By Fariha Khan1, Umar Murad Khan2, Ali Murad Khan3, Usman Mir Khan4
1. Pakistan Kidney and Liver Institute, Lahore, Pakistan
2. Faculty of Veterinary Medicine, Selcuk University, Konya, Türkiye
3. Faculty of Bio-Sciences, University of Veterinary and Animal Sciences, Lahore, Pakistan
4. National Institute of Food Science and Technology, University of Agriculture, Faisalabad, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/004
How to cite: Khan F, Khan UM, Khan AM, Khan UM. Trend of Non-Alcoholic Fatty Liver Disease in Type II Diabetes Mellitus. Pak J Med Dent. 2024;13(1): 11-16. Doi: 10.36283/PJMD13-1/004
Background: Non-alcoholic fatty liver disease (NAFLD) is becoming quite common in Type II Diabetes Mellitus (TIIDM) as obesity and insulin resistance are common within TIIDM and it is becoming a widespread liver condition globally. This study evaluated the prevalence of NAFLD patients who also had type II diabetes.
Methods: The demographic data (name, age, body mass index (BMI), gender, occupation, duration of TIIDM, and treatment taking for TIIDM), as well as the results of the tests for these enzymes, were also recorded. Alanine transaminase (ALT) and Aspartate transaminase (AST) levels, as well as abdominal ultrasound findings of the liver, were recorded in a proforma after informed consent for a total of 200 Type II diabetic patients. Using SPSS, the data were analyzed, and stratified groups were subjected to the Chi-square tests.
Results: There was a significant difference (p<0.05) observed in NAFLD patients of TIIDM concerning age, gender, BMI, treatment, occupation, and duration of diabetes. The sample size consisted of 200 patients of which 111 (55.5%) were men and 89 (44.5%) were women. Patients ranged in the age range of 40-70 years old, with a mean age of 55.08 ± 8.98 years and a mean BMI of 29.69±4.04, respectively. It was concluded that 64% of cases with diabetes mellitus had NAFLD.
Conclusion: TIIDM is an independent risk factor for NAFLD so early screening, diagnosis, and appropriate treatment are mandatory to reduce the risk of NAFLD and its related complications.
Keywords: Type II diabetes, Liver disease, NAFLD, Complications, Mortality.
Non-Alcoholic Fatty Liver Disease (NAFLD) is quite common in Type II Diabetes mellitus (TIIDM) as obesity and insulin resistance are major causes of TIIDM1. The hepatic component of metabolic syndrome is thought of as NAFLD. With a median frequency of roughly 20% in the general population and 42%-70% in those with TIIDM, it is becoming a widespread liver condition globally2. NAFLD is defined as hepatic steatosis with no secondary cause in steatosis and either proton density or fat fraction of more than ≥5.6% determined with quantitative fat/water selective proton magnetic resonance spectroscopy (MRS) or magnetic resonance imaging (MRI), or with histology and macrovesicular steatosis imaging with ≥5% of hepatocytes3. Simple steatosis and non-alcoholic steatohepatitis that cause cirrhosis and such consequences make up NAFLD4.
Clinical, laboratory, and imaging investigations are used to identify non-alcoholic fatty liver disease. MRS is now the most trustworthy imaging method for hepatic fat steatosis5. The American Diabetes Association (ADA) recommended performing an ultrasonography (US) examination on patients with type II pre-diabetes or diabetes who showed increased NAFL or alanine aminotransferase (ALT) to check liver fibrosis and NASH. The ADA recommendations advise employing noninvasive biomarkers and vibration-controlled transient elastography (VCTE) in risk classification6. Insulin resistance is closely associated with the condition. The primary causes of hepatic insulin resistance in NAFLD are thought to be hepatic inflammation and fat buildup7. NAFLD is regarded as a separate risk factor in TIIDM, severe liver disease, and cardiovascular disease. It is crucial to spot early metabolic changes to stop these diseases and their progression8.
In a Pakistani study, patients with TIIDM reported a 51% frequency of hepatobiliary dysfunction9. NAFLD was reported with 60.8% occurrence with the time in diabetic individuals in a study and 55% of the time in TIIDM from Saudi Arabia10.
Foremost, we can initiate early proper management and prevent the patients from hazardous consequences of liver dysfunction or hepatic failure. It has been noticed that among patients of TIIDM, the frequency of NAFLD varies in different populations. Moreover, the variability was also observed in local studies. This study was conducted to estimate the prevalence of NAFLD in TIIDM patients in the local population.
