By Muhammed Faisal Rahim1, Masood Ahmed Shaikh2, Shireen Qassim Bham3, Shah Jabeen Khan4, Asad Afridi5, Sama UlHaq6, Tahir Ansari7
- Medical Education Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Anatomy Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Pediatrics Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Physiology Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Community Medicine Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Anatomy Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
- Medical Education Department & Medicine Department, Fazaia Ruth Pfau Medical College, Air University, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/018
How to cite: Rahim MF, Shaikh MA, Bham SQ, Khan SJ, Afridi A, Ulhaq S, Ansari T. Students’ perception of Simulation-based learning in Clinical Skills Lab: A One-year institutional experience at Fazaia Ruth Pfau Medical College. Pak J Med Dent. 2024;13(1): 102-107. Doi: 10.36283/PJMD13-1/018
Background: Clinical skills laboratory offers great potential for undergraduate medical education by introducing the students to innovative teaching and learning strategies that efficiently fill the gap between theoretical knowledge and clinical practice. Our study aimed to assess the initial perceptions and experiences of medical students for the newly established clinical skills laboratory at FRPMC.
Methods: It was a descriptive cross-sectional study conducted at FRPMC, with 100 medical students of the first-year M.B.B.S. participating in this study. During the academic year, study participants attended six modules from Feb to Dec 2020. A 5-point Likert scale questionnaire was given to each student at the end of the module. Data has been reported as Mean ± SD and an internal consistency evaluation form for each variable was calculated.
Results: A total of 100 students participated in the study, 90% of the study participants agreed that their overall skill lab experience of training in the skills lab was satisfactory. 68% of respondents felt that instructors play an important role in organizing and structuring the course material, and 58 to 61% said that the clinical skills training simulates a hospital setting where practicing on real patients would take place. The pre-reading materials and instructions should be provided in advance, according to 64% of students.
Conclusion Students’ perceptions and experiences of teaching clinical skills were generally positive. Students showed overall satisfaction over the motivational conducive environment, content taught, gaining confidence, learning procedural skills, and adequacy of the educational equipment for learners in the newly established CSL at FRPMC.
Keywords: Clinical skills, Learning, Teaching, Simulation training.
In recent decades the role of the clinical skills laboratory has drastically increased with an evolving medical curriculum1. Clinical skills laboratory offers great potential for undergraduate medical education, especially after the introduction of the spiral curriculum in the integrated modular system. The primary role of the skills lab is clinical skills training and the introduction of innovative teaching and learning strategies that efficiently fill the gap between theoretical knowledge and clinical practice2. Clinical skills laboratory provides a safe and simulated environment in which medical students can learn and practice their clinical skills without harming the real or actual patients, they have the privilege to practice their skills any number of times in a safe learning environment3. In the new millennium, where medical curriculum all over the world is evolving rapidly, medical students are expected to integrate basic science knowledge with clinical disciplines. The role of clinical skills laboratories in this regard plays a vital role in the acquisition of cognitive, psychomotor, and affective skills in an integrated manner4.
The term ‘clinical skills’ used in the context of clinical skills laboratory (CSL) refers to history-taking skills, physical examination skills, procedural skills, effective communication skills, teamwork, and professionalism. In addition, the type of learning that takes place at a simulation laboratory or clinical skills laboratory is called simulation-based learning, it takes place with the help of state-of-the-art manikins and models5. The educational equipment used at the clinical skills lab is called simulators, these simulators are divided into three major categories, high, medium, and low fidelity simulators6.
Most of the learning in the clinical skills lab takes place with teaching and learning strategies called simulated-based learning using manikins and models. In the integrated modular system,7 each module has some portion of psychomotor skills.8,9 The clinical skills lab plays an important role in imparting these psychomotor skills through a structured clinical skills program, especially in the pre-clinical years.10 The clinical skills lab at FRPMC has been functioning for the last three years with educational activities mainly focusing on pre-clinical years. The faculty teaching medical students’ clinical skills recently realized that to assess the effectiveness of the clinical skills lab and its curriculum, it is important to understand the initial perceptions and experiences of the students. This information will also help us decide the lab’s future course. Therefore, our study aimed to assess the initial perceptions and experiences of medical students for the newly established clinical skills laboratory at FRPMC.
