By Naseem Munshi1, Muhammad Khalid2, Muhammad Naseem3, Khadijah Abid4
- Orthopedics Department, OPD Ziauddin Medical University, Karachi, Pakistan
- Orthopedic Department, Bantva Memon Hospital, Karachi, Pakistan
- Orthopedics Department, Karachi Medical and Dental College, Karachi, Pakistan
- Public Health Department, Faculty of Life Sciences, SZABIST, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/017
How to cite: Munshi N, Khalid M, Naseem M, Abid K. Proximal Fibular Osteotomy Vs Proximal Fibular Osteotomy with Intra-Articular Hyaluronic Acid: Difference in Terms of Pain Relief and Functional Outcome. Pak J Med Dent. 2024;13(1): 96-101. Doi: 10.36283/PJMD13-1/017
Background: Knee osteoarthritis (OA) is a complex, progressive illness marked by cartilage deterioration and adjacent bone enlargement, and management is challenging due to poor connective tissue self-regeneration. This study compared the effects of proximal fibular osteotomy (PFO) alone versus PFO with intra-articular hyaluronic acid injections (IAHA) among patients presenting with knee OA.
Methods: A quasi-experimental study was done at Ziauddin Hospital’s orthopedics department from March 2020 to March 2021. Patients with medial compartment knee joint OA requiring surgery aged≥40 years and BMI of <30kg/m2 were included. All participants were assigned into two groups, PFO was done alone in group A (n=30) and with IAHA in group B (n=30). Both groups had their medial joint spaces measured and documented pre- and post-operatively, as well as their Oxford knee score and visual analog scale (VAS). SPSS version 25 was used and the normality of data was assessed using Shapiro-Wilk’s test. The mean difference (post-pre) was compared using the Mann-Whitney U test. A p≤0.05 was statistically significant.
Results: A total of 60 patients were included with a mean age of 51.30±4.87 in Group A and 50.83±6.17 in Group B. Outcomes in both groups were improved considerably with a significant p<0.0001 in groups, in terms of pain and function determined using Oxford knee score, medial joint space measurement, and VAS score.
Conclusion: PFO alone and PFO with IAHA show significantly improved results in terms of functional outcomes, but the use of IAHA in combination with PFO, has considerably better results in terms of pain relief.
Keywords: Intra-Articular Injection, Knee osteoarthritis, Osteoarthritis, Osteotomy.
Knee osteoarthritis (OA) is a complex, progressive illness marked by cartilage deterioration and adjacent bone enlargement1, 2. Knee OA is expected to affect 16 percent of the global population and 203/10,000 person-years3. Increased BMI, advanced age, feminine gender, physical inactivity, trauma, and misalignment are all associated with it1. Malalignment can cause uneven load distribution inside the knee joint, exerting extra stress on a specific area of articular cartilage. An increase in breakdown products is caused by a local biochemical process involving pro-inflammatory cytokines, free radicals, and proteinases, affecting articular cartilage homeostasis and lowering synovial fluid viscosity4.
Previously, Total Knee Arthroplasty (TKA) was the only choice for orthopedic surgeons. Even though it provides pain relief and deformity repair, it is not the therapy of choice for the young population5. Uni-compartment knee arthroplasty (UKA) is another option for TKA. Although this treatment is connected to a faster recovery time and fewer problems, it is also linked to a greater risk of reoperation6. High tibial osteotomy (HTO). is another popular procedure, especially among young patients7. HTO is a technically difficult operation that can result in problems such as neurovascular damage, iatrogenic fracture, and non-union. Furthermore, many individuals may require TKA correction in the future 8, 9.
Proximal Fibular Osteotomy (PFO) has gained popularity in recent years as a treatment option for individuals with medial compartment knee OA. It is far more popular in the East (China and India) than in the West.10 Its appeal stems from the fact that it is a simpler, less costly treatment with superior functional results. It is more likely to be used than alternative procedures like UKA, HTO, and TKA in younger populations and patients with multiple co-morbidities11. A study revealed that pain scores dramatically decreased from 6.4 (baseline) to 2.1 (postoperatively after 1 year) among 30 patients treated with PFO10.
