By Hudaibiya Ayub1, Bashir A. Soomro1, Rida Younis1, Maha Ali1, Hira Fatima1, Inayat Ali Khan1
1Dr. Ziauddin Hospital, Karachi
DOI: https://doi.org/10.36283/PJMD13-2/011
How to cite: Ayub H, Soomro BA, Younis R, Ali M, Fatima H, Khan IA. ASPECTS and Functional Outcomes in Left versus Right Hemisphere Strokes: A Prospective Cohort Study. Pak J Med Dent. 2024;13(2): 67-73. Doi: 10.36283/PJMD13-2/011
Background: Stroke presents as the second most prominent factor contributing to global mortality. Immediate brain imaging can be valuable for assessing functional recovery potential. This study investigated the association between Alberta Stroke Program Early CT Score (ASPECTS) and functional outcomes in patients with left and right-hemisphere strokes.
Methods: A prospective cohort study was conducted in July-Dec2 022, at a tertiary care hospital in Karachi including patients of either gender presenting within 2 days of stroke while excluding posterior circulation strokes, TIA & unwilling patients using a non-probability consecutive sampling technique. A total of 152 patients with acute ischemic stroke involving anterior circulation were analyzed and patients were categorized into two groups: the left hemisphere group (n=76) and the right hemisphere group (n=76) accordingly. ASPECTS scores were calculated from brain CT scans, while functional outcomes were measured using the modified Rankin Scale (mRS) at the three-month mark. Descriptive analysis and chi-square test were applied using SPSS vr25.
Results: Patients (n=152) had a mean age of 61.75 ± 13 years, with males comprising 67% of the cohort. ASPECTS scores were notably higher in left hemisphere strokes (median 9, IQR 2) than right hemisphere strokes (median 8, IQR 3) (p=0.036). Higher ASPECTS scores (≥7) correlated with improved outcomes (mRS ≤2) in both hemispheres. There was no statistically significant difference in both groups’ functional outcomes (p=0.182).
Conclusion: ASPECTS predicts functional outcomes in acute ischemic strokes equally well regardless of the affected hemisphere.
Keywords: Middle Cerebral Artery Infarction, Ischemic Stroke, Recovery of Function.
Stroke represents a significant contributor to lasting disabilities and stands as the second most prominent factor contributing to global mortality1. Ischemic strokes, caused by disruption of cerebral blood flow, account for the majority of stroke cases2. The symptoms of a stroke can manifest rapidly, indicating a focal or widespread disturbance of cerebral function3. A significant differentiating factor between a stroke and a transient ischemic attack (TIA) is that stroke symptoms last longer than 24 hours, while TIA symptoms usually resolve within this timeframe. Moreover, a stroke often results in more severe and long-lasting neurological deficits than a TIA. While seizures, migraines, or psychosis can have stroke-like symptoms, they stem from different underlying causes and are present with unique distinguishing features. An exhaustive medical examination and diagnostic testing are essential to diagnose the cause of these symptoms accurately4. Early identification and management of ischemic changes are critical to improve outcomes, yet the 30-day mortality rate for ischemic strokes remains around 15%5. Early identification and management of ischemic changes are critical to improve patient outcomes. In Pakistan, the incidence of strokes varies by age and gender, with a peak rate of 584,000 per 650,000 cases in individuals aged 75-85 years old between 2000 and 20166.
Imaging the brain shortly after a stroke is valuable for assessing functional recovery potential. Computed tomography (CT) scans currently represent the first-line imaging choice for acute stroke patients7-10. The Alberta Stroke Program Early CT Score (ASPECTS) is widely used to evaluate early ischemic changes in acute stroke cases, with scores above seven indicating a positive prognosis11. ASPECTS has been employed in various stroke studies, guiding decisions on recanalization therapy and predicting patient outcomes regardless of the treatment method12. The ASPECTS is a 10-point scoring system used in neurology to assess early ischemic changes on brain scans for stroke treatment. It involves specific regions of the Middle cerebral artery (MCA) territory and deducts points for observed abnormalities in these regions. An ASPECTS score of ≤7 is associated with a poor functional outcome at 3 months and an increased risk of symptomatic hemorrhage13. Though ASPECTS is associated with functional outcomes regardless of treatment, the prognostic value based on the hemisphere affected remains unclear14. Some studies suggest worse outcomes in right hemisphere strokes, but evidence conflicts.