A cross-sectional study was done at Medical Unit 2 of Sir Ganga Ram Hospital in Lahore from January 29 to July 29, 2020, and ethical approval was obtained from the institution review board with reference number CPSP/REU/MED-2017-059-13448. A 200-sample size of patients was estimated with confidence level (95%), margin of error (5%), and predicted percentage of NAFLD such as ≥51% in siblings of TIIDM patients using consecutive sampling technique and non-probability methods11. Patients in the age range of 40-70 were chosen who met the inclusion criteria and had type II diabetes (HbA1c>6.5% and/or on treatment for diabetes or symptoms of hyperglycemia and random blood sugar level (BSL)>200mg/dL for more than 1 year). Patients with positive HBsAg, positive Anti-HCV antibodies, chronic liver disease before diabetes, or taking medicine for hepatic dysfunction including interferon therapy (on medical record), and those leading to hepatic dysfunction were omitted from the study.
After receiving informed consent, demographic information (name, occupation, gender, BMI, age, number of years with TIIDM, and medications used to treat it) was recorded. A 5cc disposable syringe was then used to draw blood, which was then forwarded to the hospital laboratory for AST and ALT testing. With the help of a researcher, a consultant radiologist with four years of residency experience performed ultrasonography on patients to assess fatty liver. NAFLD was labeled on the evidence of excessive fat on the liver on abdominal ultrasound with or without AST and ALT >40IU in the absence of alcohol intake. Patients with NAFLD were managed as per hospital protocol. All this information was recorded in a pre-designed performa12. The Statistical software (SPSS 20) was used to analyze the current data. The age, BMI, and length of patient TIIDM were quantitative factors that were provided as mean and standard deviation. Gender, occupation, and the frequency and proportion of TIIDM and hepatobiliary dysfunction therapy use were qualitative variables. The TIIDM was calculated using a two-stage, stratified, random sampling technique. The chi-square test was used as post-stratification to compare NAFLD in stratified groups, with significance consideration at p-value<0.05.
The sample size consisted of 200 patients of which 111 (55.5%) were men and 89 (44.5%) were women. The mean age mentioned here was calculated with the mean of the age groups from 40 to 70 years and BMI was the mean of the age group between 40 to 70 years with their respective NAFLD presences. Thus, patients ranged in the age range of 40-70 years old, with a mean age of 58.8 ± 8.9 years and a mean BMI of 29.69±4.04, respectively. A significant difference was observed within each group concerning NAFLD (absent/present) (p<0.05). Thus, results showed that the age group of 40-54 years showed NAFLD presence (58.8±8.9), and thus the remaining NAFLD absent accounted for 41.2±0.12 population in the same age group while the age group of 55-70 years showed NAFLD presence of 8.9±5.45 and absent in 31.1± 0.14 population and same results for all groups are shown in Table 1.
Table 1: Basic characteristics of study groups depending on NAFLD.
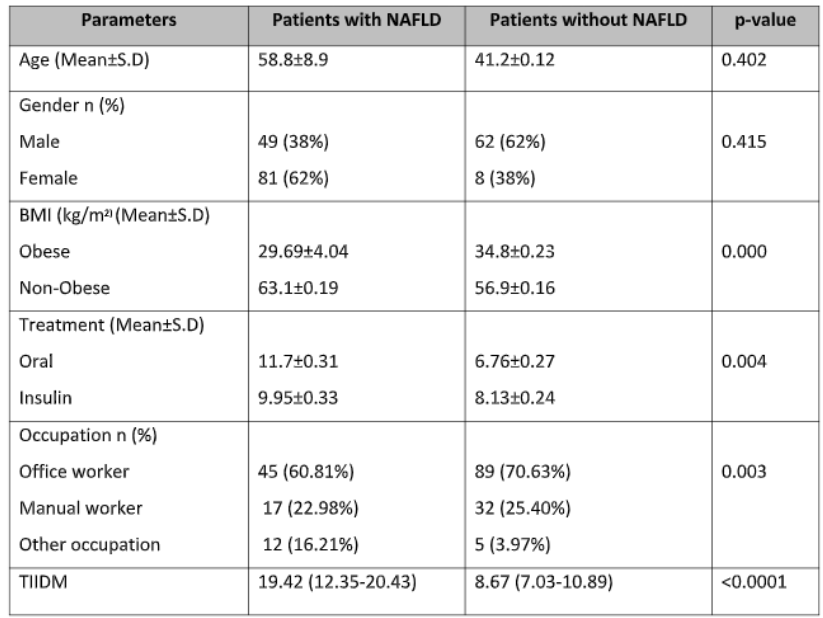
Descriptive statistics implemented on different parameters; BMI= body mass index; TIIDM= Type II diabetes mellitus, p-value <0.05 is considered significant.
