By Arshad Ali Shah1, Syed Dilbahar Ali Shah1, Sawera Haider2, Beenish Imam3, Faisal Ahmed3, Saima Zahoor4
- Cardiology Department, Dow University of Health Sciences, Karachi, Pakistan
- Cardiac Surgery Department, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, Pakistan
- Cardiology Department, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, Pakistan
- Adult Cardiology Department, Dr. Ruth K. M. Pfau Civil Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-2/018
How to cite: Shah AA, Shah SDA, Haider S, Imam B, Ahmed F, Zahoor S. A Case Report on Reverse Tokotsubo Cardiomyopathy: Diagnosis and Path toward Treatment. Pak J Med Dent. 2024;13(2): 116-120. Doi: 10.36283/PJMD13-2/018
Reverse takotsubo cardiomyopathy (rTTC), also known as inverted takotsubo syndrome, is an acute cardiac syndrome that mimics myocardial infarction and accounts for a smaller proportion of cases compared to the classic takotsubo syndrome. While the exact prevalence is not well-established, studies suggest that the proportion of patients with the rTTC variant out of all Takotsubo Cardiomyopathy (TTC) according to different literature ranges from 1-23%. This variant of TTC is characterized by basal and/or mid-akinesis/hypokinesis associated with apical hyperkinesis that resolves spontaneously. We report a case of a 30-year-old male patient who presented with complaints of sudden crushing chest pain and shortness of breath. After conducting a thorough examination, the patient’s diagnostic workup confirmed reverse takotsubo cardiomyopathy, elucidating the underlying cardiac pathology.
Keywords: Takotsubo Cardiomyopathy, Hypokinesia, Hyperkinesis.
Takotsubo cardiomyopathy (TTC), commonly known as “broken heart syndrome,” is an acute cardiac syndrome that mimics myocardial infarction1. It is characterized by transient abnormalities in cardiac wall motion, typically involving the mid and apical segments of the left ventricle, while the basal walls exhibit hyperkinesis2. It is important to note that TTC predominantly affects postmenopausal women and is commonly triggered by emotional or physical stressors3. Within the spectrum of TTC, a distinct variant known as reverse Takotsubo cardiomyopathy (rTTC) emerges, characterized by the presence of basal akinesis or hypokinesis alongside apical hyperkinesis3. The reported incidence of TTC among troponin-positive patients suspected of acute coronary syndrome (ACS) hovers around 2%; however, the prevalence of the rTTC variant within all TTC cases varies significantly, ranging from 1% to 23%3. Our report explored this captivating syndrome, presenting a case study focusing on the reverse variant, to contribute to the understanding and managing TTC.
A male patient, aged 30, visited the Emergency department of Dr. Ruth K M Pfau Civil Hospital, Karachi. The patient worked as a cook, was married, and had no known underlying health conditions. He presented with a sudden onset of symptoms, including chest pain and shortness of breath that had been occurring for the past four hours. The chest pain originated substantially, had a crushing nature, and was of moderate to severe intensity. The pain radiated to the left shoulder and worsened with exertion. The patient also experienced associated symptoms of nausea and vomiting. There was no history of fever, joint pain, cyanosis, hemoptysis, or immobilization. The patient’s family history revealed the significant information that his father had passed away at the age of 60 due to coronary artery disease.
Upon arrival, the patient exhibited vital stability and was alert and oriented to time, place, and person. The patient’s condition was characterized by normal body temperature, a blood pressure (BP) reading of 110/80 mg, a heart rate of 110 beats per minute, and a pulse that was normal in volume with no radio radial or radio femoral delays. Additionally, the patient had a respiratory rate of 22 breaths per minute and an oxygen saturation level of 94% while breathing room air.
A young male of average height and build was found alert and lying on the bed during the physical examination. On general examination, the patient presented with a flushed face. Further examination of the chest revealed bilateral basal crepitations. Assessment of the precordium did not reveal any visible pulsations or scar marks. The apex beat was localized at the 5th intercostal space medial to the midclavicular line, without any parasternal heave or thrill. No murmurs were appreciated upon auscultation. The abdominal examination yielded unremarkable findings.
Baseline investigations were conducted, and the results indicated abnormal findings. The Troponin I level was elevated at 2.51 ng/L (reference range: 0-0.04 ng/mL). Other hematological parameters showed a hemoglobin level of 16.7 g/dL, a total leukocyte count (TLC) of 11,000/cmm3, and a platelet count of 296 k/μL. Renal function tests exhibited a blood urea nitrogen (BUN) level of 20 mg/dL and a serum creatinine level of 1.1 mg/dL. Electrolyte analysis demonstrated sodium (Na) at 136 mmol/L, potassium (K) at 4.2 mmol/L, and chloride (Cl) at 99 mmol/L. Liver function tests indicated an alanine aminotransferase (ALT) level of 32 U/L and an alkaline phosphatase (ALP) level of 134 U/L. The International Normalized Ratio (INR) was measured at 0.97.
