the patient reached the hospital and the time the patient was admitted to the operating theater.
The National Emergency Laparotomy Audit (NELA) scale was used and the NELA score served as a risk calculation tool to estimate the risk of death within 30 days of peritonitis intervention through laparotomy. NELA score was calculated after the patient underwent laparotomy using their presentation vitals and investigation results.
The collected data was analyzed using SPSS version 26.0, with qualitative variables presented as percentages and frequencies in tables. We assessed associations using the most relevant statistical analysis, considering a significance level of p-value<0.05. The tests used were the Chi-square test and logistic regression when the dependent variables recorded were qualitative. Linear regression was used when both variables were quantitative. In cases where the dependent variable was quantitative and the independent was qualitative, we applied t-test and ANOVA if responses weren’t dichotomous. In the case of the dependent variable being qualitative and the independent being quantitative, we used logistic regression.
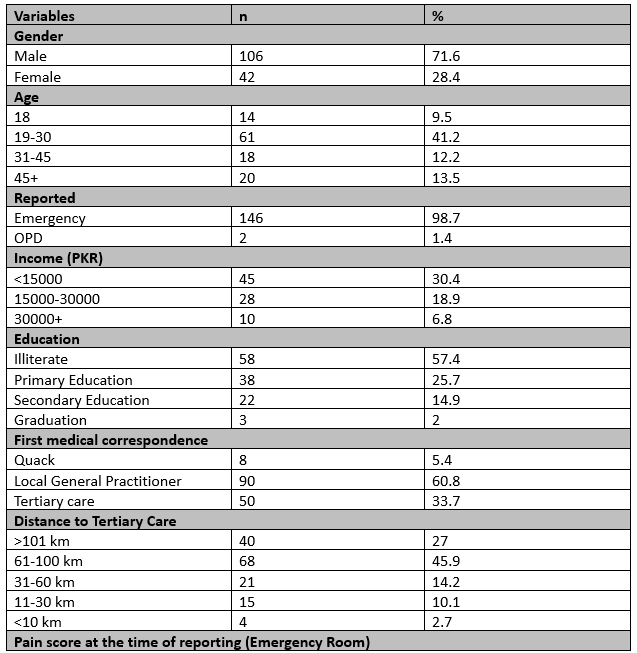
A total of 148 patients diagnosed with peritonitis were included in the study, composed of 106 males (71.6%) and 42 females (28.4%). The majority of our patients were between the ages of 19-30 (41.2%). Among the admitted patients, a considerable portion of 58 patients (57.4%) did not receive any sort of education, 38 patients (25.7%) had only attended school, and 22 patients (14.9%) completed school while only 2 patients (2%) pursued further education. The prevalence of educational disparity was evident through this. A pattern of financial constraints was seen, with 45 patients (30.4%) earning less than 15,000 PKR monthly in contrast to only 10 patients (6.8%) earning more than 30,000 PKR.
Table 1: Demographic details of the patients.

Upon presentation, the mean systolic blood pressure was approximately 109.05±15.78 mmHg, diastolic blood pressure was around 71.41±20.26 mmHg, and the mean respiratory rate was about 21.97±7.79 breaths per minute. We also collected data from past medical records regarding the patient’s vital when they reported to an emergency, the mean Hemoglobin was approximately 12.87±11.85, TLC was around 10.61±7.44, and the mean Platelet count was about 250.89±143.21.
Amongst all these variables the mean value of urea (p=0.030) and creatinine (p=0.049) was found to be significantly different in the mortality group vs non mortality group. The mean systolic blood pressure was found to be 99.24 in the non-mortality group and 111 in the mortality and this mean difference was also found to be statistically significant with a p-value of 0.04. Except for creatinine, all the variables are part of the NELA calculation, and is already established that they affect mortality. However, more information regarding creatinine as a predictor of mortality in these patients can be looked into.
A statistically significant (p<0.05) difference was found amongst patients in the mortality group and non-mortality group with a mean respiratory rate of 27.56 and 22.52 respectively. A mean difference of 16.05 bpm was found to be statistically significant (p=0.004) between the mortality and non-mortality groups.
Table 2: Descriptive analysis of laboratory investigations.