These cases had a mean duration of TIIDM ranging from 8.67 to 19.42 in most prevalence situations. There were 62(31.0%) working men and women, 72(36.0%) were Govt. Employed, 49 (24.5%) were doing their own business and 17(8.5%) cases had other work occupations. In 107 instances (53.5%), insulin therapy was used, while oral medication was used in 93 cases (46.5%). A total of 128(64%) cases had non-alcoholic fatty liver disease.
The mean patient age in the current study was 55.08±8.98 years. There were 89 (44.5% of the cases) females and 111 (55.5%) males. In the TIIDM study, 130 instances comprised 81 (62%) females and 49 (38%) males. The patients were 52.31±5.96 years old on average. In the present study, there are differences in the distribution of gender and age. Out of 130 type II diabetes patients, results showed that 78 (60%) had fatty livers. NAFLD was evaluated according to its presence or absence within different age groups. The table shows the age at which NAFLD would be present or absent with the passage of age (Table 2).
Table 2: Comparison of NAFLD within age groups concerning gender, BMI, treatment, occupation, and duration of TIIDM
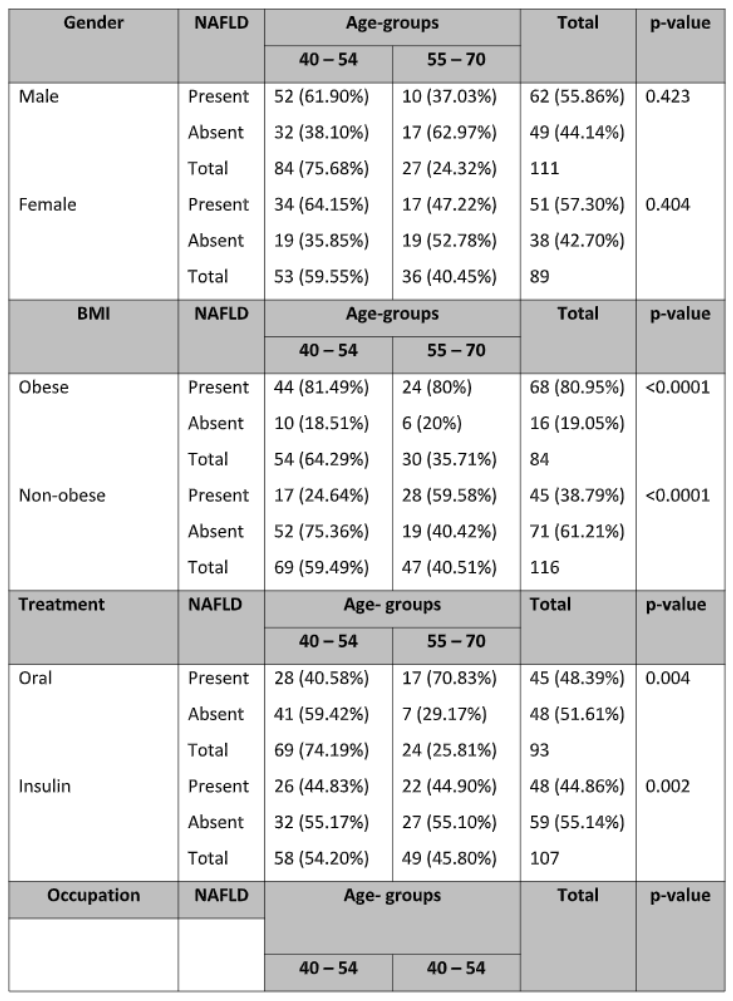
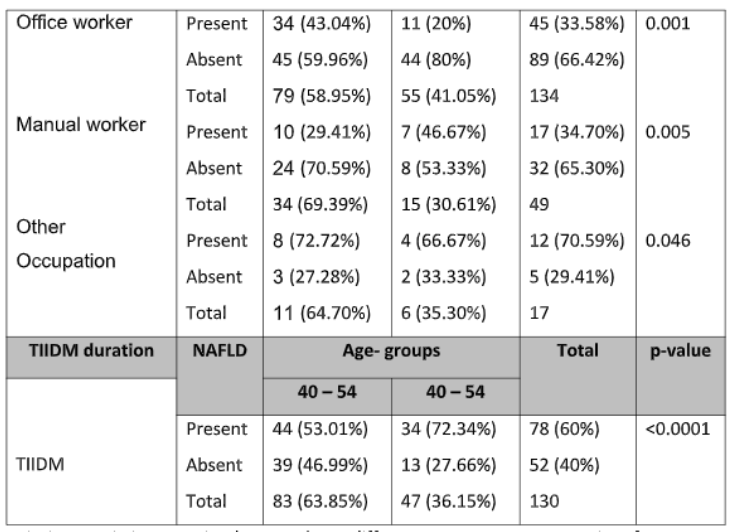
Descriptive statistics was implemented on different parameters concerning frequency and percentage [n (%)]. BMI= body mass index; TIIDM= Type II diabetes mellitus
The most prevalent NAFLD and liver illnesses are becoming global public health concern13. The NAFLD (steatosis hepatic and NAFL) and steatohepatitis (NASH), which are both characterized by fibrosis, hepatocyte lobular inflammation, and ballooning may proceed with cirrhosis and, in rare cases, hepatocellular carcinoma14.
Diabetes and NAFLD development are both correlated risk factors for obesity and physical inactivity. According to several studies, the prevalence of NAFLD in people with TIIDM ranges roughly between 34 and 94%15. If a person has NAFLD, their chance of acquiring diabetes is about five times higher. The insulin resistance, hepatic triglyceride (TG) dyslipidemia factors buildup in NAFLD and a faulty B-cell in TIIDM may all contribute to the link between NAFLD and type II diabetes16. Patients with TIIDM showed a higher chance of advanced liver disease development, such as hepatocellular carcinoma, fibrosis, and cirrhosis as compared to healthy people17. The role of diabetologists is crucial in identifying type II diabetes patients with higher NAFLD complications. But, thanks to recent advancements in the diagnosis of NAFLD and various phase III trials for NASH-specific therapies, an evolved caring plan is initiated for integrated multidisciplinary controls in such matters18.
