By Yusra Arshad1, Hudaibiya Ayub2, Nimra Akhtar3, Qurat-ul-Ain Usmani1
- Internal Medicine Department, Dr Ziauddin Hospital, Karachi, Pakistan
- Neurology Department, Dr Ziauddin Hospital, Karachi, Pakistan
- Community Medicine Department, Liaquat National Medical College, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/015
How to cite: Arshad Y, Ayub H, Akhtar N, Usmani QA. Risk Factors of Non-Invasive Ventilation Failure in COPD Patients Presenting with Acute Exacerbation. Pak J Med Dent. 2024;13(1): 81-87. Doi: 10.36283/PJMD13-1/015
Background: Non-invasive ventilation (NIV) is the first-line management for acute exacerbation of COPD (AECOPD), but some patients don’t improve and need invasive ventilation, leading to high mortality. We conducted a study to determine risk factors associated with NIV outcomes in these patients. Identifying predictive parameters of NIV failure could help timely intervention and prevent mortality.
Methods: A Quasi Single Arm study was conducted at a tertiary care Hospital, in Karachi, from July to December 2022. We studied 170 COPD patients admitted to Medicine Department and Medical ICU with acute respiratory failure, among those 170 patients 80 were male and 90 were female, aged above 40 and below 80 years.
Results: Among 170 AECOPD patients studied, 38% experienced NIV failure, while 61% had NIV success. In the NIV failure group, 38.46% of patients died in hospital. Most factors like quadrant infiltrate, weak cough reflex, low consciousness level, more requirements of oxygen, low pH, more respiratory rate, and positive blood cultures (p-value <0.001) were significantly associated with NIV failure and mortality, while others with no significant association still contributed towards NIV failure, like co-morbidities. Out of the 66 patients with NIV failure, 56% experienced immediate failure, 33% had early NIV failure, and 11% had late NIV failure.
Conclusion: Most identified risk factors significantly predicted NIV failure, suggesting they may serve as useful early indicators to guide intervention. Even non-significant factors still exhibited some association with NIV failure. Further research exploring additional predictors could optimize NIV outcomes and reduce mortality from AECOPD.
Keywords: COPD, Hospital mortality, Non-invasive Ventilation, Risk factors, Symptom Exacerbation.
Chronic Obstructive Pulmonary Disease (COPD) is a frequently avoidable and manageable condition. It leads to respiratory symptoms and persistent airflow restrictions caused by airways and alveoli abnormalities. These abnormalities are primarily the result of significant exposure to harmful particles or gases1. As per the guidelines established by GOLD (Global Initiative for Chronic Obstructive Lung Disease), an Acute Exacerbation of COPD (AECOPD) refers to a sudden decline in respiratory function that necessitates additional therapeutic intervention. This added need for treatment places a financial strain on the patient. Furthermore, repeated exacerbations of COPD not only increase the risk of mortality and medical complications but also contribute to a decline in lung function, ultimately diminishing the individual’s quality of life. Additionally, the utilization of healthcare services further adds to the financial burden2-3. Frequent occurrences of Acute Exacerbation of COPD (AECOPD) episodes lead to a decline in lung function among patients and significantly heighten the risk of mortality4. Non-invasive ventilation (NIV) has proven to be a beneficial treatment option for respiratory failure as it improves the survival rate and is also highly recommended for managing acute respiratory failure (ARF) in patients with COPD5-6. NIV in ARF reduces breathing effort, and respiratory muscle workload, and improves the respiratory rate, decreasing intubation needs. This helps avoid complications linked to invasive mechanical ventilation (IMV)7-8.
Management with NIV needs little to no sedation, and have lesser chances of developing ventilator-acquired pneumonia as compared to IMV and it gives larger morbidity and mortality benefit by avoiding prolonged IMV, tracheostomy, and prolonged weaning procedures, and their complications. NIV improves the consciousness level of the patients by reducing the partial pressure of carbon dioxide (PaCO2), which normalizes the arterial pH, and subsequently normalizes the cerebrospinal fluid pH9-10.