The clinical skills curriculum for integrated modular systems was developed, and the clinical skills program has at least 3-4 psychomotor skills in each module to be learned at the clinical skills lab. A total of 18-22 different competencies of psychomotor skills were taught in the first-year MBBS program. The clinical skills program or curriculum was developed consisting of History taking skills, examination skills, and procedural and communication skills.
A descriptive cross-sectional study was carried out over ten months on 100 undergraduate medical students aged between 20 to 23 years who have attended clinical skills sessions in an integrated modular system of curriculum at Faizaia Ruth Pfau Medical College, Karachi. Convenient sampling was done and all 100 students of the first-year MBBS were added to this educational study. Informed written consent was obtained from study participants before conducting the study which was a part of the questionnaire. IRB approval (IRB: Refer No: IRB/32) was obtained before recruitment and data collection for this study. All students who had more than 75 percent attendance in the clinical skills sessions were included in the study while those who were absent or had less than 75 percent of attendance were excluded from the study. The study participants attended six modules in the integrated modular system from February 2020 to December 2020. A 5-point Likert scale questionnaire with 21 items consisting of a rating scale from strongly agree to strongly disagree was designed and distributed among students at the end of the module to determine students` perception and experiences of attending clinical skills sessions in an integrated modular system for the acquisition of cognitive and psychomotor skills.11. There was a total of 6 modules (Foundation 1, Haemopoietic, Musculoskeletal 1 & 2, Respiratory, and Cardiovascular system). comprising of history taking, examination, and procedural skills. The Instrument used was a questionnaire containing a total of 21 structured closed-ended items with a rating of 01 dedicated to strongly disagree and 5 to strongly agree for each item on a 5-point Likert scale.
Analysis of the questionnaires filled by the students was conducted for all modules. Data obtained through these questionnaires was analyzed using SPSS Version 21.0. Data has been reported as Mean ± SD, frequency charts and graphs were computed in the data analysis software along with internal consistency evaluation through Cronbach alpha values form for each variable was calculated.
As seen in Table 1. 90% of the study participants agreed that their overall skill lab experience of training in the skills lab was satisfactory, helped them in improving procedural skills & and gaining effective communication skills, motivated them to learn & helped in building up knowledge and skills of universal precautions. A total of 68% of respondents felt that instructors play an important role in organizing and structuring the course material, and 58 to 61% said that the clinical skills training simulates a hospital setting where practicing on real patients would take place. The pre-reading materials and instructions should be provided in advance, according to 64% of students.
Table 1: Perceptions and experiences of medical students for the newly established clinical skills laboratory at FRPMC.