The mean number of days in the first delay was reported to be 2.98 days. Variables that affect the first delay include financial, educational, perception of pain, and other social variables. After deciding to seek care, the logistical challenges that arose had a mean difference of 12.72 hours was found between the decision to seek care to reach the health facility of choice. These logistical delays were found to have a statistically significant correlation (p-value 0.035) with NELA scores of the patient with a Pearson correlation giving a r value of 0.177.
Multiple factors such as the travel time to the nearest possible healthcare professional were documented. The mean travel time was reported to be 14.72 minutes, which in itself reflects the availability of health facilities in our region. Distance to tertiary care and mode of transport as factors affecting included logistical delay.
The mean cost of consultation was PKR 543.38. All these neighborhood doctors prescribed medications to each patient. When inquired regarding the cost of medication that was spent, the median cost was PKR 3500. The mean number of doses administered was 5.46. It was reported that 29 patients experienced relief in pain from the medication given by their local GP while 57 reported no improvement from it.
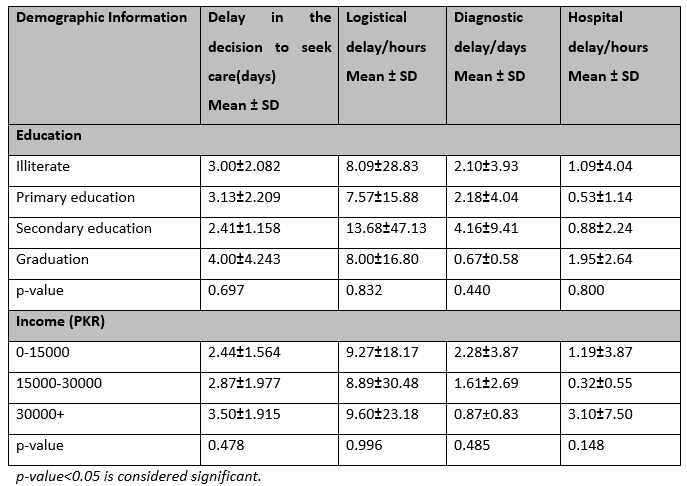
Table 3: Demographic Variables and their respective delay durations.
A total of 98(65.3%) patients went to neighborhood care before coming to our center. It was in 80(53.3%) cases that the doctor himself referred the patient to a tertiary care center, the rest of the patients eventually decided to visit a tertiary care center due to eventual no improvement in symptoms. All of this further increased the delay in seeking an appropriate level of care. Half of the patients who reported to emergency were given an expected waiting before the surgery could take place, the mean waiting time was 1.01 hours. 6(11.6%) of these patients were again rescheduled of surgery time assigned earlier. It was only after an average of 2.42 days after their first consultation that they came to our Centre where they were diagnosed and operated on. The median distance was 22km and we had a higher value going as far as 700km which shows how far the patient had to go for a disease that required immediate intervention. The mean cost of traveling was Rs. 4156.55 and the median was PKR 1000. The delay in surgery after reaching the relevant location of care in our study population was 1.79±4.22 hours.

Figure 1: Impact of the delays on the mortality, morbidity, and recovered groups.
The Mean±S.D of the NELA score in our sample was 7.73±13.54. The minimum NELA score was 0.08 while the maximum it went onto was 72.90.
