By Arham Shah1, Yasir Murtaza2, Zahra Saifuddin3
- General Surgery Department, Ziauddin Hospital, Karachi, Pakistan
- Urology Department, Ziauddin Hospital, Karachi, Pakistan
- Surgery Department, Ziauddin Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/022
How to cite: Shah A, Murtaza Y, Saifuddin Z. Xantho-granulomatous Orchitis: A Rare Cause of Scrotal Swellings. Pak J Med Dent. 2024;13(1): 119-124. Doi: 10.36283/PJMD13-1/022
We aim to present an adult case of a rare cause of scrotal swelling i.e., xantho-granulomatous orchitis (XGO). The patient presented to us with a history of swelling and pain in the left scrotum for one month. There were no other associating symptoms and sexual and traumatic history were not present. Incision and drainage were planned for the patient under our care, however, because of ruptured tunica albuginea and dispersion of seminiferous tubules, left orchiectomy was performed and the specimen was sent for histopathological analysis. Xantho-granulomatous inflammation (XGI) is a relatively benign and infrequent condition and usually affects the 3rd-7th decade of life. The lipid-laden macrophages replace the destructed and necrotic normal tissue. The findings that are the hallmark of granulomatous diseases are necrosis and multinucleated giant cells which are not present in cases of XGI. It affects the testis, epididymis, spermatic cord, and bladder among genital organs.
Keywords: Genitalia, Orchitis, Scrotum, Swelling, Xanthogranulomatous.
Xantho-granulomatous inflammation (XGI) is a benign inflammatory condition commonly and the kidney and gallbladder are the most common organs to be affected. The much rarer organs to be affected are the bones, urinary bladder, liver, appendix, ovaries, and vagina 1. The distinguishing characteristics of XGI are that the cellular infiltrate of foamy histiocytes containing an admixture of plasma cells, multinucleated giant cells, and foci of necrosis are responsible for the destruction of tissue 2. Testicular involvement is relatively rare and according to our best knowledge, few cases of this condition have been reported in the literature. We report a case of Xantho-granulomatous orchitis (XGO) in a young adult. Histopathological biopsy report revealed exudative regions along with testicular ischemic necrosis all mixed with inflammation.
A 22-year-old male, having no co-morbidity, presented at the outpatient department with complaints of pain and swelling in the left scrotum for one month. The patient revealed no history of urethral discharge, fever, or any constitutional symptoms relating to urinary infection. The patient also gave no history of trauma or sexual contact. Examination revealed left scrotal swelling, and reddening of the skin and it was severe tenderness Testicular torsion was ruled out during examination.
The patient was advised scrotal ultrasonography and urine culture and was started on empirical treatment with Amoxicillin/Clavulanic acid for 5 days and further advised to follow up with reports after completing a 5-day course of antibiotics. However, the patient followed up after 10 days with no improvement in symptoms. Upon inquiring, the patient revealed that he took antibiotics for 2 days only, instead of 5 days. The examination findings were the same as in the previous visit.
Ultrasonography of the scrotum revealed the left epididymis to be bulky showing low echogenicity with hyperemia on color Doppler application with reactionary thick wall spermatic cord and subcutaneous edema, suggestive of inflammatory/infective etiology.
The urine culture report showed no growth within the specimen. The patient was advised to take the same antibiotic along with painkillers for 5 days and follow up after completing the course.
But 3 days after the last visit, the patient presented to the emergency department with the worsening of symptoms. On this visit, there were some changes in the examination findings. Examination revealed left scrotal swelling, firm but cystic in some areas, hyperemic, with 2 small dark brown patches and a dry peeling thin layer of epidermis with yellowish purulent fluid beneath it and extremely tender to touch (Figure 1).

Figure 1: Examination revealed left scrotal swelling, firm but cystic in some areas, hyperemic, having a yellow gangrenous patch at the inferior aspect and a dry thin layer of skin, breached through some points with purulent discharge and extremely tender to touch.