This study described ASPECTS’ ability to distinguish left/right hemisphere outcomes that may streamline prognosis and care. Comparing ASPECTS scores/outcomes between hemispheres may reveal insight for individualized rehabilitation/treatment matching location/severity. Also, to determine if ASPECTS predicts outcomes differently by hemisphere to refine its prognostic role. This study investigated whether ASPECTS scores differ between left and right hemisphere strokes and whether these scores predict functional outcomes differently based on the hemisphere affected.
This was a prospective cohort study conducted at the Department of Neurology in a tertiary care hospital in Karachi, Pakistan. The study received ethical approval from the Ethical Review Committee of Dr. Ziauddin University. (Reference Code: 5380522HANEU).
The target population was stroke patients aged 18 years and older. During the study, which lasted for six months (July 2022 – Dec 2022), ASPECTS scores were calculated at the time of patient presentation with stroke. Additionally, the modified Rankin Scale (mRS), which determined the functional outcome, was calculated during a follow-up at the three-month mark. The sample size was calculated WHO calculator with an absolute precision of 10%. The calculated sample size is 152 based on the good three-month outcome in the left and right hemispheres keeping a 95% confidence level dividing the groups by 76 patients in each group. A non-probability consecutive sampling technique was utilized.
The inclusion criteria comprised cases of either gender with anterior circulation stroke (as primary aspects were only designed for anterior circulation and a modified score is applied for posterior circulation), presenting to the hospital within 2 days of stroke onset, and not having a previous history of stroke, patients who died were also included in the study. Exclusion criteria included non-consenting patients, posterior circulation stroke cases, transient ischemic attack patients with no significant findings on imaging, and those undergoing mechanical thrombectomy (as this can influence outcomes) or lost to follow-up.
After obtaining informed consent, patient data was collected. This included history (including age, gender, and marital status), clinical examination, Glasgow Coma Scale (GCS) assessment, and non-contrast CT scan as part of the initial stroke workup. ASPECTS scores were calculated based on early ischemic CT scan changes by the principal investigator which were cross-checked by a certified neurologist. The National Institutes of Heart Stroke Scale (NIHSS) was excluded as it was not considered for this study. The modified Rankin Scale (mRS) score was assessed at 90 days follow-up in person to evaluate functional outcomes by the principal investigator under the supervision of a certified neurologist. Patients were divided into left and right-hemisphere stroke groups based on involvement.
Statistical analysis was performed using SPSS version 25. Descriptive analyses used mean, standard deviation, percentages, and frequencies. Chi-square tests analyzed relationships, while logistic regression assessed associations. A p-value ≤ 0.05 indicated statistical significance.
In this study of 152 stroke patients, the mean age was 61.75±13 years, with the majority falling between 62-71 years. Male patients constituted 67% of the participants. The average weight was 69.1±11.7 kg, and the mean BMI was 26.9±6 kg/m2. The patients were equally divided into left and right-hemisphere stroke groups, with 76 patients in each. Left-sided strokes had higher ASPECTS scores compared to right-sided strokes, with a statistically significant difference (p=0.036). However, other baseline variables, including ICU and hospital stay duration and rehabilitation, showed no significant differences between the two groups. The overall mortality rate was 4.5%, with no significant difference between left and right hemisphere strokes. The ASPECTS score analysis reveals that 94 patients (61.8%) exhibited a significant enhancement in their functional outcomes, marking a notable improvement. Conversely, 58 patients (38.2%) experienced a less favorable trajectory, resulting in a decline in their functional well-being.