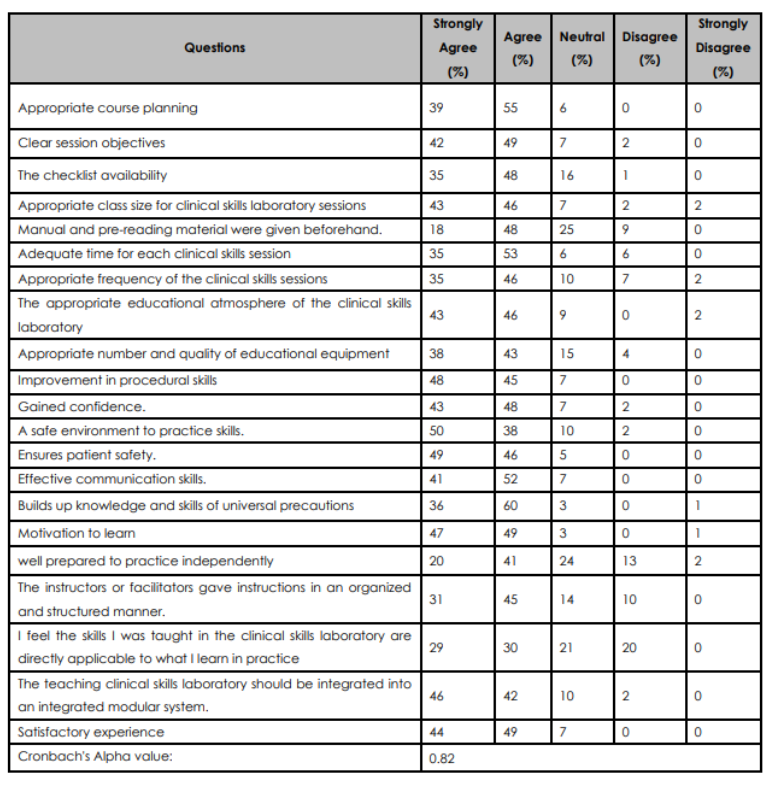
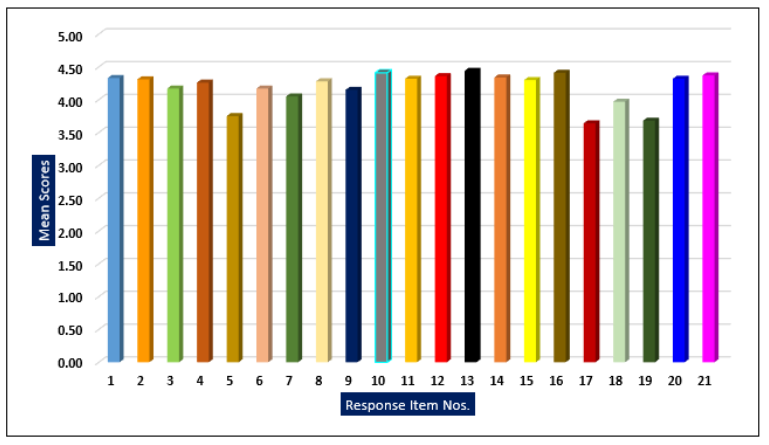
Figure 1: Mean score on a 5-point Likert scale.
In a medical curriculum where educational contents, especially in pre-clinical years are fully loaded with basic sciences subjects, the existence of a clinical skills program as a vertical theme takes lots of effort and is difficult to implement. Our efforts were focused on developing an evidence-based clinical skills program for the pre-clinical year which would benefit medical students to acquire effective psychomotor skills at every stage of the medical curriculum.
There are many advantages of introducing a clinical skills program in the early years of the medical curriculum. One study showed that the early introduction of clinical skills in the medical curriculum increases students’ interest and provides relevance to their studies12. According to our results, more than two-thirds of the class were satisfied with the program and the facility provided to them was conducive for learning. Wasson described that a better learning environment has a great impact on student learning and enhances students` problem-solving skills13. A study by Pande mentioned that skills taught practically have a greater impact on students` knowledge retention. Most students expressed pleasure with the program, but there was also a low level of agreement on the opinion that this clinical skills training mimics or is equivalent to what they learned in a hospital setting with real patients14. This argument is partly true as training in clinical skill laboratories would never be an alternative to training on real patients in a real hospital setting. Students attending skill labs already have the perception that the skill lab settings are artificial, not real as in hospitals. But at the same time, training in the clinical skills lab has many advantages as it improves skills related to communication skills, universal precautions, and assessment of skills done through the structured checked lists which provide objectivity in assessment, though the real effectiveness of clinical skills programs in preclinical years could only be measured if another study is done in later years comparing both tradition method with training in the clinical skills laboratory15. However, most of the students believed that a clinical skills training program helped in the acquisition of knowledge and skills for other subjects in the integrated curriculum and provided them with a good context of learning.