The NAFLD prevalence in type II diabetes patients and its relationship to the resistance of insulin were assessed in 2017, and it was found that 45% of patients with NAFLD showed higher rates leading to central obesity (as determined by waist-hip ratio, BMI, and waist circumference), higher triglyceride and HbA1c levels19. As a result, among TIIDM patients, insulin resistance and the occurrence of NAFLD appear to be associated20. Higher NAFLD statistics were discovered in the current investigation, however, BMI had no significant effect.
This study compromised the results in agreement with a cross-sectional study that evaluated NAFLD prevalence and identified predictive factors related to NAFLD among South Asian Pakistani patients with Metabolic Syndrome (MS) and type II DM. The prevalence of NAFLD overall was 72.4%, and it was greater in patients with dyslipidemia, obesity, and HTN21. While higher values were observed among males than females. In this group, people with type II diabetes and metabolic syndrome, NAFLD prevalence was higher. Additionally, it was discovered that the growing MS components were linked with larger NAFLD risks, in addition to the fact that NAFLD was highly connected with MS22.
Similar to one previous study, this study established NAFLD prevalence and pinpointed risk factors in type II DM patients with NAFLD. In NAFLD individuals with Type II DM, obesity and high liver enzymes, triglycerides, and cholesterol are considerably elevated. It emphasizes the significance of routine lipid profiles and liver function testing in individuals with type II diabetes, who must be closely monitored for liver consequences and NAFLD23.
Another local study was utilized to ascertain NAFLD prevalence in type II diabetes patients present at Jinnah Postgraduate Medical Centre, Karachi, Pakistan. The study had 120 participants with type II diabetes in total. They were split into two groups, one with fatty livers and the other without, and further assessed using measurements of liver function tests, body mass index, lipid profile, and HbA1c. On ultrasonography, 73 (60.8%) of the 120 patients had fatty liver24. While, in comparison with non-fatty liver groups, the fatty liver group showed higher levels of HBA1c, BMI, AST, GGT, alkaline phosphatase, LDL, ALT, triglycerides, total cholesterol, and decline of HDL levels25.
