By Amber Khalid1, Muhammad Ayoob1, Ambreen Masood1, Muhammad Nashit1, Faiza Zafar Sayeed1, Aveen Fatima1
- Ophthalmology Department, Ziauddin University Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/008
How to cite: Khalid A, Ayoob M, Masood A, Nashit M, Sayeed FZ, Fatima A. Preventing Ocular Surface Foreign Body Complications: Enhancing Awareness and Precaution. Pak J Med Dent. 2024;13(1): 37-43. Doi: 10.36283/PJMD13-1/008
Background: Ocular surface foreign bodies are the second most common emergency condition in the ophthalmology department OPD, which can be easily prevented through proper precautionary measures. Also, they can be either superficial or embedded into the cornea or conjunctiva. In this study, we aimed to create awareness regarding the prevention and management of such cases to reduce ocular complications.
Methods: This prospective cross-sectional study was carried out in the Ophthalmology department of Ziauddin University Hospital Karachi. The study duration was 4 years from 16th November 2019 to 15 November 2022. Patients presented to the ophthalmology department OPD with complaints of ocular foreign bodies were examined clinically and a total of 427 patients were included in the study who fulfilled the inclusion criteria. The data was collected and analyzed on SPSS 23. The chi-square test was used to compare the variables.
Results: Our study analyzed that ocular surface foreign bodies had a strong association with the profession. The metallic foreign bodies were found in 283(66.3%) patients and the remaining 144 (37.7%) were non-metallic. There was a strong correlation found between the type of foreign body and the site of ocular involvement. The p-value was significant with 0.0001.
Conclusion: The majority of ocular surface foreign bodies were workplace-related due to a lack of awareness of protective measures. A counseling workshop should be arranged regarding its importance for workers in their workplaces which will improve their work capacity, and health and reduce economic burden.
Keywords: Foreign Bodies, Eye Foreign Bodies, Ocular.
Ocular surface foreign bodies are one of the most common ocular emergencies1. Timely and appropriate management of ocular surface foreign body can reduce the risk of visual loss. The incidence of ocular surface foreign bodies greatly varies from region to region2,3. One of the Swedish studies documented the incidence of ocular injury 8.1% per 1000 and 40% out of these were corneal and conjunctival foreign bodies4. The majority of these types of injuries occurred at the workplace due to the lack of use of protective shields or high-risk professions such as welding, construction, carpentry, and agriculture5.
Ocular superficial foreign bodies can also occur during household work, playing sports, or even windy weather6,9. These foreign bodies can be metallic bodies such as iron, silver, and copper particles or non-metallic ones like dust particles, eyelashes, bird feathers, insects, vegetable particles, glass, etc. These ocular foreign bodies are less common in females, however, most of the ones found are usually either vegetable, fruit pieces or dust particles2,7. These foreign bodies can cause red eye associated with pain, irritation, photophobia, and clear watery discharge. Surface ocular foreign body removal needs a detailed slit lamp examination of the conjunctiva and cornea. The foreign body can be removed in the clinic, some superficial ones can be removed easily by a thorough eyewash, while the impacted ones need removal through forceps, needles, or cotton buds8.
Immediate removal of foreign bodies is important to reduce the risk of conjunctivitis, corneal ulcer, epithelial defect, and corneal scarring9. Some patients present after a few days with unsuccessful self-removal attempts. Patients have mentioned attempting self-removals using handkerchiefs, currency notes, and tissue papers. These lead to infections which may result in corneal abscess and corneal ulcer formation6,10. Therefore, our objective was to raise awareness about preventing and effectively managing cases of ocular surface foreign bodies to minimize ocular complications. This includes reducing the risk of post-injury complications related to the type of foreign body, the duration of the injury, and the method of removal. In this way, we can improve the quality of life, reduce the risk of visual impairment, and ensure that industrial workers are aware of the safety precautions necessary to avoid such accidents.
A prospective cross-sectional study was carried out in the Ophthalmology department of Ziauddin University Hospital Karachi. The duration of the study was 4 years from 16th November 2019 to 15 November 2022. A group of individuals who came in with eye OPD with complaints of foreign bodies in the eye was examined clinically and if met the inclusion criteria, were included in the study.