Following the baseline investigations, additional diagnostic measures were undertaken to evaluate the patient’s cardiac function and structural integrity. The echocardiogram findings revealed significant motion wall abnormalities, indicating irregularities in the movement of the myocardium. The echocardiogram findings demonstrated that all basal and mid segments of the left ventricle (LV) were akinetic, indicating a lack of movement or contraction in these regions. Conversely, hyperkinetic motion was observed in the apical segments and LV apex, suggesting increased contractility and heightened activity in these areas.
Furthermore, the echocardiogram revealed a normal-sized LV, but with moderate to severe LV systolic dysfunction. This indicates impaired LV function during the contraction phase of the cardiac cycle. Notably, the ejection fraction (EF), a critical measure of cardiac performance, was estimated to be significantly low, ranging from 30% to 35%. (Figure 1)

Figure 1: a) Shows short axis view at the mitral valve level and displays hypokinetic basal segments during systole b) Shows short axis view at the apical level and displays hyperkinetic apical segments during systole
To further assess the patient’s LV function and detect any potential abnormalities, a left ventricular angiogram was also conducted. The angiogram revealed a hyperkinetic motion at the LV apex, indicating increased contraction in that particular region. In contrast, the base of the LV exhibited hypokinetic motion, suggesting reduced contraction or impaired function. Moreover, coronary angiography was performed during the same procedure to assess the patency and health of the coronary arteries. Remarkably, the coronary angiography results showed normal coronary arteries without any notable pathology, indicating that the patient’s coronary circulation was intact. (Figure 2)
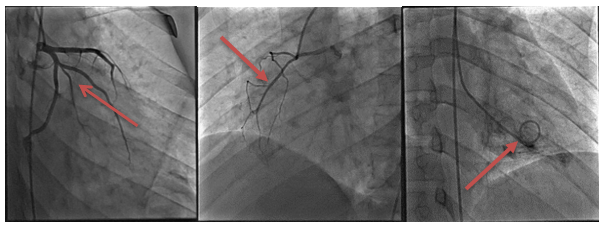
Figure 2: a) The Left system of the coronary artery was engaged via the femoral approach. It showed normal epicardial coronary arteries, b) non-dominant normal right epicardial coronary artery, and c) LV angiogram showing hyperkinetic LV apex and hypokinetic base of LV during systole.
Additionally, electrocardiography was conducted to assess for any significant pathologies, which unveiled the presence of sinus bradycardia along with hyperacute T waves observed in leads V3, V4, and V5. These findings served as notable observations, contributing to the comprehensive characterization of the cardiac manifestations associated with Takotsubo cardiomyopathy in this particular patient. (Figure 3)
Based on the LV angiogram findings of hyperkinetic LV apex and hypokinetic LV base, in conjunction with the echocardiogram revealing motion wall abnormalities, a diagnosis of reverse takotsubo cardiomyopathy is considered in this case. The patient was managed symptomatically, using analgesics to alleviate chest pain. Additionally, specific triggers associated with this condition, such as physical and emotional stress, were advised to be avoided.
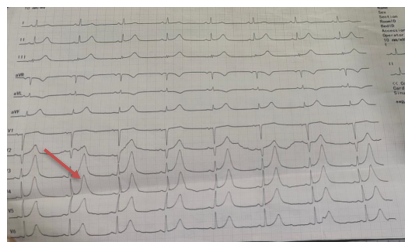
Figure 3: This ECG shows sinus bradycardia with hyperacute T waves in leads V3, V4 and V5.
Takotsubo cardiomyopathy (TC) or broken heart syndrome is a rare cause of stress cardiomyopathy. It was called Takotsubo after an octopus trap- in Japanese because of the typical ballooning appearance of the left ventricle of the heart. First reported in the 1990s, in Japan, it is a disease that occurs exclusively in women. Greater than 90% of the cases occurred in elderly women between ages 58 to 754.
We present a case of a male, resident of Karachi with no prior comorbidities. The main clinical symptoms of the disease manifest from chest pain and shortness of breath (SOB) resembling angina-like characteristics4. Our 30-year-old patient narrated that he was in his usual state of health when suddenly he developed chest pain, substernal in origin, crushing in nature, moderate to severe in intensity, with radiation to shoulders. It increased on exertion and was associated with SOB, nausea vomiting, and no association with respiration.
The disease comprises a short-term cardiac wall motion deformity of the left ventricle mostly due to an underlying stress that settles completely with time. Therefore, it is also called stress-induced cardiomyopathy or transient Left Ventricle (LV) apical ballooning syndrome5. Diagnostic criteria given by the Mayo Clinic include symptoms such as chest pain and ST elevation on ECG mimicking STEMI, transitory hypokinesia or akinesia of the apex of the left ventricle, and hyperkinesia of the basal region of the heart as seen on echocardiogram or ventriculogram. The organization of the coronary arteries remains unaffected at least in the first 24 hours after the event as established by angiogram5. Brain natriuretic peptide (BNP), a marker of ventricular function is high in such cases as well6. In addition, there are no signs of cranial bleeds, pheochromocytomas, or myocarditis5.