Most of the students in this study have consensus that the clinical skills laboratory is well equipped and its curriculum provides them with a safe learning environment to learn procedural skills, it also improves their communication skills and teaches them to follow universal precautions while doing any procedures. 96% of the study participants agreed that learning in a clinical skills laboratory creates interest and motivates students to learn new things. A study done by Zhaalts R and colleagues to investigate the association between motivation and learning environment has reported a significant correlation between motivation with learning environment16. Moreover, many clinical skills schools around the world have implemented clinical skills program as a vertical theme in the curriculum, which means the program runs parallel with other subjects of basic and clinical sciences, they have incorporated many skills like evidence-based medicine, bioethics, communication skills, and basic research skills in their program and running these programs successfully 17. Wright State University School of Medicine has a wonderful bioethics program of clinical skills laboratory, likewise, Harvard Medical School conducts a communication skills module in pre-clinical years similarly many other medical colleges are involved in conducting research, and evidence-based medicine modules in the clinical skills laboratory in fourth-year MBBS program18,19,20.
Moreover, it can be inferred from our results that a small percentage of students think that the clinical skills taught in the clinical skills laboratory have a limited role and application when it comes to replicating on real patients. This view can be respected but there is always an advantage to start something new and early in the curriculum which has clinical relevance and practical application in the curriculum. There is strong evidence to support this argument that whenever something new is introduced in the curriculum, there is always a little resistance from faculty and students as they look hesitant in this regard21.
Mixed responses were also observed when students gave feedback to instructors; there was a comparatively low rating on questions where they were asked if instructors were providing content in a structured and organized manner. The fact that the program’s instructors lacked the necessary qualifications to offer simulation-based instruction at the outset created a major issue. Most of the students believed that the program’s execution at the instructor level needed improvement, hence there is a need for a faculty development program for those instructors who are participating in skills training that focuses on simulation-based learning22.
There is much to learn and consider as we reevaluate our goals for the clinical skills lab. As time goes on, we anticipate that the clinical skills lab will play a significant role in medical education for both students and faculty and will reap significant benefits from integrating a variety of skills programs that are applicable, pertinent, and effective in fostering cognitive and psychomotor skills. Programs like Evidence-based Medicine, Clinical Research, BLS, ACLS, Pediatrics Life support, BLS, First Responders, ATLS, Personal Protective Equipment, crash courses on clinical skills, communication skills, and bioethics modules are a few programs that can be easily integrated into the undergraduate curriculum23,24.
Students’ perceptions and experiences of teaching clinical skills were generally positive. Students showed overall satisfaction over the motivational conducive environment, content taught, gaining confidence, learning procedural skills, and adequacy of the educational equipment for learners in the newly established CSL at FRPMC. As for future directions, we aim to evaluate the structure and functions of the CSL regular basis for new academic batches.
We would like to acknowledge Muhammad Azher Uddin, Research Data analyst for the analysis and formulation results of this study.
The authors declared no conflict of interest.
None
All participants were given a consent form before they filled out the questionnaire for their voluntary participation in this study. As this is educational research there was no patient involved or vulnerable subject involved in this study.
All authors contributed equally.
- Swanwick T. Understanding medical education. Understanding Medical Education: Evidence, Theory, and Practice. 2018:1-6.
- So HY, Chen PP, Wong GK, Chan TT. Simulation in medical education. Journal of the Royal College of Physicians of Edinburgh. 2019 r;49(1):52-57.
- Massoth C, Röder H, Ohlenburg H, Hessler M, Zarbock A, Pöpping DM, Wenk M. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC medical education. 2019;19:1-8
- Lateef F, Suppiah M, Chandra S, Yi TX, Darmawan W, Peckler B, Tucci V, Tirado A, Mendez L, Moreno L, Galwankar S. Simulation centers and simulation-based education during the time of COVID-19: A multi-center best practice position paper by the world academic council of emergency medicine. Journal of emergencies, trauma, and shock. 2021;14(1):3.