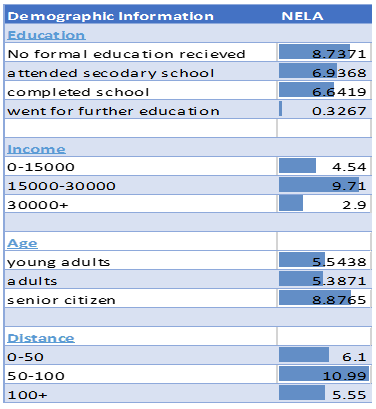
Figure 2: Association of NELA Score with demographic variables of participants
Our observations noted that the most common reason for patients undergoing exploratory laparotomy due to peritonitis was secondary to hollow viscous perforation with the most common being ileal perforation i.e., 55 patients (36.9%) followed by gastric perforation in 20 patients (13.4%) and duodenal in 16 patients (10.7%). This is comparable to other studies in the subcontinent which showed ileal perforation and duodenal perforation to the two most common 6,7. Our study tried to identify many factors that contributed to the delayed presentation of peritonitis using the 3 factors delay model. (Figure 3)
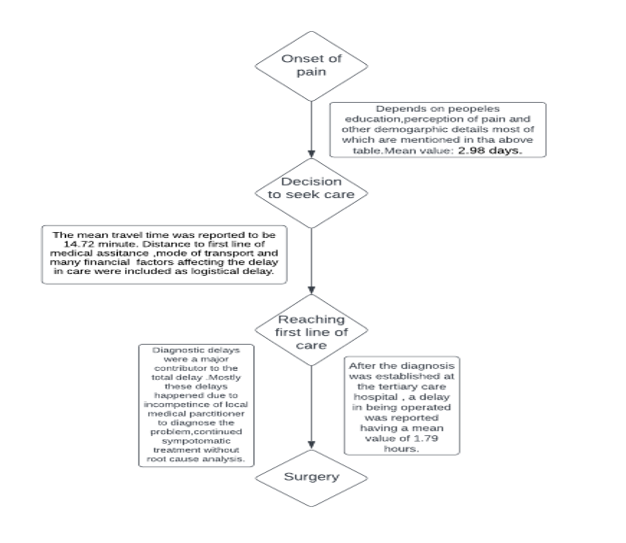
Figure 3: The three-factor delay model.
Factors that led to delay in seeking care were lower monthly income, low education level, and careless attitude towards their health. The majority of our patients were uneducated (57%) or had only completed secondary school (38%). Multiple studies found that individuals with lower levels of education were more likely to delay seeking treatment (estimated odds ratio of 11.72), suggesting that lack of education could contribute to a lack of understanding about their illness and the importance of early treatment8,9. The majority of our patients belonged to a lower socioeconomic group (45%) and increased mortality was associated with lower household income.
The second type of delay is referred to in our study as logistical delay. As shown, more than half of the people in our patient population were from a financial background that had less than PKR 15000 monthly household income which equates to less than 1 dollar per day in a family. Travel distance and cost were the most significant factors that contributed to delay in reaching care. 32.8% of patients reported that they traveled “very far” to reach the hospital. The mean distance traveled by our patients was 83.79 km. The most common means of transport was the use of an ambulance (59.5%). It is pertinent to note that increased travel distance would lead to increased travel costs with the mean travel cost being PKR 4156. A study from Uganda showed an association between the delay in reaching Tuberculosis (TB) treatment and travel time. At a median distance driving time of about 47 minutes, it represented an additional delay of about 12 days, increasing the mean delay time of 40 days to approximately 52 days10.
The economic burden introduced by travel, in the form of transport fees and lost work time, contributes to the second delay. This is especially evident in a systemic review by Herbet al. citing delays in access to surgical cancer care, which often proves to be expensive11. The third delay tends to happen after the patient is present in a healthcare facility and is delayed because of doctors’ decisions, whether it be a delay in diagnosis or management. This delay can include multiple factors such as incompetent neighborhood care, misdiagnosis from the first point of care, quacks, and the attitude that focuses merely on symptomatic care without finding/fixing the root pathology and this delay was a major contributor to mortality. In our study, a common theme among most mortality patients was how long they were being treated symptomatically by local GP without proper diagnosis.
The third delay for peritonitis was classified as ‘‘met’’ by the Logs target if conducted within 2 h or less after arriving at the hospital or as ‘‘not met’’ if performed in more than two hours. Only 26(22.6%) of the patients can be classified as met while 89(77.45%) were not met3. The study by Ahmajarvi et al. also shows a similar trend, it reported that the diagnostic delay in primary care usually occurs as an organizational delay from first contact to correct diagnosis, meaning it surely contributes to the third delay12. Similar findings were seen in an Indonesian study, where a healthcare system delay (median of 49 days from first symptoms to diagnosis) was significantly longer than patient delay13. A systematic review confirmed that both patient delay and health system delay for Tuberculosis diagnosis, in both low- and high-income countries, can be similar in length, again emphasizing the importance of healthcare system-related delays in the diagnostic process14.