According to a case report based on four patients, published in 2017, it was found out that there was ST elevation in the anterior leads of three people while QT interval was prolonged in all cases and troponin levels were also not very high thus concluding that acute myocardial infarction can cause stress cardiomyopathy7. Our case presented with Troponin I levels of 2.5 ng/L and echocardiogram findings included akinetic basal and mid segments, hyperkinetic but normal-sized LV apex with an ejection fraction of 30-35%. The systolic function of the LV was typically decreased. The exact pathogenesis of the disease remains unknown but the postulated theories include coronary artery spasm, catecholamine excess8, microvascular dysfunction, and estrogen deficiency6.
Ramaraj et all presented interesting research that proposed 4 different subtypes of Tokotsubo cardiomyopathy namely classic, cavitary, and reverse or inverted. Patients with the reverse subtype of cardiomyopathy were of a comparatively younger age group (mean age: 36) than other types (mean age: 62)9. Our patient’s age falls in the classic subtype more than the reverse cardiomyopathy. The recurrence rate of TC is around 10%6. The majority of patients recover cardiac functions within 4-6 weeks. Research by Mehak Shah et all suggested that patients were mostly readmitted to the hospital for non-cardiac causes and not due to recurrence of TC10. LV thrombi, pericardial and pleural effusions, and myocarditis are the most common complications of this disease. Juan Manuel et all analyzed a 60-patient case series concluding that cardiogenic shock was excessive in male patients with Left bundle branch block with TC11. Management is predominantly supportive comprising of resolution of physical or emotional stress along with analgesics and specific care in cases which have worsened to cardiogenic shock or cardiac failure.
In summary, reverse takotsubo cardiomyopathy stands as a unique and infrequent cardiac syndrome, displaying transient left ventricular dysfunction with hyperkinesis of LV apex. Typically precipitated by acute emotional or physical stress, this intriguing condition requires further exploration to unravel its underlying mechanisms, optimize therapeutic approaches, and establish long-term prognostic implications. Enhanced understanding of reverse takotsubo cardiomyopathy promises to refine clinical management and improve patient outcomes.
The authors would like to acknowledge and extend their gratitude to the institution.
The authors declare no conflict of interest.
AAS, SDAS, and BI conducted physical examinations and relevant investigative procedures. SH collected and compiled the data, interpreted the results, and writeup FA, SZ history taking, and preliminary tests and writeup.
- Akel T, Barsoum E, Mroue J, Nalluri N, Tamburino F, Bogin M. Reverse Takotsubo Cardiomyopathy Following Exploratory Laparotomy. J Investig Med High Impact Case Rep. 2018; 6:2324709618757259. doi:10.1177/2324709618757259
- Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155(3):408-417. doi:10.1016/j.ahj.2007.11.008
- Awad HH, McNeal AR, Goyal H. Reverse Takotsubo cardiomyopathy: a comprehensive review. Ann Transl Med. 2018;6(23):460. doi:10.21037/atm.2018.11.08
- Takotsubo cardiomyopathy (broken-heart syndrome). Harvard Health. 2010.
- Komamura K, Fukui M, Iwasaku T, Hirotani S, Masuyama T. Takotsubo cardiomyopathy: Pathophysiology, diagnosis and treatment. World J Cardiol. 2014;6(7):602-609. doi:10.4330/wjc.v6.i7.602
- Parekh M. Change of heart: Reverse Takotsubo’s cardiomyopathy – A case report. Clin Imaging. 2021;69:219-222. doi:10.1016/j.clinimag.2020.08.018
- Christodoulidis G, Kundoor V, Kaluski E. Stress Induced Cardiomyopathy Triggered by Acute Myocardial Infarction: A Case Series Challenging the Mayo Clinic Definition. Am J Case Rep. 2017;18:931-936. doi:10.12659/AJCR.902860
- Bhat S, Gazi H, Mwansa V, Chhabra L. Catecholamine-induced reverse takotsubo cardiomyopathy. Proc Bayl Univ Med Cent. 2019;32(4):567-569. doi:10.1080/08998280.2019.1634229
- Ramaraj R, Movahed MR. Reverse or inverted takotsubo cardiomyopathy (reverse left ventricular apical ballooning syndrome) presents at a younger age compared with the mid or apical variant and is always associated with triggering stress. Congest Heart Fail Greenwich Conn. 2010;16(6):284-286. doi:10.1111/j.1751-7133.2010.00188.x
- Shah M, Ram P, Lo KBU, et al. Etiologies, predictors, and economic impact of readmission within 1 month among patients with takotsubo cardiomyopathy. Clin Cardiol. 2018;41(7):916-923. doi:10.1002/clc.22974
- Nogales-Asensio JM, González-Fernández MR, López-Mínguez JR, Merchán-Herrera A, Martínez-Cáceres G, Aranda-López C. Síndrome de Tako-tsubo: análisis de una serie de 60 casos. Med Clínica. 2014;143(6):255-260. doi:10.1016/j.medcli.2014.02.027
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