Intra-articular hyaluronic acid (IAHA) injections have recently gained popularity as a therapy for knee OA.12 Restoration of the elastic and viscous characteristics of the synovial fluid, anti-inflammatory and anti-nociceptive actions, and regulated hyaluronic acid production are all advantages of IAHA injections8, 9. A review of 8 meta-analyses reported, that patients with knee OA treated with IAHA treatment showed substantial improvement in stiffness, function, and pain for up to 26 weeks when compared to controls12.
PFO and IAHA, both techniques, might theoretically be employed together to generate synergistic benefits for restoring normal architecture and delaying disease progression. As a result, we examined the effects of PFO alone versus PFO with IAHA injections in terms of pain relief and functional outcomes in this study.
It was a quasi-experimental study conducted at the orthopedics department of Dr. Ziauddin University Hospital, Karachi over 1 year from March 2020 to March 2021. A sample size of 24≈to 30 in each group was estimated on the Open Epi sample size calculator. Statistics of mean function sub scores as 67.63 ± 13.65 in the PFO group and 54.10±10.29 in the PFO plus IAHA group (considering 20% difference between groups), 99% confidence level, and 90% power of test were considered for sample size estimation13.
Patients with medial compartment knee joint OA who needed surgery, were age≥40 years and had a BMI of less than 30 kg/m2 were included in the study. Patients in whom conservative management was unsuccessful were also included in this study as they were good candidates for surgery. Whereas patients with morbid obesity, tri-compartmental or bi-compartmental OA, valgus knee deformity, inflammatory joint disease, or any infection in the knee joint were not included in this study. A non-random consecutive sampling technique was applied for sample selection.
Ethical review approval of Ziauddin Hospital Nazimabad was attained for the study (ERC #3092020). All the patients, included in this study, underwent clinical and radiological evaluation. PFO alone (group A) or with IAHA (group B) was performed after receiving written informed consent.
PFO was performed by cutting a single lateral incision in the fibula that measured 3-5 cm in length. Between the peroneus and soleus muscles, fascia was incised along the septum. Using an oscillating saw and an osteotome, a 2-3 cm portion of the fibula was removed 6 to 10 cm below the caput fibulae. The surgical site was irrigated with a large amount of normal saline, and the muscles, fascia, and skin were then sutured in layers.
For IAHA injection, the patient is placed in a supine position with the knee flexed slightly by placing a towel roll in the popliteal space. The needle insertion site was marked, a lateral suprapatellar approach was chosen, and the site of injection was marked one finger breadth above the patellar edge and one finger breadth lateral to the patellar edge, and the drug was injected. Pre and postoperatively, a weight-bearing x-ray of the diseased knee was taken in anteroposterior (AP) and lateral perspectives and medial and lateral joint spaces were measured and documented. At monthly intervals, VAS and Oxford knee score values were recorded before and after surgery.
The collected data was entered into SPSS version 25. The normality of the numeric data was assessed using Shapiro-Wilk’s test. Data such as age and pre- and post-Oxford Knee Score were normally distributed and therefore presented as mean ± standard deviation. Whereas pre- and post-VAS scores and pre- and post-medial joint space followed non-normal distribution and, therefore, presented as median and interquartile range. Qualitative variable such as gender was presented in the form of frequency and percentage. Change in Oxford knee score (pre and post) in both groups was assessed using a Paired t-test. Change in medial joint space (pre and post) and VAS score (pre and post) in both groups were assessed using the Wilcoxon Rank test. The mean difference (post-pre) in Oxford knee score and medial space between both groups was compared using an independent sample t-test (as the mean difference in Oxford knee score and medial joint space across groups followed normal distribution). The mean difference (post-pre) in VAS score between both groups was compared using the Mann-Whitney U test (as the mean difference in VAS score across groups followed a non-normal distribution). A p-value≤0.05 was considered statistically significant.
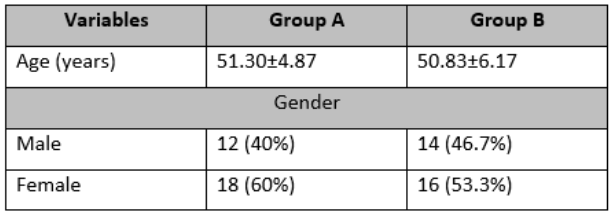
The sixty patients were between the ages of 40 and 65, with a mean age of 51.30±4.87 years in Group A and 50.83±6.17 years in Group B. In group A, there were 18 (60%) females and 12 (40%) males, whereas in group B, there were 16 (53.3%) females and 14 (46.7%) males.