NIV is effective for AECOPD, but some patients don’t achieve the desired outcomes. Failure rates range from 15 to 24%. Transitioning to IMV after NIV failure increases in-hospital mortality compared to elective intubation before NIV failure11. Recognizing factors causing NIV failure is crucial. Take measures to overcome them or consider IMV before NIV failure. NIV failure is defined as emergency endotracheal intubation (ETI) or death12. Prior studies displayed inconsistent failure rates, making outcome prediction and identification of contributing factors challenging. Discrepancies may stem from variations in NIV failure timing, acidosis severity, and overall patient disease severity, including multi-organ failure13-14. This study identified factors causing NIV failure, and increasing mortality. By utilizing these predictors, we can reduce mortality in COPD patients with ARF. This study aimed to identify factors contributing to NIV failure in COPD patients with acute exacerbation. Therefore, by utilizing these risk factors we can decide to switch from NIV to IMV before the patient’s condition worsens.
A Quasi Single Arm study was conducted in the Medicine Department and Intensive Care Unit (ICU) of a tertiary care hospital in Karachi, after approval from the ethical research committee of the institution (4930222YAMED). The calculated sample size was 170 via the WHO calculator, with a 95% confidence interval. The absolute precision required was 0.07. Anticipated population proportion 1 was 0.115 and anticipated population proportion 2 was 0.119.
The inclusion criteria of the cases comprise of the COPD patients admitted to the Medicine Department and Medical ICU with ARF, aged above 40 and below 80 years, of either gender. Cases were labeled as COPD if i) they have a history of smoking at least 20 packs for years, ii) having difficulty in breathing, chronic cough, production of sputum, and/or a medical history of environmental exposure linked to COPD, iii) Patients diagnosed as COPD based on spirometry, iv) Patients previously treated as COPD or currently being treated as COPD by attending physician. Cases were excluded from the research if i) Patients were below 40 or above 80 years of age, ii) If patients/family refused to participate in the study, iii) If patients/family signed do-not-attempt-resuscitation orders, iv) If patients diagnosed other than COPD or not fit in above criteria of COPD. Informed consent was signed by either the patient or the next of kin.
The application of NIV was performed according to the hospital’s set criteria. ETI was performed if respiratory failure worsened. When intubation or mortality happened, it was recorded as NIV failure. The time duration in which NIV failure happened and the risk factors present in such patients were noted in the proforma used for data collection.
SPSS version 27 was used for data analysis. Shapiro Wilk test checked the normality of continuous variables (like age). Mean and standard deviations were calculated for normally distributed variables (like age in our data), while the median (IQR) was reported for non-normality distributed ones. Mann-Whitney U test compared continuous data. Percentages and frequencies measured qualitative variables like gender, weak cough reflex, non-invasive ventilation failure, and in-hospital mortality.
A total of 170 patients were included in this study, the mean age was 66 ± 12 years ranging from 40–80 years, 21 patients between 40-49 years, 40 patients between 50-59 years, 60 patients between 60-69 years, and 49 patients between 70-80 years.
We found a highly significant association of quadrant filtration, weak cough reflex, excessive secretions, hypercapnic encephalopathy, poor Arterial Blood Gases (ABGs), severity of illness, disruption of circadian sleep cycle, and blood cultures with the non-invasive ventilation status (p<0.001). There is an insignificant association of non-invasive ventilation status was found with gender (p=0.541), diabetes (p=0.441), hypertension (p=0.263), chronic kidney disease (p=0.308), ischemic heart disease (p=0.303) and increased expired tidal volume (p=0.561). We also found a significant association of intolerance (p=0.018), agitation (p=0.018), and hospital-acquired pneumonia (P=0.019) with the non-invasive ventilation status (Table 01).