Figure 2. Black arrow showing normal testicular tissue. The blue arrow represents dispersed seminiferous tubules bulging out through ruptured tunica albuginea of the left testis.
His scrotal ultrasonography was repeated which had the same findings as in the previous report.
Hospital admission was advised. The patient was started on intravenous Ceftriaxone and painkillers. Incision and drainage of the left hemiscrotum were planned as per clinical and radiological findings as it was being treated as a testicular abscess. The incision was given to the left hemiscrotum, which revealed ruptured tunica albuginea and dispersion of seminiferous tubules, mixed with purulent discharge (Figure 2). In light of the findings, the surgery of choice was left orchiectomy with a margin to the cord. The specimen was sent for histopathological analysis.
Histopathological biopsy report revealed exudative regions along with testicular ischemic necrosis all mixed with inflammation. Sheets of histocytes and multiple giant cells are seen forming granulation tissue, suggestive of xantho-granulomatous inflammation. Special stains used for mycobacterial and fungal microorganisms came out to be negative. No evidence of malignancy. The immunohistochemical analysis was done which showed CD68: positive in histocytes. (Figures 3 and 4).
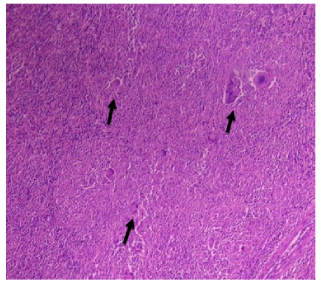
Figure 3. Histological slide of testicular parenchyma showing multinucleated giant cells along with diffuse sheets of histiocytes. Black arrows represent multinucleated giant cells.
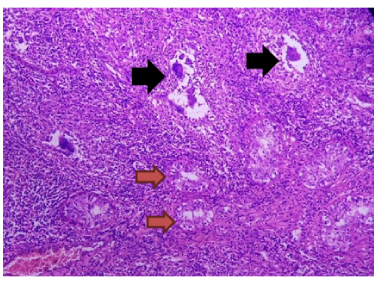
Figure 4. Histological slide of testicular parenchyma showing widely spaced tubules separated by diffuse sheets of histiocytes along with intimately admixed multinucleated giant cells. Yellow arrows represent testicular parenchyma. Black arrows represent multinucleated giant cells.
Xantho-granulomatous inflammation is a benign condition that is relatively rare with an unclear etiology 3. It was first described in 1926 by Grunberg 4. It is non neoplastic inflammatory disease that presents as a mass lesion and therefore mimics malignancy 5. Common organs that are affected are kidneys, liver, and gall bladder, and less common organs that are affected are the cecum, ovaries, and bladder 3. XGI involves urogenital organs and often affects the kidney, bladder epididymis, testis, spermatic cord, and prostate. The testicle is much more affected than the epididymis, but solo cases of XGI in the spermatic cord have not yet been reported. XGO is not specific to any age group and can occur in young adults and the elderly. Most cases of XGO have had unilateral presentation, however, there have been cases where bilateral XGOs have been reported. It is not known why the right testicle is much more affected than the left 4. The exact pathogenesis of this condition has not been determined; however, many authors have hypothesized multiple factors leading to XGO. One of the reasons could be because of the remains of surgical thread, calculi as a foreign body, lymphatic dysfunction, and alteration in the immune system which affect the metabolism of macrophages and lipids 6. Testicular abscess is a rare complication of epididymo-orchitis and XGO is a rare subgroup of testicular abscess4. XGI formation is affected by bacterial infection, impaired response host, and reduced leukocyte function 2.