The inclusion criteria included patients with age above 15 years and with ocular foreign bodies without any penetrating injuries. As per the exclusion criteria, all patients with penetrating injuries with ocular foreign bodies, and a previous history of ocular surgery were not added to this study. A total of 427 patients diagnosed with surface ocular foreign bodies were included in this study based on consecutive sampling techniques. The study was reviewed and approved by the Ziauddin University ethical committee, reference no: 1491019MAOPH. Informed written consent was taken from all the patients.
A questionnaire form regarding patient demography and presenting complaints, the material of the foreign body, and the time and duration of injury was filled out by the resident medical officer. The patient was then examined thoroughly by a single ophthalmologist for a visual acuity test and a slit lamp examination for the location of the foreign body. Ocular surface foreign bodies were removed with the help of forceps, cotton buds, or 27-gauge needles under topical anesthesia proparacaine hydrochloride 1%. After removing the ocular surface foreign bodies’ cornea was stained with fluorescein stain for corneal abrasion or epithelial defect and topical antibiotics Moxifloxacin and Tobramycin in eye ointment were prescribed 5 times a day for 7 days. All patients were advised to visit the ophthalmologist for follow-up after 24 hours and again after 1 week. The complications related to the foreign bodies were documented on these follow-up visits. In case of corneal abscess or corneal ulcer, patients’ corneal and conjunctival swabs were also sent for culture sensitivity and staining. These patients were called for follow-up until their clinical signs were resolved.
The association between the etiology of foreign bodies and their locations was assessed. The data was analyzed and entered into SPSS version 23. Quantitative variables, such as age, will be presented in the form of mean ± standard deviation. Qualitative variables, such as gender, will be presented in the form of frequency and percentage. The comparative data will be analyzed by chi-square test with a significant p- p-value < 0.05.
A total of 427 patients based on inclusion criteria were included in this study. All patients were presented in the Ophthalmology department of Ziauddin Hospital Karachi. The incidence of ocular surface foreign body was 1.78%. The average age of the affected population was 36± 9.12. There were 366 (85.7%) men and 61 (14.3%) women, with men: women 6:1. A total of 353 (82.7%) patients did not use protective glasses, and 74 (17.3%) patients did have some type of protective shield or glasses. 248 (58%) of the patients were present in OPD within 24 hours of injury, 167 (39%) of the patients were present within 3 days and the last 12 (3%) were there within 7 days. 115 (27%) of the patients have tried self-removal or have had them removed by a coworker using tissues, coins, currency notes, and cotton buds. Topical anesthesia was given while removing the foreign body. 137 (32%) patients were using un-prescribed topical antibiotics or steroids. 269 (63%) foreign bodies were found in the right eye, 149 (34.9%) in the left eye, and in the remaining 9 (2.1%) cases foreign body was found in both eyes. Multiple corneal foreign bodies were found in 15(3.5%) cases. There were 327(76.6%) cases presented with 1st time and the remaining 100 (23.4%) cases had a history of the foreign body more than 1 time. Most patients had a corneal foreign body in 290 (68%) and a conjunctival foreign body in 137 (32%), the chi-square test statistic is 101.73 and p-value <0.00001.
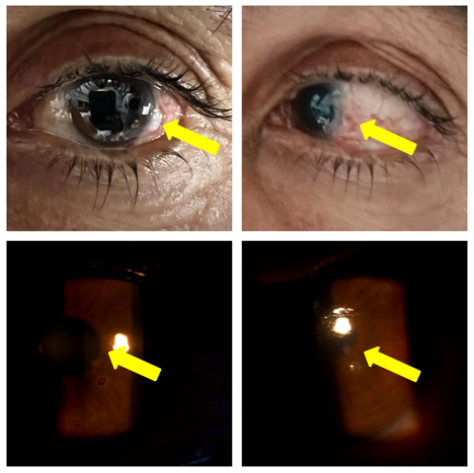
Figure 1: (a) showing vegetable particles at the limbus. (b) showing the patient’s eye after the removal of the particle. (c) shows a corneal metallic foreign body, and (d) shows the patient’s eye after the removal of the particle.