Table 1: Baseline characteristics of both groups
Significant pain relief and improved joint function were observed in all patients using the Oxford knee scoring system at 1 year post-operatively, with an average increase of 14.78-15.20 points (as compared to pre-operative evaluation), with a score of 26.23±2.75 pre-operatively improving to 41.01±2.61 post-operatively in group A (p=0.001), and a score of 27.47±4.10 pre-operatively improving to 42.70±2.57 post-operatively (p=0.001). Similarly, weight-bearing lower-limb X-rays revealed an increase in the median medial knee joint space from 3.81 mm pre-operatively to 5.14 mm post-operatively in group A and from 3.79 mm pre-operatively to 5.21 mm post-operatively in group B, both with a significant p-value of ≤0.05. In group A, the median pain score fell from 8 pre-operatively to 4 post-operatively, while in group B, the median pain score decreased from 8 pre-operatively to 3 post-operatively, with a significant p-value of ≤0.05 in both groups.
Table 2: Comparative analysis of pre and post of Oxford knee score, medial joint space, and VAS score in both groups
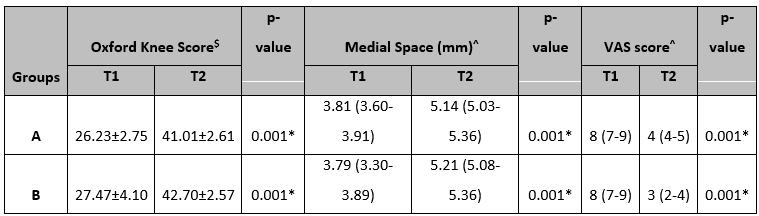
T1=Pre-operatively, T2=post-operatively at one year, Data presented as Mean±SD or Median (IQR), $ Paired t-test was applied, ^ Wilcoxon Rank test was applied *Significant at 5% level of significance
The mean difference in Oxford knee score and medial joint space was identical in both groups, according to an independent t-test. (Table 3)
Table 3: Comparative analysis of mean difference in Oxford knee score and medial joint space between both groups.
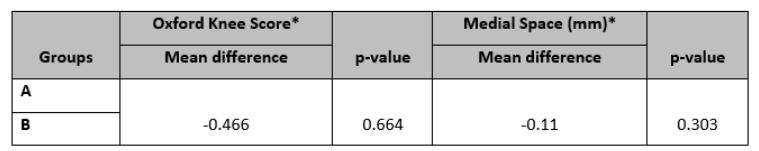
*An independent t-test was applied
Mann-Whitney U test revealed that the change in VAS score was significantly different between both groups (U=186, p=0.001). (Figure 1)
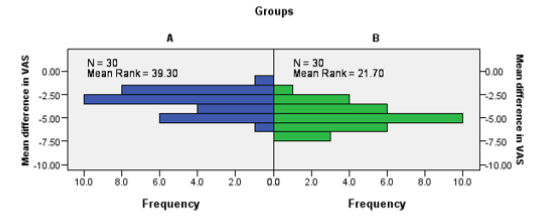
Figure 1: Comparison of change in VAS score between both groups.
PFO is based on the idea that non-uniform settling causes knee OA and accelerates its development14. The lateral section of the tibial plateau is supported by the fibula and associated soft tissues, but the medial side is exclusively supported by the medial tibial cortex. In light of this, the medial side experiences increased axial stress, resulting in non-uniform settlement and tibial plateau degeneration15. PFO is used to decrease the lateral fibular support, which subsequently shifts the stress from the medial to the lateral side, causing the varus deformity to be corrected and thereby impacting disease development16.
Intra-articular drug administration, on the other hand, which is a concentrated therapeutic dosage that is dispersed through the joint capsule, may be regarded as an optimal route of drug delivery in OA17. Intra-articular drug administration provides several advantages over systemic drug delivery, including higher local bioavailability, less systemic exposure to some medications, fewer side effects, and a lower cost10, 18, 19.
There are numerous studies and ample data about the benefits and use of PFO and IAHA individually, but there is no study has been conducted on the use of PFO and IAHA in combination. Hence, in the current study, we have compared the effects of PFO alone with PFO with IAHA injections in terms of pain relief and functional outcome. Our research demonstrates that while both PFO alone and PFO + IAHA have dramatically improved functional outcomes, the use of IAHA in conjunction with PFO has much superior pain reduction results. In individuals with knee OA, IAHA also lowers the requirement for additional analgesics such as NSAIDs, corticosteroids, and opioids, according to recent research20.