Table 1: Association of different characteristics with non-invasive ventilated status
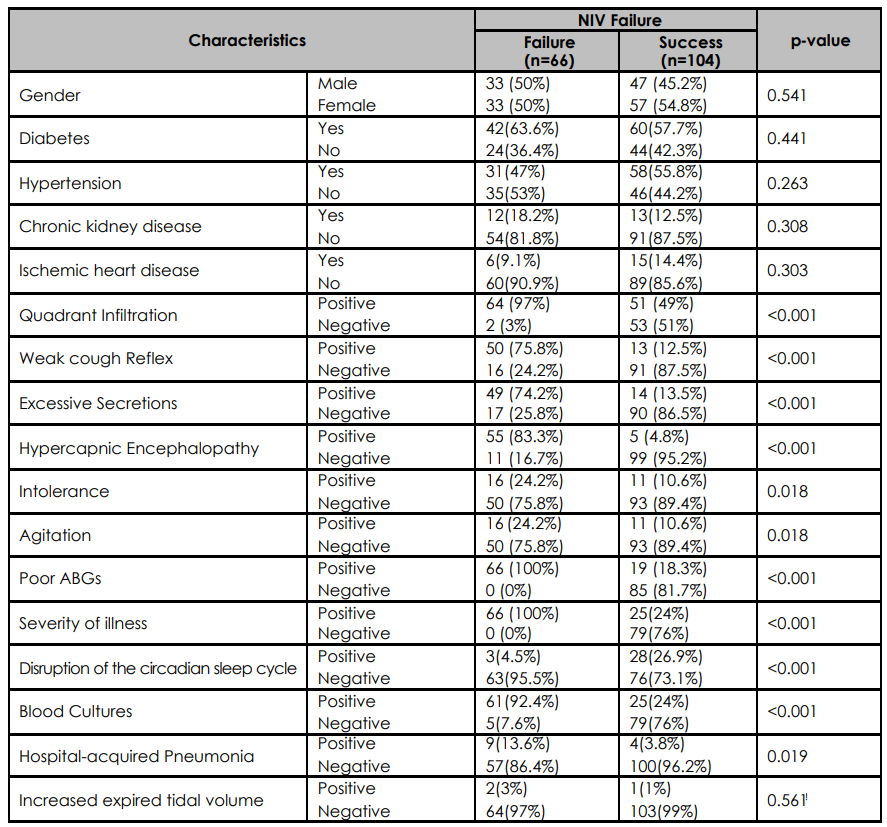
*Statistically significant values <0.05 by Chi-square or Fisher Exact test
There was a significant association of quadrant filtration, weak cough reflex, excessive secretions, hypercapnic encephalopathy, poor ABGs, severity of illness, blood cultures, and non-invasive ventilation status with mortality. (p<0.001). There is an insignificant association of mortality was found with gender (p=0.949), diabetes (p=0.460), hypertension (p=0.287), chronic kidney disease (p=0.952), ischemic heart disease (p=0.412), intolerance (p=0.415), agitation (p=0.415), and hospital-acquired pneumonia (P=0.081) and increased expired tidal volume (p=0.555). We also found a significant association between disruption of the circadian sleep cycle the mortality (p=0.003) (Table 02).
Table 2: Association of different characteristics with mortality
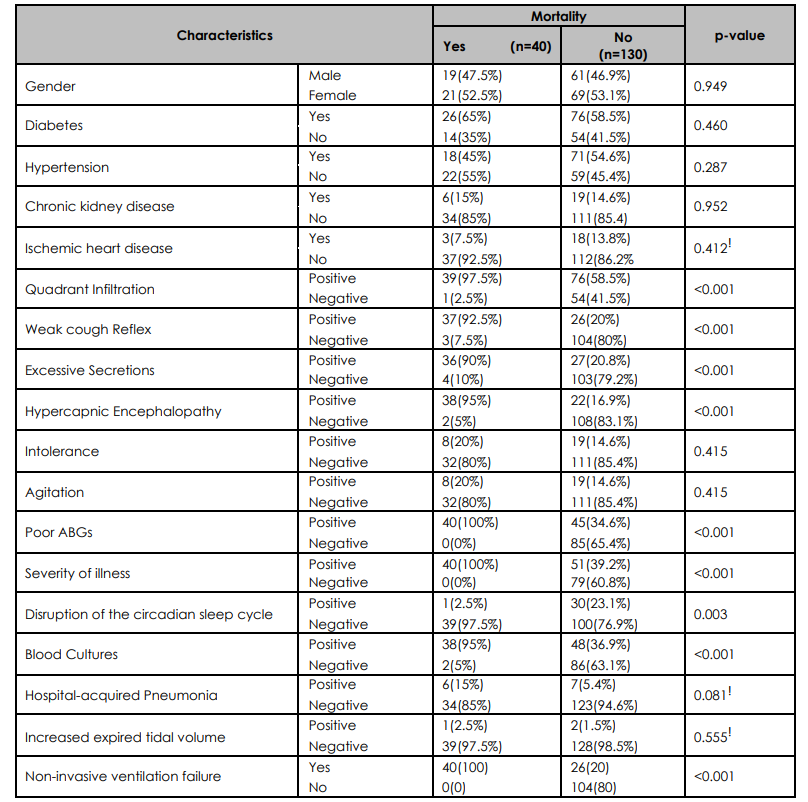
*Statistically significant values<0.05 by Chi-square or ǂFisher exact test.