The metallic industrial workers were more commonly affected 265 (62.1%) followed by the constructor industry 39(9.1%), Farmers 37 (87.7%), trauma during domestic work 32 (7.5%), and the remaining 54(12.6%) miscellaneous profession. In the metallic industry, 162 (63.3%) patients were from the wielding occupation, 69 (27%) were from metal cutting, and 25 (9.7%) were from metal grinding. (Table 1)
Table 1: Correlation of type of foreign body with profession
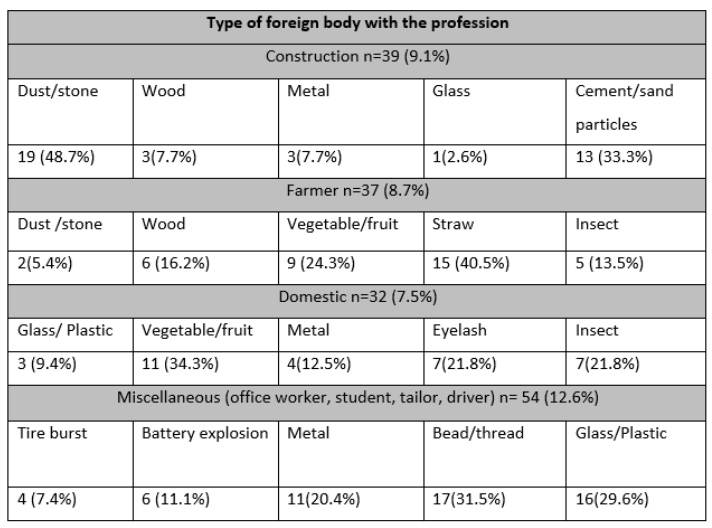
*The chi-square statistic is 101.73 and the p-value <0.00001.
The frequency of foreign bodies with relation to ocular distribution was 290(68%) in cornea, 73(17.1%) in superior palpebral conjunctivitis, 39(9.1%) in inferior palpebral conjunctivitis, 16(3.7%) in Fornix, 9(2.1%) in Caruncle. (Table 2) The chi-squared statistic is 101.72 and the p-value is 0.00001. The most common type of foreign body was the metallic foreign body which accounts for 283(66.3%) and the remaining 144 (37.7%) were non-metallic. A total of 274 (96.8%) metallic-foreign bodies were removed with the help of needles and 9 (3.2%) metallic-foreign bodies with forceps. 33 (22.9%) of the non-metallic foreign bodies were removed with forceps, 6(4.2%), and the rest of 105 (72.9%) were removed with needles. The rate of complication before and after the removal of metallic foreign bodies and non-metallic foreign bodies was assessed.
Table 2: Type of ocular foreign bodies in correlation to site.
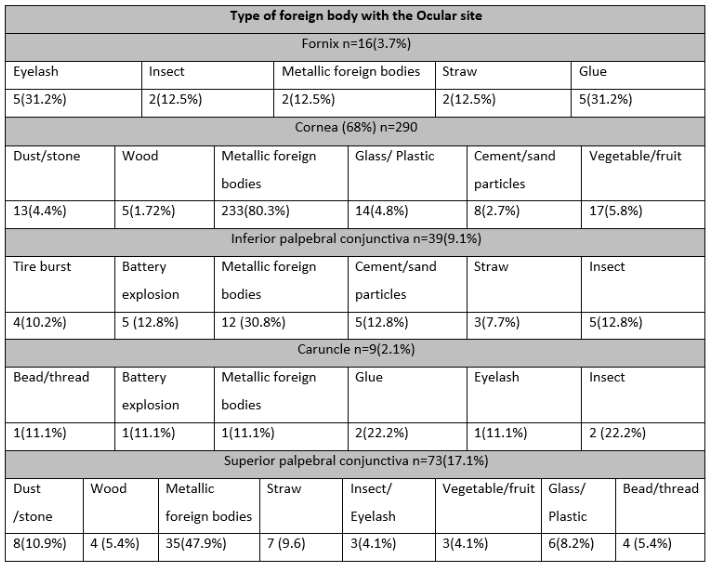
*The chi-square statistic is 101.73 and the p-value <0.00001
The complication rate at the time of presentation in metallic foreign body was 39(13.6%) in epithelial defect, 21(7.5%) in corneal abrasion, 133(47%) in rust ring, 16(5.8%) in incomplete removal, 79(28%) in conjunctivitis and 17(6%) in corneal abscess. The complication rate at the time of presentation in non-metallic foreign body was 7(4.9%) in epithelial defect, 3(2.3%) in corneal abrasion, 5(3.2%) in incomplete removal, 11(7.3%) in conjunctivitis and 3(2%) in corneal abscess. The chi-square statistic is 57.06 at p value 0.00001. The complication rates after removal of foreign bodies in the metallic foreign body were 40(14%) in rust ring, 91(32%) in epithelial defect, 59(21%) in conjunctivitis, 17(6%) in corneal abscess and 34(12%) in corneal scarring. The complication rates after the removal of foreign bodies in the non-metallic foreign body were 15(10%) in conjunctivitis, 4(3%) in corneal abscess, and 3(2%) in corneal scarring. (Table 3) The chi-square statistic is 53.64 and the p-value is 0.00001.