Retrospective database analyses show a 0.6–2.2-year delay in the need for TKR with 5 or more doses of IAHA, and up to 3.6 years with 5 or more doses of IAHA21-23. In a prospective comparative study of PFO and HTO for unilateral varus knee OA, Zou et al. found that the PFO group had a significantly lower operating time, peri-operative hemorrhage, time to full weight-bearing, VAS score, and post-operative complications24. PFO improved both the radiological look and function of varus knee OA, as well as long-term pain alleviation, according to Yang et al., who performed it in 156 patients with medial compartment knee OA25.
Both above-mentioned treatments give considerable advantages on their own, but when used together, they produce better results, particularly in terms of pain reduction. Some of the limitations were that assessing the results in the treatment of medial compartment osteoarthritis required a bigger sample size and a longer follow-up time. Another flaw was the lack of a control group. Because the patients were assigned at random, it is impossible to say which treatment approach will provide better results in whatever grade of OA. More research should be done in the future to assess how successful and safe these treatments are on a broader sample of persons with knee OA. This would help to broaden the therapeutic applicability of these methods.
In conclusion, our study highlights the efficacy of PFO and PFO + IAHA in enhancing functional outcomes. Notably, the addition of the IAHA with PFO yields superior pain relief. These findings advocate for a nuanced approach in clinical interventions, emphasizing the potential synergies for improved patient outcomes in pain management.
None.
The authors declared no conflict of interest.
Ethical review approval of Ziauddin Hospital Nazimabad was attained for the study (ERC #3092020).
All the patients, included in this study, underwent clinical and radiological evaluation. PFO alone (group A) or with IAHA (group B) was performed after receiving written informed consent.
NM Conceptualization, Methodology design, Manuscript writing and editing, and manuscript review. MK, MN Data collection and validation, manuscript drafting and revision, data entry and management. KA Data analysis and interpretation, manuscript review, and final approval.
- Hsu H, Siwiec RM. Knee Osteoarthritis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
- Primorac D, Molnar V, Rod E, Jeleč Ž, Čukelj F, Matišić V, et al. Knee Osteoarthritis: A Review of Pathogenesis and State-Of-The-Art Non-Operative Therapeutic Considerations. Genes. 2020;11(8):854
- Cui A, Li H, Wang D, Zhong J, Chen Y, Lu H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine. 2020;29 DOI: 10.1016/j.eclinm.2020.100587
- Ravalli S, Pulici C, Binetti S, Aglieco A, Vecchio M, Musumeci G. An Overview of the Pathogenesis and Treatment of Elbow Osteoarthritis. Journal of Functional Morphology and Kinesiology. 2019;4(2):30
- Varacallo M, Luo TD, Johanson NA. Total Knee Arthroplasty Techniques. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2023.