The comparison of respiratory rate, pH, and PCO2 at the time of admission among non-invasive ventilation status was presented in Table 3. The median respiratory rate at the time of admission for the NIV failure group was 24 with an IQR of 6, while it was 22 with an IQR of 4 for the NIV success group. The p-value <0.001 suggested a statistically significant difference in the respiratory rate between the two groups at the time of admission. The median pH at the time of admission for the NIV failure group was 7.1 with an IQR of 0.2, while it was 7.3 with an IQR of 0.1 for the NIV success group. The p-value <0.001 suggested a statistically significant difference in the PH between the two groups at the time of admission. The median PCO2 at the time of admission for the NIV failure group was 67.5 with an IQR of 29, while it was 41 with an IQR of 8 for the NIV success group. The p-value <0.001 suggested a statistically significant difference in the PCO2 between the two groups at the time of admission.
Table 3: Comparison of respiratory rate, pH, and PCO2 at admission among NIV status
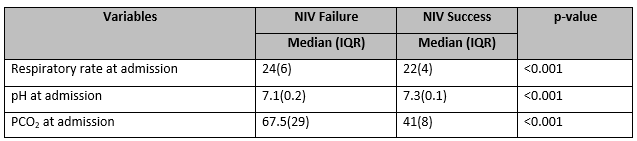
*Statistically significant values <0.05 by Non-parametric Mann-Whitney U test
Out of 170 cases, 66 (38%) experienced NIV failure while 104 (61%) had NIV success, and 40 (23.5%) participants died in hospital. Figure 1 shows NIV failure concerning timings that are immediate, early, or late.
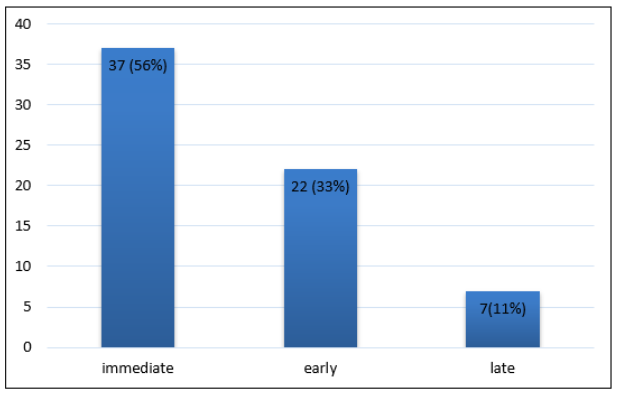
Figure 1: Non-invasive ventilation time in NIV Failure (n=66)
In this study, we focused on the parameters that can predict NIV failure in less than 1 hour of admission, between 1 to 48 hours of admission, and after 48 hours of admission of NIV. These three temporal moments are based on randomized control trials (RCTs) 1) immediate failure (within minutes to <1 hour), 2) early failure (1 to 48 hours), and 3) late failure (after 48 hours) 12,15-17. We studied 170 COPD patients who presented with acute respiratory failure. Of these patients 80 (47%) were male and 90 (53%) were female. The ages of the patients were above 40 and below 80 years. Out of 170 patients, 66 (38%) experienced NIV failure while 104 (61%) experienced NIV success. Out of 66, 37 were immediate, 22 were early and 7 were late NIV failure. In those who experienced NIV failure 40 (38.46%) patients died in hospital. In the NIV success group, there were 33 males (50%) and 33 females (50%) while in the NIV failure group, there were 47 males (45%) and 57 females (55%), shows there is no significant association of gender with NIV failure. In the NIV failure group, 64 patients (97%) had quadrant infiltration, while only 2 patients (3%) did not. The association of quadrant infiltration with NIV failure is proven in previous studies, it was a major complication at the time of admission which led to NIV failure in our study 18-20. Quadrant infiltration was also significantly associated with mortality after NIV failure. Factors present upon admission – especially quadrant infiltration, low Glasgow Coma Scale (GCS), reduced oxygenation, and higher Fraction of Inspired Oxygen (FiO2) needs – indicated heightened risk of NIV failure. GCS remained a robust predictor over the next 48 hours. Moreover, weak cough reflex, excessive secretions, hypercapnic encephalopathy (more specifically with 1 hour of NIV), Intolerance (especially mask intolerance), Agitation, and Poor ABGs are also significantly associated with NIV failure in our study as well as in previous studies 21-23. Research has shown that