Diabetes mellitus is a frequent association with XGI, thus opening the door for another possible mechanism and pathogenesis that has not yet been explored. Diabetes mellitus was found in one-third of the reported cases and was also reported by I Ademi 4. The risk of infection increases in a diabetic patient as diabetes predisposes to immunocompetence, and therefore all routine activities of leukocytes are compromised, these include bactericidal activity, phagocytosis, adherence, chemotaxis, and bactericidal activity 4. A case of a tetraplegic patient was reported in which the cause of XGO was urinary reflux along the ductus deferens 7. Among other risk factors include urinary reflux in the ductus deferens, chronic inflammation secondary to infections, surgery, and/or catheterization causing changes to the urethra 2. Our case was not related to any of these risk factors.
Epididymal obstruction or urinary obstruction is one of the most common factors associated with this case. XGO has also been reported because of atherosclerosis leading to testicular ischemia in the patients of older age group, and in younger patients, it can be caused by endarteritis or endophlebitis. The patient in our care had no history of obstructive uropathy or testicular torsion. Urinary tract infection is also one of the etiological factors leading to XGO9, one of them being infectious microorganisms, however, culture reports usually reveal no growth of microorganisms. The most common organism associated with XGO is Escherichia coli2.
Mostly the use of antibiotics and chronic inflammation are the two causes that suggest the failure to identify any microorganisms In most cases, failure to associate any infectious agent may be due to chronic inflammation and routine antibiotic use before therapy 2. The culture report in this case was unremarkable. This sheds light on the fact that obstruction or failure of antegrade sperm flow along with reflux of infected urine into the reproductive system leads to local infection rather hematogenous spread of infection that initiates an immune response10. A local tumor may illicit a response to 1. The occurrence has also been reported after testicular trauma 11. There was no history of testicular trauma, or associated tumor in the current case.
Diagnosis of XGO preoperatively is quite challenging because it mimics testicular neoplasms regarding clinical and radiological features. Painless testicular swellings are the most common presentation and on radiological investigations such as testicular and groin ultrasound they appear as mass lesions 10. Fine needle aspiration cytology also does not give a definitive diagnosis. Serum tumor biomarkers can be used as a tool for preoperative diagnosis because they may be elevated in cases of XGO 5. Although serum tumor markers are within the normal range in some cases of testicular tumors, it is challenging to distinguish between the two conditions. Taking these factors into account, diagnosis depends on histopathological examination of the resected specimen 5.
These lesions can be termed pseudo-neoplastic and can be divided into those that mimic macroscopically and those that mimic neoplasia microscopically, regardless of whether they form a macroscopic mass. It is much more difficult for the pathologist to classify lesions, especially those that microscopically mimic neoplasia4. Histologically, granulomatous orchitis occurs because of trauma, infections, autoimmune diseases, or sperm extravasation. Other infectious agents include tuberculosis, syphilis, leprosy, and brucellosis. Distinct granulomas do not occur in cases where the cause remains unknown 10.
Microscopically, XGO is identified by its typical finding of aggregated foamy histiocytes mixed with inflammatory cells destroying the testicular parenchyma. Malakoplakia, Rosai-Dorfman disease, and infectious epididymorchitis are differential diagnoses based on histopathological findings.1,8. Intracytoplasmic laminated concretions of calcium and iron known as Michaelis Gutmann bodies, were not identified, therefore malakoplakia was excluded. As large histiocytes with pathognomonic lymph phagocytosis known as emperipolesis were absent, and together with negative staining of histiocytes on S100 immunostaining, Rosai-Dorfmann disease was excluded as a differential diagnosis. No mold was seen on the PASD special stain, and the Ziehl Neelson special stain was negative for acid-fast bacilli,excluding the diagnosis of tuberculosis2, 8.
Diagnosis is challenging because the condition on physical examination resembles bacterial orchitis, which usually improves with antibiotic therapy, but in this case, antibiotic therapy showed no improvement.
XGI is characterized by severe tissue destruction, and therefore surgical removal is the only curative treatment in most cases6. Orchiectomy is therefore the procedure of choice in XGO7. The role of antibiotics is a disputed treatment modality, as the tissue affected is lost in many cases. Unless the scrotum/scrotal wall is involved, the method of choice should be trans-inguinal orchiectomy. In conditions of XGI when testicular abscess or scrotal sinuses are present (as in this case), then scrotal orchiectomy combined with hemicolectomy is preferred9.