- Beckmann J, Meier MK, Benignus C, Hecker A, Thienpont E. Contemporary knee arthroplasty: one fits all or time for diversity? Arch Orthop Trauma Surg. 2021;141(12):2185-2194 DOI: 10.1007/s00402-021-04042-4
- Laprade RF, Spiridonov SI, Nystrom LM, Jansson KS. Prospective outcomes of young and middle-aged adults with medial compartment osteoarthritis treated with a proximal tibial opening wedge osteotomy. Arthroscopy: The Journal of Arthroscopic & related Surgery: official publication of the Arthroscopy Association of North America and the International Arthroscopy Association. 2012;28(3):354-364 DOI: 10.1016/j.arthro.2011.08.310
- Seo SS, Nha KW, Kim TY, Shin YS. Survival of total knee arthroplasty after high tibial osteotomy versus primary total knee arthroplasty: A meta-analysis. Medicine (Baltimore). 2019;98(30):e16609 DOI: 10.1097/md.0000000000016609
- Rai A, Saurabh A, Shekhar S, Kunwar A, Verma V. Proximal fibular osteotomy for pain relief and functional improvement in patients of osteoarthritis of knee. International Surgery Journal. 2019;6:2368 DOI: 10.18203/2349-2902.isj20192957
- Kakumanu R, Kunadharaju R, Ganesh C. Prospective study of functional and radiological outcome of proximal fibular osteotomy for medial compartment osteoarthritis in elderly. Journal of Orthopaedic Diseases and Traumatology. 2021;4(3):86-91 DOI: 10.4103/jodp.jodp_13_21
- Vaish A, Kumar Kathiriya Y, Vaishya R. A Critical Review of Proximal Fibular Osteotomy for Knee Osteoarthritis. The archives of bone and joint surgery. 2019;7(5):453-462
- Bhandari M, Bannuru RR, Babins EM, Martel-Pelletier J, Khan M, Raynauld JP, et al. Intra-articular hyaluronic acid in the treatment of knee osteoarthritis: a Canadian evidence-based perspective. Ther Adv Musculoskelet Dis. 2017;9(9):231-246 DOI: 10.1177/1759720×17729641
- Wang X, Wei L, Lv Z, Zhao B, Duan Z, Wu W, et al. Proximal fibular osteotomy: a new surgery for pain relief and improvement of joint function in patients with knee osteoarthritis. J Int Med Res. 2017;45(1):282-289 DOI: 10.1177/0300060516676630
- Yang Z-Y, Chen W, Li C-X, Wang J, Shao D-C, Hou Z-Y, et al. Medial compartment decompression by fibular osteotomy to treat medial compartment knee osteoarthritis: a pilot study. Orthopedics. 2015;38(12):e1110-e4
- Zheng Z, Sun Y, Zhang X, Chen W, Li S, Zhang Y. The pathogenesis and clinical imageology research of the knee osteoarthritis. J Hebei Med Univ. 2014;35(5):599-600
- Shanmugasundaram S, Kambhampati SB, Saseendar S. Proximal fibular osteotomy in the treatment of medial osteoarthritis of the knee–A narrative review of literature. Knee Surgery & Related Research. 2019;31(1):1-7
- Emami A, Tepper J, Short B, Yaksh TL, Bendele AM, Ramani T, et al. Toxicology evaluation of drugs administered via uncommon routes: intranasal, intraocular, intrathecal/intraspinal, and intra-articular. International journal of toxicology. 2018;37(1):4-27
- Cao Y, Ma Y, Tao Y, Lin W, Wang P. Intra-Articular Drug Delivery for Osteoarthritis Treatment. Pharmaceutics. 2021;13(12) DOI: 10.3390/pharmaceutics13122166
- Huang H, Lou Z, Zheng S, Wu J, Yao Q, Chen R, et al. Intra-articular drug delivery systems for osteoarthritis therapy: shifting from sustained release to enhancing penetration into cartilage. Drug Deliv. 2022;29(1):767-791 DOI: 10.1080/10717544.2022.2048130
- McIntyre LF, Bhattacharyya S, Yadalam S, Bisson B, Kim M. Impact of hyaluronic acid injections on utilization of pain management medications. Am J Pharm Benefits. 2017;9(6):195-199
- Mar J, Jurado MR, Arrospide A, Fidalgo AE, Lopez BS. Cost-analysis of viscosupplementation treatment with hyaluronic acid in candidate knee replacement patients with osteoarthritis. Revista Española de Cirugía Ortopédica y Traumatología (English Edition). 2013;57(1):6-14
- Delbarre A, Amor B, Bardoulat I, Tetafort A, Pelletier-Fleury N. Do intra-articular hyaluronic acid injections delay total knee replacement in patients with osteoarthritis–a Cox model analysis. PLoS One. 2017;12(11):e0187227
- Altman RD, Bedi A, Karlsson J, Sancheti P, Schemitsch E. Product differences in intra-articular hyaluronic acids for osteoarthritis of the knee. The American journal of sports medicine. 2016;44(8):215821-65
- Zou G, Lan W, Zeng Y, Xie J, Chen S, Qiu Y. Early clinical effect of proximal fibular osteotomy on knee osteoarthritis. Biomedical Research (0970-938X). 2017;28(21)
- Yang ZY, Chen W, Li CX, Wang J, Shao DC, Hou ZY, et al. Medial Compartment Decompression by Fibular Osteotomy to Treat Medial Compartment Knee Osteoarthritis: A Pilot Study. Orthopedics. 2015;38(12):e1110-1114 DOI: 10.3928/01477447-20151120-08
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