the outcome of NIV is favorable in acute hypercapnic encephalopathy as compared to other causes of encephalopathy 24-26. However, in our study, NIV is more successful in cases with higher GCS regardless of hypercapnia. The respiratory rate at the time of presentation was higher in patients who developed NIV failure. Respiratory failure was also significantly associated with mortality. Low pH and higher PCO2 at the time of presentation were also significantly associated with NIV failure and mortality. Hospital-acquired respiratory infections, septicemia, and positive cultures were responsible for poor outcomes and potentially associated with mortality. An increase in PO2 after 1 hour of administration of NIV and reduced requirements of oxygen is associated with favorable outcomes.
Our study results showed that factors at admission predict NIV failure low GCS, weak lungs, and high oxygen needs. Places with fluid in the lungs correlated with failing non-invasive ventilation within 48 hours, as did poor response of blood gases to treatment. Thirteen was the minimum GCS score for success. Factors like struggling to breathe, extreme secretions, and confusion often meant non-invasive ventilation failed. However, higher GCS scores meant non-invasive ventilation worked better. Infections and severe illness correlated with death. Factors like gender, diabetes, hypertension, chronic kidney disease, ischemic heart disease, intolerance, agitation, hospital-acquired pneumonia, and increased expired tidal volume were not significantly associated with NIV failure. Hospital-acquired pneumonia and co-morbidities can still contribute towards NIV failure and mortality with other factors.
The NIV failure rate of our study was 38.8% and mortality was 38.6%. Only 7 patients among 66 patients in the NIV failure group, developed NIV failure after 48 hours, this limits our study in evaluating risk factors associated with late NIV failure. This study provides us information that admission exam findings especially low Glasgow Coma Scale, increased respiratory rate, poor oxygenation, high oxygen demands, and weak cough reflex and a few investigations like ABGs and chest x-rays can be useful in predicting NIV failure among COPD patients presenting with acute respiratory failure. If this kind of study is ever conducted on a larger scale, including more hospitals, it will provide us with more useful information about NIV failure and risk factors.
Late NIV failure risk factors were under-reported due to low cases developing failure after 48 hours. If this study is expanded in the future to encompass a broader range of hospital setups, we can delve deeper into additional risk factors, particularly those linked to late-onset NIV failure.
Quadrant infiltrate, diminished consciousness, heightened oxygen needs, low pH levels, and elevated respiratory rates strongly correlate with NIV failure and subsequent mortality. These risk indicators can be identified through basic clinical examinations or straightforward tests such as ABGs and chest radiographs. Our findings emphasize that despite an initially positive response, patients might still encounter NIV failure, warranting ongoing monitoring. In cases of non-improvement, prompt endotracheal intubation (ETI) is advisable, as mortality and complications escalate following unsuccessful NIV treatment.
I would like to thank my teachers, Dr. Ejaz Ahmed Vohra (Prof. of Medicine), Dr. Syed Ali Abbas, and my senior Dr. Shan ul Haq Siddique for all their support and guidance.