Descriptive data regarding the delay due to local general practitioners showed that most of them did not refer the patient to a tertiary care center. Statistically speaking, in our study, logistical delay correlated with mortality despite diagnostic delay being the biggest contributor to it. The mortality reported for secondary peritonitis in the literature varies. Desa and Mehta reported a mortality of 24.8%, while Angelo Nespoli reported it to be 20.5%15. A similar mortality was seen by Memon et al. at 16.7%16. In a study by Tolonen et al, a mortality of 14.5% was noted17. In our study, a mortality of 22.3% was reported. The delayed presentation was found to be a significant contributor to mortality in a case series of patients undergoing emergency surgery for caecal volvulus, in which mortality was seen more in cases of bowel perforation18. We also found out that the concentration of urea and creatinine also varied significantly between the patients who lived and those who were in the mortality group. This is similar to studies done in the continent which found the same results19,20,21. Another study focusing on lactate as a predictor of ICU stay and postoperative mortality and morbidity found it to be associated with mortality which could be used in a follow-up study22.
Several studies have utilized the National Emergency Laparotomy Audit (NELA) score to evaluate postoperative mortality after emergency laparotomy. An Australian study compared the utility of the NELA risk prediction calculator with ACS calculators, finding NELA to be highly sensitive and useful in predicting 30-day mortality, with comparable performance to ACS. The Hellenic Emergency Laparotomy Study compared outcomes in Greece to NELA results, revealing similar demographics and preoperative risk factors but markedly worse mortality in Greek patients (16.3% vs 8.7%). This indicates the possible underutilization of critical care in Greece. However, we found that NELA scores to be significantly higher in the mortality group vs non mortality group which shows that NELA can be a good source of predicting mortality. Many studies have been done that have focused on the use of scoring systems to identify mortality, as seen in this study done in India and another in Nepal which focused on the Mannheim Peritonitis Index22.
Our study data was collected in the ward and many patients who may have died before reaching the facility or in the emergency department were not documented. A few patients expired after surgery and their data was collected from the hospital’s mortality record. Data regarding the description of delay was barely collected from such early mortalities. Few patients were lost to follow-up.
Peritonitis remains a major cause of morbidity and mortality. This research gives prominence to the delayed presentation as a factor that significantly increases mortality in peritonitis patients undergoing emergency laparotomy. There isn’t a specific study that correlates the 3-factor delay model with 30-day mortality for peritonitis patients. This is a first-of-its-kind study. We found out that delay in the management of peritonitis has a statistically significant effect on mortality. Logistical delays, especially related to accessing healthcare facilities, emerged as critical factors while diagnostic and hospital delays played a role as well. Addressing the issues could potentially enhance patient outcomes and reduce mortality in emergency surgeries.
None
There was no conflict of interest among the authors.
Ethical approval was taken from the Institutional Review Board and Ethical Committee in document NO.F.2-81/2023-GENL/168/JPMC.
ZM: Supervision, ZR: Ideation and focal person, SAMR: Statistical Analysis and write-up focal, ZK, IM: Writing and Data Collection, AK: Questionnaire Design and Data Collection, and NN, WH, LS: Data Collection and follow-up calls.
- Kumar D, Garg I, Sarwar AH, et al. Causes of Acute Peritonitis and Its Complication. Cureus. 2021;13(5):e15301. https://doi.org/10.7759/cureus.15301
- Sharma L, Gupta S, Soin AS, Sikora S, Kapoor V. Generalized peritonitis in India—The tropical spectrum. The Japanese journal of surgery. 1991;21(3):272-277. https://doi.org/10.1007/BF02470946
- Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624. https://doi.org/10.1016/s0140-6736(15)60160-x
- Actis Danna V, Bedwell C, Wakasiaka S, Lavender T. Utility of the three-delays model and its potential for supporting a solution-based approach to accessing intrapartum care in low- and middle-income countries. A qualitative evidence synthesis. Glob Health Action. 2020;13(1):1819052. https://doi.org/10.1080/16549716.2020.1819052
- Eugene N, Oliver CM, Bassett MG, et al. Development and internal validation of a novel risk adjustment model for adult patients undergoing emergency laparotomy surgery: the National Emergency Laparotomy Audit risk model. Br J Anaesth. 2018;121(4):739-748. https://doi.org/10.1016/j.bja.2018.06.026.