Table 1: Baseline demographics of stroke patients (n=152)
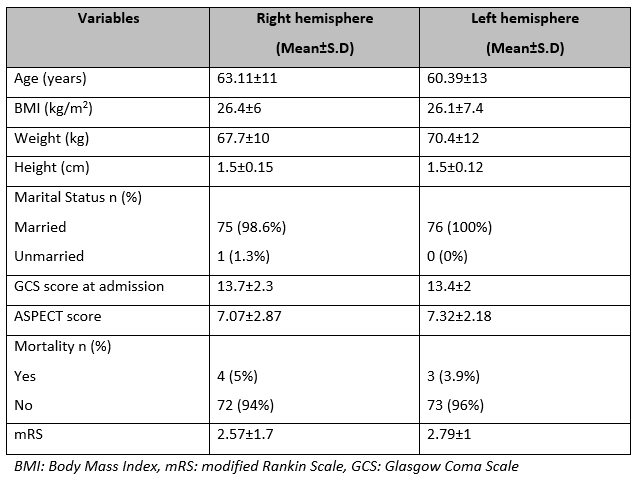
Table 1 summarizes the baseline demographics of stroke patients, with data separated by affected hemisphere. The results show that there are slight differences between the right hemisphere and left hemisphere stroke patients in terms of age, BMI, weight, height, GCS score at admission, ASPECT score, mortality rates, and mRS scores. However, these differences are generally small and not necessarily clinically significant.
Table 2: Baseline Characteristics and Outcome of Left vs Right Hemisphere Strokes (n=76)

Table 2 compares baseline characteristics and outcomes between left and right hemisphere strokes in stroke patients (n=76). the table indicates that there are significant differences in ASPECTS score between left and right hemisphere strokes (p=0.038), while other variables such as age, BMI, GCS at admission, duration of ICU stay, duration of hospital stay, and rehabilitation show no significant differences between the two groups.
Table 3: Classification of patient outcome according to the side of brain involvement (n=76)
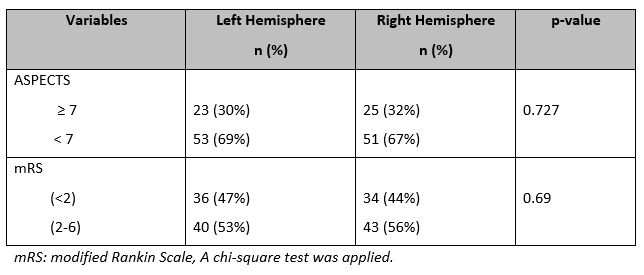
Table 3 compares patient outcomes based on left and right hemisphere involvement in 76 patients. It shows percentages for ASPECTS score (≥ 7 and < 7) and mRS score (< 2 and 2-6), with no significant differences found between the two hemispheres (p > 0.05). This suggests similar outcomes regardless of the side of brain involvement.

Figure 1: Outcome of ASPECTS score in Left & Right Hemisphere Strokes (Good ASPECTS: ≥ 7, Worse ASPECTS: <7)
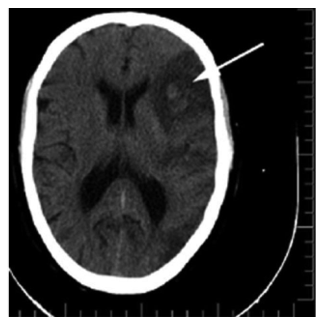
Figure 2: ASPECTS on this slice count to 6, however further slices are needed for complete quantification15.