Although this study showed a higher NAFLD prevalence in type II DM patients, lack of early screening, available resources for non-invasive investigations, and the cost of diagnostic scanning are the main limitations for proper diagnosis and management of these patients. Therefore, the author would recommend carrying out a multicenter study with a large sample size for more accurate results.
NAFLD was present in 64% of cases with type II diabetes mellitus. Early detection, diagnosis, and treatment are essential to lower the risk of NAFLD and the consequences linked to it. Mortality and morbidity among type II diabetic individuals can be greatly decreased by lowering NAFLD. Future research advancements in the diagnosis of NAFLD and various phase III trials for NASH-specific therapies will evolve the caring plan with initiation for integrated multidisciplinary controls in diabetes mellitus.
The authors are thankful to Medical Unit II, Department of Medicine, Sir Ganga Ram Hospital, Lahore for supporting this research and their valuable contribution.
Ethical Approval was obtained from the institution review board with reference number CPSP/REU/MED-2017-059-13448.
Ethical Approval was obtained from the institution review board with reference number CPSP/REU/MED-2017-059-13448.
Informed consent was taken from the patients for the collection of data and publication of results.
Each other has contributed to the manuscript equally and approved for submission of the manuscript.
[1] Bhatt HB, Smith RJ. Fatty liver disease in diabetes mellitus. Hepatobiliary surgery and nutrition. 2015 Apr;4(2):101. http:// https://doi.org/10.3978%2Fj.issn.2304-3881.2015.01.03
[2] Ahmed MH, Husain NE, Almobarak AO. Nonalcoholic Fatty liver disease and risk of diabetes and cardiovascular disease: what is important for primary care physicians? Journal of family medicine and primary care. 2015;4(1):45. http://doi.org/10.7759/cureus.3626
[3] Huang DQ, El-Serag HB, Loomba R. Global epidemiology of NAFLD-related HCC: trends, predictions, risk factors, and prevention. Nature Reviews Gastroenterology & Hepatology. 2021;18(4):223-238. https://doi.org/10.1038/s41575-020-00381-6
[4] Mandal A, Bhattarai B, Kafle P, Khalid M, Jonnadula SK, Lamicchane J, Kanth R, Gayam V, Jonnadula S. Elevated liver enzymes in patients with type 2 diabetes mellitus and non-alcoholic fatty liver disease. Cureus. 2018;10(11). https://doi.org/10.4103%2F2249-4863.152252
[5] Mehta SR, Thomas EL, Bell JD, Johnston DG, Taylor-Robinson SD. Non-invasive means of measuring hepatic fat content. World journal of gastroenterology: WJG. 2008;14(22):3476. https://doi.org/10.3748%2Fwjg.14.3476
[6] Care D. Standards of medical care in diabetes 2019. Diabetes Care. 2019;42(Suppl 1):S124-38. https://doi.org/10.2337/dc19-S008
[7] Gruben N, Shiri-Sverdlov R, Koonen DP, Hofker MH. Nonalcoholic fatty liver disease: a main driver of insulin resistance or a dangerous liaison? Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2014 Nov 1;1842(11):2329-2343. https://doi.org/10.1016/j.bbadis.2014.08.004
[8] Saponaro C, Gaggini M, Gastaldelli A. Nonalcoholic fatty liver disease and type 2 diabetes: common pathophysiologic mechanisms. Current diabetes reports. 2015;15:1-3. https://doi.org/10.1007/s11892-015-0607-4
[9] Ijaz-ul-Haque Taseer LH, Safdar S, Mirbahar AM, Ahmad I. Frequency of nonalcoholic fatty liver disease (NAFLD) and its biochemical derangements in Type-2 diabetic patients. Pakistan Journal of Medical Sciences. 2009;25(5):817-820. DOI: 20103029404
[10] Luxmi S, Sattar RA, Ara J. Association of non-alcoholic fatty liver with type 2 diabetes mellitus. Jlumhs. 2008;9:188-193. DOI: ID: emr-197938.