- Afridi SP, Malik F, Ur-Rahman S, Shamim S, Samo KA. Spectrum of perforation peritonitis in Pakistan: 300 cases Eastern experience. World J Emerg Surg. 2008;3:31. https://doi.org/10.1186/1749-7922-3-31
- Yadav D, Garg PK. Spectrum of perforation peritonitis in delhi: 77 cases experience. Indian J Surg. 2013;75(2):133-137. https://doi.org/10.1007/s12262-012-0609-2
- Obsa MS, Daga WB, Wosene NG, et al. Treatment seeking delay and associated factors among tuberculosis patients attending health facility in Ethiopia from 2000 to 2020: A systematic review and meta-analysis. PLoS One. 2021;16(7):e0253746. https://doi.org/10.1371/journal.pone.0253746
- Absa MS, Daga WB, Gebremedhin TD, et al. Treatment seeking delay and associated factors among tuberculosis patients attending health facility in Ethiopia from 2000 to 2020: A systematic review and meta-analysis. PLoS One. 2021;16(7):e0253746. doi: 10.1371/journal.pone.0253746
- Fluegge K, Malone LL, Nsereko M, et al. Impact of geographic distance on appraisal delay for active TB treatment seeking in Uganda: a network analysis of the Kawempe Community Health Cohort Study. BMC Public Health. 2018;18(1):798. https://doi.org/10.1186/s12889-018-5648-6
- Herb J, Shell M, Carlson R, Stitzenberg K. Is long travel distance a barrier to surgical cancer care in the United States? A systematic review. Am J Surg. 2021;222(2):305-310. https://doi.org/10.1016/j.amjsurg.2020.12.005
- Ahmajärvi K, Isoherranen K, Venermo M. Cohort study of diagnostic delay in the clinical pathway of patients with chronic wounds in the primary care setting. BMJ Open. 2022;12(11):e062673. https://doi.org/10.1136/bmjopen-2022-062673
- Handayani K, Sitaresmi MN, Supriyadi E, et al. Delays in diagnosis and treatment of childhood cancer in Indonesia. Pediatr Blood Cancer. 2016;63(12):2189-2196. https://doi.org/10.1002/pbc.26174
- Sreeramareddy CT, Panduru KV, Menten J, Van den Ende J. Time delays in diagnosis of pulmonary tuberculosis: a systematic review of literature. BMC Infect Dis. 2009;9:91. https://doi.org/10.1186/1471-2334-9-91.
- Khan PS, Dar LA, Hayat H. Predictors of mortality and morbidity in peritonitis in a developing country. Ulus Cerrahi Derg. 2013;29(3):124-130. https://doi.org/10.5152/ucd.2013.1955
- Memon AA, Siddiqui FG, Abro AH, Agha AH, Lubna S, Memon AS. An audit of secondary peritonitis at a tertiary care university hospital of Sindh, Pakistan. World J Emerg Surg. 2012;7:6. https://doi.org/10.1186/1749-7922-7-6
- Tolonen M, Sallinen V, Mentula P, Leppäniemi A. Preoperative prognostic factors for severe diffuse secondary peritonitis: a retrospective study. Langenbecks Arch Surg. 2016;401(5):611-617. https://doi.org/10.1007/s00423-016-1454-8
- Sylvester KR, Ooko PB, Mwachiro MM, Parker RK. Cecal volvulus in rural Kenya: delayed presentation contributes to high mortality. BMC surgery. 2021;21:1-7. https://doi.org/10.1186/s12893-021-01416-8
- Singh R, Kumar N, Bhattacharya A, Vajifdar H. Preoperative predictors of mortality in adult patients with perforation peritonitis. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2011;15(3):157. https://doi.org/10.4103/0972-5229.84897
- Rai A, Huda F, Kumar P, David LE, Chezhian S, Basu S, Singh S. Predictors of Postoperative Outcome in Emergency Laparotomy for Perforation Peritonitis; a Retrospective Cross-sectional Study. Archives of Academic Emergency Medicine. 2022;10(1). https://doi.org/10.22037/aaem.v10i1.1827
- Yan YX, Wang WD, Wei YL, Chen WZ, Wu QY. Predictors of mortality in patients with isolated gastrointestinal perforation. Experimental and Therapeutic Medicine. 2023;26(6):1-9. https://doi.org/10.3892/etm.2023.12255
- Negi R, Bhardwaj S, Singh S, Gupta S, Kaushik R. Peritonitis‐associated hyperlactatemia for evaluating mortality in secondary peritonitis. ANZ Journal of Surgery. 2020;90(12):2463-2466. https://doi.org/10.1111/ans.16278
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