The authors declared no conflict of interest.
Approval from the Ethical Review Committee of the relevant institution. (Reference Code: 4930222YAMED).
Informed consent was taken from the patients.
YA apprehended the idea of the research, did the relevant literature search, and drafted the manuscript, HA helped in the literature search, and NA, and QU authors participated in data acquisition. YA also provides clinical support to the patients who participated in this study.
- Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. American journal of respiratory and critical care medicine. 2017;195(5):557-582. https://doi.org/10.1164/rccm.201701-0218PP
- Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha J. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847-852. http://dx.doi.org/10.1136/thorax.57.10.847
- Miravitlles M, Ferrer M, Pont A, Zalacain R, Alvarez-Sala JL, Masa F, Verea H, Murio C, Ros F, Vidal R. Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004;59(5):387-395. http://dx.doi.org/10.1136/thx.2003.008730
- Meeraus WH, DeBarmore BM, Mullerova H, Fahy WA, Benson VS. Terms and definitions used to describe recurrence, treatment failure and recovery of acute exacerbations of COPD: a systematic review of observational studies. International Journal of Chronic Obstructive Pulmonary Disease. 2021:3487-3502. https://doi.org/10.2147/COPD.S335742
- Callegari J, Magnet FS, Taubner S, Berger M, Schwarz SB, Windisch W, Storre JH. Interfaces and ventilator settings for long-term noninvasive ventilation in COPD patients. International Journal of Chronic Obstructive Pulmonary Disease. 2017:1883-1889. https://doi.org/10.2147/COPD.S132170
- Roberts CM, Stone RA, Buckingham RJ, Pursey NA, Lowe D. Acidosis, non-invasive ventilation and mortality in hospitalized COPD exacerbations. Thorax. 2011;66(1):43-48. http://dx.doi.org/10.1136/thx.2010.153114
- Ko FW, Chan KP, Hui DS, Goddard JR, Shaw JG, Reid DW, Yang IA. Acute exacerbation of COPD. Respirology. 2016;21(7):1152-1165. https://doi.org/10.1111/resp.12780
- Wedzicha JA, Miravitlles M, Hurst JR, Calverley PM, Albert RK, Anzueto A, Criner GJ, Papi A, Rabe KF, Rigau D, Sliwinski P. Management of COPD exacerbations: a European respiratory society/American thoracic society guideline. European Respiratory Journal. 2017;49(3). https://doi.org/10.1183/13993003.00791-2016.
- Gonçalves G, Saeed H, Abdelrahim ME, Harb HS, Madney YM, Eng K, Karim HM, El-Khatib M, Mina B, Skoczyński S, Sarc I. Non-invasive ventilation in patients with an altered level of consciousness. A clinical review and practical insights. Advances in respiratory medicine. 2020;88(3):233-244. https://doi.org/10.5603/ARM.2020.0110
- Yeung J, Couper K, Ryan EG, Gates S, Hart N, Perkins GD. Non-invasive ventilation as a strategy for weaning from invasive mechanical ventilation: a systematic review and Bayesian meta-analysis. Intensive care medicine. 2018; 44:2192-2204. https://doi.org/10.1007/s00134-018-5434-z
- Duan J, Wang S, Liu P, Han X, Tian Y, Gao F, Zhou J, Mou J, Qin Q, Yu J, Bai L. Early prediction of noninvasive ventilation failure in COPD patients: derivation, internal validation, and external validation of a simple risk score. Annals of Intensive Care. 2019;9: 1-10. https://doi.org/10.1186/s13613-019-0585-9
- Ozyilmaz E, Ugurlu AO, Nava S. Timing of noninvasive ventilation failure: causes, risk factors, and potential remedies. BMC Pulmonary Medicine. 2014;14(1):1-10. http://www.biomedcentral.com/1471-2466/14/19
- Plant PK, Owen JL, Elliott MW. Non-invasive ventilation in acute exacerbations of chronic obstructive pulmonary disease: long term survival and predictors of in-hospital outcome. Thorax. 2001;56(9):708-712. http://dx.doi.org/10.1136/thx.56.9.708