[11] Manoria P, Inamdar S, Kumar R. Hepatobiliary dysfunction in Type-2 diabetes mellitus. Journal of Family Medicine and Primary Care. 2017;6(3):563. https://doi.org/10.4103%2F2249-4863.222018
[12] Cho EE, Ang CZ, Quek J, Fu CE, Lim LK, Heng ZE, Tan DJ, Lim WH, Yong JN, Zeng R, Chee D. Global prevalence of non-alcoholic fatty liver disease in type 2 diabetes mellitus: an updated systematic review and meta-analysis. Gut. 2023 Nov 1;72(11):2138-2148. http://dx.doi.org/10.1136/gutjnl-2023-330110
[13] Feldstein AE, Canbay A, Angulo P, Taniai M, Burgart LJ, Lindor KD, Gores GJ. Hepatocyte apoptosis and fas expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125(2):437-443. https://doi.org/10.1016/S0016-5085(03)00907-7
[14] Firneisz G. Non-alcoholic fatty liver disease and type 2 diabetes mellitus: the liver disease of our age? World journal of gastroenterology: WJG. 2014;20(27):9072. https://doi.org/10.3748%2Fwjg.v20.i27.9072
[15] Angulo P. Nonalcoholic fatty liver disease. New England Journal of Medicine. 2002;346(16):1221-1231. DOI: 10.1056/NEJMra011775
[16] Hazlehurst JM, Woods C, Marjot T, Cobbold JF, Tomlinson JW. Non-alcoholic fatty liver disease and diabetes. Metabolism. 2016;65(8):1096-1108. https://doi.org/10.1016/j.metabol.2016.01.001
[17] Bondini S, Kleiner DE, Goodman ZD, Gramlich T, Younossi ZM. Pathologic assessment of non-alcoholic fatty liver disease. Clinics in liver disease. 2007;11(1):17-23. https://doi.org/10.1016/j.cld.2007.02.002
[18] Tomah S, Alkhouri N, Hamdy O. Nonalcoholic fatty liver disease and type 2 diabetes: where do Diabetologists stand? Clinical diabetes and endocrinology. 2020;6:1-1. https://doi.org/10.1186/s40842-020-00097-1
[19] Afzal MY, Anjum HS, Siddiqui UN, Shaihd S. Nonalcoholic fatty liver disease (NAFLD) frequency in Diabetes Mellitus (DM) type–II patients. FUUAST Journal of Biology. 2016;6(1):7-10. DOI: 2222-0356
[20] Bhatt KN, Pranav V, Dipika Y, Dharmesh N, Radhika N, Arvind S. Prevalence of nonalcoholic fatty liver disease in type 2 diabetes mellitus and its relation with insulin resistance in South Gujarat Region. Journal of Mahatma Gandhi Institute of Medical Sciences. 2017;22(1):8-11. DOI: 10.4103/0971-9903.202001
[21] Butt A, Hamid S, Jafri W, Salih M, Haider Z, Akhter J. Prevalence and Risk Factors of NAFLD among Native South Asian Pakistani Patients with Type 2 Diabetes and Metabolic Syndrome: 332. Official journal of the American College of Gastroenterology| ACG. 2011;106:S131. DOI: SS-332
[22] Kanwal S, Ghaffar T, Aamir AH, Usman K. Frequency of non-alcoholic fatty liver disease in patients with type-2 diabetes mellitus and its associated risk factors. Pakistan Journal of Medical Sciences. 2021;37(5):1335. https://doi.org/10.12669%2Fpjms.37.5.4211
[23] Singh S, Kuftinec GN, Sarkar S. Non-alcoholic fatty liver disease in South Asians: a review of the literature. Journal of clinical and translational hepatology. 2017;5(1):76. https://doi.org/10.14218%2FJCTH.2016.00045
[24] Khademalhosseini M, Ranjbar E, Mohammadi R, Khalili P, Mehran M, Jalali N, Rajabi Z, Jamali Z. Dietary antioxidants and liver enzymes in Rafsanjan, a Region in Southeast Iran. Scientific Reports. 2023;13(1):8555. https://doi.org/10.1038/s41598-023-35385-0
[25] Kakehashi A, Suzuki S, Wanibuchi H. Recent Insights into the Biomarkers, Molecular Targets and Mechanisms of Non-Alcoholic Steatohepatitis-Driven Hepatocarcinogenesis. Cancers. 2023;15(18):4566. https://doi.org/10.3390/cancers15184566
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