- Chernikova O, Heitzmann N, Stadler M, Holzberger D, Seidel T, Fischer F. Simulation-based learning in higher education: A meta-analysis. Review of Educational Research. 2020;90(4):499-541.
- Onturk ZK, Ugur E, Kocatepe V, Ates E, Ocaktan N, Unver V, Karabacak U. Use of simulation from high fidelity to low fidelity in teaching of safe-medication practices. JPMA. 2019;69:195-200.
- Yadollahi A, Yazdani S. Defining cognitive, higher order thinking, and psychomotor meta-skills: three-curricular content concept analysis. Journal of Medical Education. 2020;19(3).
- Wood YI, Zegwaard KE, Fox-Turnbull W. Conventional, remote, virtual and simulated work-integrated learning: A meta-analysis of existing practice. International Journal of Work-Integrated Learning. 2020;21(4):331-354.
- Andreatta P, Dougherty P. Supporting the development of psychomotor skills. Advancing Surgical Education: Theory, Evidence and Practice. 2019:183-196.
- Bracq MS, Michinov E, Arnaldi B, Caillaud B, Gibaud B, Gouranton V, Jannin P. Learning procedural skills with a virtual reality simulator: An acceptability study. Nurse education today. 2019;79:153-60.
- El Achi D, Al Hakim L, Makki M, Mokaddem M, Khalil PA, Kaafarani BR, Tamim H. Perception, attitude, practice and barriers towards medical research among undergraduate students. BMC medical education. 2020;20(1):1-1.
- So HY, Chen PP, Wong GK, Chan TT. Simulation in medical education. Journal of the Royal College of Physicians of Edinburgh. 2019;49(1):52-57.
- Wong BM, Headrick LA. Application of continuous quality improvement to medical education. Medical Education. 2021;55(1):72-81.
- Srivilaithon W, Amnuaypattanapon K, Limjindaporn C, Diskumpon N, Dasanadeba I, Daorattanachai K. Retention of Basic-life-support knowledge and skills in second-year medical students. Open Access Emergency Medicine. 2020:211-217.
- Lefor AK, Harada K, Kawahira H, Mitsuishi M. The effect of simulator fidelity on procedure skill training: a literature review. International journal of medical education. 2020;11:97.
- Zalts R, Green N, Tackett S, Lubin R. The association between medical students’ motivation with learning environment, perceived academic rank, and burnout. International journal of medical education. 2021;12:25.
- Bugaj TJ, Blohm M, Schmid C, Koehl N, Huber J, Huhn D, Herzog W, Krautter M, Nikendei C. Peer-assisted learning (PAL): skills lab tutors’ experiences and motivation. BMC medical education. 2019;19:1-4.
- de Lemos Tavares AC, Travassos AG, Rego F, Nunes R. Bioethics curriculum in medical schools in Portuguese-speaking countries. BMC Medical Education. 2022;22(1):199.
- Ibrahim MY, Yusof MR, Yaakob MF, Othman Z. Communication skills: Top priority of teaching competency. International Journal of Learning, Teaching and Educational Research. 2019;18(8):17-30.
- Hassan AK, Lampkin SJ, Hutcherson TC. Students’ perceptions of biostatistics following integration into an evidence-based medicine course series. Currents in Pharmacy Teaching and Learning. 2019;11(6):614-620.
- Jarvis MA, Baloyi OB. Scaffolding in reflective journaling: A means to develop higher order thinking skills
in undergraduate learners. International Journal of Africa Nursing Sciences. 2020;12:100195. - Rogers BA, Franklin AE. Cognitive load experienced by nurses in simulation-based learning experiences: An integrative review. Nurse education today. 2021;99:104815.
- Park YN, Cho BJ, Kim GY. The effects of out of hospital ACLS simulation training on the paramedic’s duty ability. Journal of the Korea Convergence Society. 2019;10(4):99-106.
- Adkoli BV. Assessment of professionalism and ethics. Journal of Education Technology in Health Sciences. 2019;6(1):2-9.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