- Carlucci A, Delmastro M, Rubini F, Fracchia C, Nava S. Changes in the practice of non-invasive ventilation in treating COPD patients over 8 years. Intensive care medicine. 2003;29: 419-425. DOI: 10.1007/s00134-002-1574-1
- Lemyze M, Taufour P, Duhamel A, Temime J, Nigeon O, Vangrunderbeeck N, Barrailler S, Gasan G, Pepy F, Thevenin D, Mallat J. Determinants of noninvasive ventilation success or failure in morbidly obese patients in acute respiratory failure. PloS one. 2014;9(5):e97563. https://doi.org/10.1371/journal.pone.0097563
- Liu Y, An Z, Chen J, Liu Y, Tang Y, Han Q, Lu F, Tang H, Xu Z. Risk factors for noninvasive ventilation failure in patients with post-extubation acute respiratory failure after cardiac surgery. Journal of Thoracic Disease. 2018;10(6):3319. doi: 10.21037/jtd.2018.05.96
- Scala R. Challenges on non-invasive ventilation to treat acute respiratory failure in the elderly. BMC Pulmonary Medicine. 2016;16(1):1-10. DOI 10.1186/s12890-016-0310-5
- Rodríguez A, Ferri C, Martin-Loeches I, Díaz E, Masclans JR, Gordo F, Sole-Violán J, Bodí M, Avilés-Jurado FX, Trefler S, Magret M. Risk factors for noninvasive ventilation failure in critically ill subjects with confirmed influenza infection. Respiratory Care. 2017;62(10):1307-1315. https://doi.org/10.4187/respcare.05481
- Suttapanit K, Boriboon J, Sanguanwit P. Risk factors for non-invasive ventilation failure in influenza infection with acute respiratory failure in emergency department. The American Journal of Emergency Medicine. 2021;45: 368-373. https://doi.org/10.1016/j.ajem.2020.08.094
- Pham T, Pesenti A, Bellani G, Rubenfeld G, Fan E, Bugedo G, Lorente JA, do Vale Fernandes A, Van Haren F, Bruhn A, Rios F. Outcome of acute hypoxaemic respiratory failure: insights from the LUNG SAFE Study. European Respiratory Journal. 2021;57(6). DOI: 10.1183/13993003.03317-2020
- Maggiorelli C, Ciarleglio G, Granese V, Maccari U, Manta C, Madioni C, Scala R. Integrated therapeutic strategy during noninvasive ventilation in a patient with end-stage respiratory disease. Respiratory Care. 2015;60(4):e80-85. https://doi.org/10.4187/respcare.03303
- Hadda V, Chawla G, Tiwari P, Madan K, Khan MA, Mohan A, Khilnani GC, Guleria R. Noninvasive ventilation for acute respiratory failure due to noncystic fibrosis bronchiectasis. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2018;22(5):326. doi: 10.4103/ijccm.IJCCM_474_17
- Hong Y, Duan J, Bai L, Han X, Huang S, Guo S. Noninvasive ventilation failure in pneumonia patients≥ 65 years old: the role of cough strength. Journal of Critical Care. 2018;44: 149-153. https://doi.org/10.1016/j.jcrc.2017.11.008
- Comellini V, Pacilli AM, Nava S. Benefits of non‐invasive ventilation in acute hypercapnic respiratory failure. Respirology. 2019;24(4):308. https://doi.org/10.1111/resp.13469
- Lemyze M, De Palleja G, Guiot A, Bury Q, Jonard M, Granier M, Thevenin D, Mallat J. Outcome of frail do-not-intubate subjects with end-stage chronic respiratory failure and their opinion of noninvasive ventilation to reverse hypercapnic coma. Respiratory care. 2019;64(9):1023-1030. https://doi.org/10.4187/respcare.06346
- Gonçalves G, Saeed H, Abdelrahim ME, Harb HS, Madney YM, Eng K, Karim HM, El-Khatib M, Mina B, Skoczyński S, Sarc I. Non-invasive ventilation in patients with an altered level of consciousness. A clinical review and practical insights. Advances in respiratory medicine. 2020;88(3):233-244. https://doi.org/10.5603/ARM.2020.0110
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