ASPECTS is considered to be a robust clinical tool as it has exceptional reliability in the clinical setting. Pexman et al showed in their study that good to excellent reliability can be attained with ASPECTS when the symptom side of stroke is known16. While ASPECTS remains useful for predicting overall stroke prognosis, our findings suggest it may predict outcomes similarly for left and right hemisphere strokes. In our study, the results indicate that higher ASPECTS scores (≥7) are associated with better functional outcomes (mRS ≤2) in both left and right hemisphere strokes, which is consistent with other studies’ findings 16-18. However, the relationship between stroke laterality and outcomes appears complex, with evidence on this topic remaining mixed.
It has been suggested in some studies that right-hemisphere strokes may lead to worse functional outcomes or greater impairments in domains like mood and spatial skills compared to left-hemisphere strokes, our study did not find a significant difference in overall outcomes between the hemispheres19,20. Also, the difference in functional outcomes was not statistically significant (p=0.182) in left vs right hemisphere strokes. A larger proportion of left-hemisphere stroke patients achieved a good outcome (mRS ≤2) compared to right-hemisphere patients (67% vs 56%), but this difference was not large enough in this study to be statistically significant. Other variables like age, gender, and hospital stay duration did not differ significantly between the two groups. GCS scores varied between left and right hemisphere strokes, with the lowest GCS scores associated with poorer outcomes in both groups. Several factors may have contributed to this. First, laterality effects likely depend on the specific region or lobe affected rather than just the broad categorization of left vs right hemispheres. For example, right frontal lobe strokes may impact function differently than right parietal or occipital strokes. Second, individual patient characteristics like age, comorbidities, and stroke severity influence prognosis and were not fully accounted for in our study.
Other factors, such as the size and location of the infarct, the presence of other comorbidities, and the individual characteristics of the patients, may also influence functional outcomes and should be considered in clinical practice. Additionally, the prognostic value of ASPECTS in predicting functional outcomes highlights its utility as a bedside tool for guiding clinical decision-making and optimizing resource allocation in stroke care settings. This study has valuable insights, but there are limitations to consider. The small sample size of 152 patients may not represent the broader population, and the study was conducted at a single center, limiting its generalizability. The exclusion of patients with posterior circulation strokes, as this study was based on the primarily developed ASPECTS that focus only on the anterior circulation, and limited diversity among participants may affect the applicability of the results. However, a pc-ASPECTS has been developed and used in various studies to predict functional outcomes21-26.
Furthermore, the study focused on limited variables and lacked long-term follow-up, hindering a comprehensive understanding of stroke outcomes and differences between left and right-sided strokes, patients’ handedness was not explored, hence dominance of the hemispheres was not studied. Factors like lifestyle habits, comorbidities, and treatments were not examined, potentially influencing the overall conclusions.
ASPECTS remains valuable for prognosis, but more research is needed to clarify hemisphere impact on prediction power. Larger samples, detailed neuroimaging, and long-term follow-up may reveal nuances in laterality. Prognosis seems more driven by ASPECTS score severity than hemisphere alone. Future work expanding on these limitations could enhance understanding to guide stroke management decisions.
We express our sincere gratitude to Dr. Ziauddin University and Hospital for granting us the opportunity to conduct our research in their esteemed Neurology ward and Stroke unit. Special thanks go to Dr. Bashir A. Soomro and Dr. Inayat Ali Khan for their invaluable assistance and support throughout the study. Their guidance and expertise have been instrumental in the successful completion of this research.
The authors declare no conflict of interest.
The study was initiated only after obtaining ethical approval from the Ethical Review Committee of Dr. Ziauddin University. (Reference Code: 5380522HANEU).
Patients or their next of kin who agreed to participate in the study provided written informed consent in both English and Urdu languages.
HA conceived the idea, conducted the relevant literature search, and obtained permission from the Ethical Review Committee of Dr. Ziauddin University. HA also took the lead in writing the manuscript. BS, and IAK contributed to the literature search and played crucial roles in finalizing the discussion of the article. Additionally, they provided invaluable clinical support to the patients involved in the study. The collaborative efforts of all authors have significantly contributed to the completion and success of this research.