Xantho-granulomatous orchitis is a benign, non-neoplastic inflammatory condition, which is quite rare as only a few cases have been reported. There is no specific laboratory test or radiological investigation that could diagnose the disease. Currently, it can only be diagnosed on histopathology analysis. The only curative treatment for this condition is orchiectomy. Further research work should be done to know the exact etiology and establish a proper treatment regime.
None.
The authors declare no conflict of interest.
Patient consent was taken.
All authors contributed equally to this case report write-up.
(1) Alazab RS, Ghawanmeh HM, Al-Okour RK, Alshammari A, Lafi T, Al-Karasneh AI, Al-Bashir S, Al-Ghazo M. Xanthogranulomatous orchitis: rare case with brief literature review. Urology Case Reports. 2017;13:92-93. DOI: https://doi.org/10.1016/j.eucr.2016.12.006
(2) Rifat Mannan AA, Kahvic M, Abu Sara Y, Bharati C. An unusual case of extensive xanthogranulomatous orchitis in a diabetic patient. Medical Principles and Practice. 2009;18(5):418-421. DOI: https://doi.org/10.1159/000226299
(3) Chlif M, Chakroun M, Rhouma SB, Chehida MA, Sellami A, Gargouri MM, Nouira Y. Xanthogranulomatous pyelonephritis presenting as a pseudotumour. Canadian Urological Association Journal. 2016;10(1-2):E36. DOI: 10.5489/cuaj.3225
(4) Ademi I, Vrajnko A, Ademi M. Xanthogranulomatous Epididymo-Orchitis As A Uncommon And Rare Pseudoneoplastic Condition. Knowledge-International Journal. 2020;38(4):657-662.
(5) Murshed KA, Taha NM, Ben-Gashir M. A case of xanthogranulomatous orchitis and its preoperative diagnostic challenges. Urology Case Reports. 2020; 32:101248. DOI: https://doi.org/10.1016/j.eucr.2020.101248
(6) Demirci D, EKMEKÇİOǦLU O, Soyuer I, EMİRDOǦAN M. Xanthogranulomatous orchitis with scrotal fistulas. International journal of urology. 2004;11(8):686-688. DOI: https://doi.org/10.1111/j.1442-2042.2004.00864.
(7) Val‐Bernal JF, González‐Márquez P, Ramos‐Barseló E, Portillo JA. Concurrent xanthogranulomatous orchiepididymitis and seminoma in the same testis. Pathology international. 2010;60(1): 55-58.DOI: https://doi.org/10.1111/j.1440-1827.2009.02475.x
(8) Nistal M, Gonzalez-Peramato P, Serrano A, Regadera J. Xanthogranulomatous funiculitis and orchiepididymitis: report of 2 cases with immunohistochemical study and literature review. Archives of pathology & laboratory medicine. 2004;128(8):911-914. DOI: https://doi.org/10.5858/2004-128-911-XFAORO
(9) Ezer SS, Oguzkurt P, Temiz A, Bal N, Hicsonmez A. Xanthogranulomatous orchiepididymitis: a very uncommon cause of scrotal mass in childhood. Urology. 2013;82(1):228-230. DOI: https://doi.org/10.1016/j.urology.2013.01.039
(10) amin Said SH, Abdalla RY, Aghaways I, Abdullah AM. Xanthogranulomatous orchitis: review of the published work, and report of one case. Urology Case Reports. 2019; 27:100908. DOI: https://doi.org/10.1016/j.eucr.2019.100908
(11) Yamashita S, Umemoto H, Kohjimoto Y, Hara I. Xanthogranulomatous orchitis after blunt testicular trauma mimicking a testicular tumor: A case report and comparison with published cases. Urology journal. 2017;14(3).
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