- Gattringer T, Posekany A, Niederkorn K, Knoflach M, Poltrum B, Mutzenbach S, Haring HP, Ferrari J, Lang W, Willeit J, Kiechl S. Predicting early mortality of acute ischemic stroke: score-based approach. Stroke. 2019;50(2):349-356. https://doi.org/10.1161/STROKEAHA.118.022863
- Martínez-Coria H, Arrieta-Cruz I, Cruz ME, López-Valdés HE. Physiopathology of ischemic stroke and its modulation using memantine: evidence from preclinical stroke. Neural Regeneration Research. 2021;16(3):433. doi: 10.4103/1673-5374.293129
- Chugh C. Acute ischemic stroke: management approach. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2019;23(Suppl 2): S140.doi: 10.5005/jp-journals-10071-23192
- McClelland G, Rodgers H, Flynn D, Price CI. The frequency, characteristics and aetiology of stroke mimic presentations: a narrative review. European Journal of Emergency Medicine. 2019;26(1):2-8. DOI: https://doi.org/10.1097/MEJ.0000000000000550
- Ganesh A, Lindsay P, Fang J, Kapral MK, Côté R, Joiner I, Hakim AM, Hill MD. Integrated systems of stroke care and reduction in 30-day mortality: a retrospective analysis. Neurology. 2016;86(10):898-904. https://doi.org/10.1212/WNL.0000000000002443
- Khan MI, Khan JI, Ahmed SI, Haq U. The Epidemiology of Stroke in a Developing Country (Pakistan). J Neurol Stroke. 2018;8(1): 00275.DOI: https://doi.org/10.15406/jnsk.2018.08.00275
- Vagal A, Wintermark M, Nael K, Bivard A, Parsons M, Grossman AW, Khatri P. Automated CT perfusion imaging for acute ischemic stroke: pearls and pitfalls for real-world use. Neurology. 2019;93(20):888-898. https://doi.org/10.1212/WNL.0000000000008481
- Adan AM. A study of evaluation and proper diagnosis of stroke in CT scan and MRI. ACADEMIC JOURNAL. 2022. doi: 10.3306/AJHS.2022.37.06.130
- Anwar MM, Afrin S, Hossain MS, Jahan SM, Rahman MM. Sensitivity, Specificity, Predictive Values and Accuracy of Clinical Diagnosis of Acute Stroke. Journal of Rangpur Medical College. 2023;8(1):33-39. DOI: https://doi.org/10.3329/jrpmc.v8i1.65038
- Guarnizo A, Farah K, Lelli DA, Tse D, Zakhari N. Limited usefulness of routine head and neck CT angiogram in the imaging assessment of dizziness in the emergency department. The Neuroradiology Journal. 2021;34(4):335-340. https://doi.org/10.1177/1971400920988665
- Barber PA, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. The Lancet. 2000;355(9216):1670-1674.https://doi.org/10.1016/S0140-6736(00)02237-6
- de Freitas Brito, R., Bettero, P.A.G., Veiga, A.C.P. and Destro Filho, J.B., Alberta Stroke Program Early CT Score Region Segmentation. 2021 https://www.doi.org/10.33422/4th.msetconf.2021.03.05
- Ghodsi H, Mehrizi MA, Khoshdel AR, Shekarchi B. Evaluation of combining Alberta Stroke Program Early CT Score (ASPECTS) with mean platelet volume, plateletcrit, and platelet count in predicting short-and long-term prognosis of patients with acute ischemic stroke. Clinical Neurology and Neurosurgery. 2021; 208:106830. https://doi.org/10.1016/j.clineuro.2021.106830
- Esmael A, Elsherief M, Eltoukhy K. Predictive value of the alberta stroke program early CT score (ASPECTS) in the outcome of the acute ischemic stroke and its correlation with stroke subtypes, NIHSS, and cognitive impairment. Stroke research and treatment. 2021;2021. https://doi.org/10.1155/2021/5935170
- Mehrpour M, Motamed MR, Aghaei M, Jalali N, Ghoreishi Z. Unusual recovery of aphasia in a polyglot Iranian patient after ischemic stroke. Basic and clinical neuroscience. 2014;5(2):173
- J. H. Warwick Pexman, Philip A. Barber, Michael D. Hill, Robert J. Sevick, Andrew M. Demchuk, Mark E. Hudon, William Y. Hu and Alastair M. Buchan
- American Journal of Neuroradiology September 2001, 22 (8) 1534-1542;
- Erler KS, Wu R, DiCarlo JA, Petrilli MF, Gochyyev P, Hochberg LR, Kautz SA, Schwamm LH, Cramer SC, Finklestein SP, Lin DJ. Association of modified rankin scale with recovery phenotypes in patients with upper extremity weakness after stroke. Neurology. 2022;98(18):e1877-1885. https://doi.org/10.1212/WNL.0000000000200154
- Khan M, Baird GL, Goddeau Jr RP, Silver B, Henninger N. Alberta Stroke Program Early CT Score infarct location predicts outcome following M2 occlusion. Frontiers in neurology. 2017; 8:98. https://doi.org/10.3389/fneur.2017.00098
- Schröder J, Thomalla G. A critical review of Alberta Stroke Program Early CT Score for evaluation of acute stroke imaging. Frontiers in neurology. 2017; 7:245. https://doi.org/10.3389/fneur.2016.00245
- Ween JE, Alexander MP, D’Esposito M, Roberts M. Factors predictive of stroke outcome in a rehabilitation setting. Neurology. 1996;47(2):388-392. https://doi.org/10.1212/WNL.47.2.388
- Aszalós Z, Barsi P, Vitrai J, Nagy Z. Lateralization as a factor in the prognosis of middle cerebral artery territorial infarct. European neurology. 2002;48(3):141-145. https://doi.org/10.1159/000065515
- Lu WZ, Lin HA, Bai CH, Lin SF. Posterior circulation acute stroke prognosis early CT scores in predicting functional outcomes: a meta-analysis. PLoS One. 2021 ;16(2):e0246906. https://doi.org/10.1371/journal.pone.0246906
- Tei H, Uchiyama S, Usui T, Ohara K. Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome. Journal of neurology. 2010; 257:767-773. DOI 10.1007/s00415-009-5406-x
- Sang H, Li F, Yuan J, Liu S, Luo W, Wen C, Zhu Q, Chen W, Lin M, Qi L, Zhong Y. Values of baseline posterior circulation acute stroke prognosis early computed tomography score for treatment decision of acute basilar artery occlusion. Stroke. 2021;52(3):811-820. https://doi.org/10.1161/STROKEAHA.120.031371
- Khatibi K, Nour M, Tateshima S, Jahan R, Duckwiler G, Saver J, Szeder V. Posterior circulation thrombectomy—pc-ASPECT score applied to preintervention magnetic resonance imaging can accurately predict functional outcome. World Neurosurgery. 2019;129: e566-571. https://doi.org/10.1016/j.wneu.2019.05.217
- Caruso P, Ridolfi M, Lugnan C, Ajčević M, Furlanis G, Bellavita G, Mucelli RA, Zdjelar A, Ukmar M, Naccarato M, Stella AB. Multimodal CT pc-ASPECTS in infratentorial stroke: diagnostic and prognostic value. Neurological Sciences. 2021; 42:4231-4240. DOI:10.1007/s10072-021-05072-x
- Liang W, Kwan AT, Ye H, Mofatteh M, Feng M, Wellington J, Fu P, Wei W, Sun Y, Huang J, Luo J. Post-ASPECTS and Post-PC-ASPECTS Predict the Outcome of Anterior and Posterior Ischemic Stroke Following Thrombectomy. Risk Management and Healthcare Policy. 2023:2757-2769. https://doi.org/10.2147/RMHP.S436661
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