Table 3: Comparison of complication rate at the time of presentation and removal of foreign body.
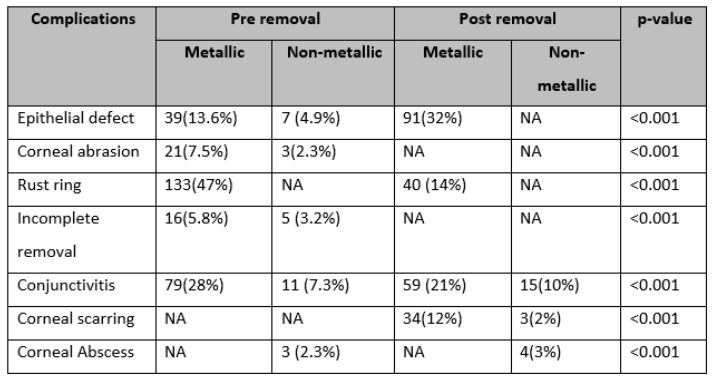
* A paired t-test was used to compare before and after results at a p-value <0.001.
The patients with epithelial defects and corneal abrasion were given topical Moxigan eye drops 5 times a day for a week with Tobrex eye ointment. They were called in for follow-up after 24 hours and 48 hours. The epithelial defect for all patients had healed by the 48-hour follow-up. The patients with corneal abscesses were followed up for 2 weeks and were given systemic antibiotics and topical Moxigan eye drops 5 times a day for a week with Tobrex eye ointment. The corneal abscess in these patients resolved within 7 days.
An ocular surface foreign body is an object such as glass, metal, or sand, which gets adhered to or embedded into different ocular surfaces11. These are commonly found in cornea and palpebral Conjunctival surfaces12,13. They are also found in caruncles, fornices, and subtarsal spaces. The surface ocular foreign bodies are common emergencies reported in the eye department. These patients usually try self-removal or visit a general practitioner which leads to incomplete removal, corneal abscess, and conjunctivitis14-16. These ocular surface foreign bodies are usually minute particles that are difficult to remove with the naked eye and required a slit lamp for efficient removal. These are removed with forceps and needles with only a minor iatrogenic trauma which usually doesn’t affect the patient’s vision. If the foreign body involves the visual axis and corneal stroma there will be corneal scarring which leads to visual impairment. It is an easily manageable ocular condition however improper or untimely treatment may lead to serious visual impairment17,18. Most of these are workplace injuries. Patients usually present with complaints of foreign body sensations associated with redness of the eye, watery discharge, and a history of trauma or something that went in their eyes19-21. These patients usually belong to low socio-economic status. The literacy rate among them is also low, the majority of them having only passed up to grade 5. There is a lack of awareness regarding the use of protective glasses and most workplaces don’t offer these to their workers. This results in workers being unaware that simple precautionary measures can prevent sight-threatening injuries22-24.
Research conducted by Bahoo et al also showed a strong association of the type of ocular surface foreign bodies and their association with the professions. The first incidence of foreign body fall was 782(75.6%), and repeated history was in 263(24.4%) patients. The foreign bodies were most commonly found in the cornea of the eyes25. In our study, the first incidence of foreign body patients was 327(76.6%) while repeated history was 100(23.4%). Kar AS conducted a study on 90 patients with surface ocular foreign bodies. Metallic corneal foreign bodies were the most common type with 48(53.3%) patients. The other particles included dust in 15 (16.7%), wood matter in 10(11.1%), insects in 5 (5.6%), glass in 7 (7.78%), and glue, gunpowder and plastic collectively made up for 5 (5.6%) of the patients. There was a strong occupational association with 49 (54.4%) patients from different industries and 10(11.1%) were domestic chore-related. Corneal foreign bodies about occupation showed that agriculture work accounted for 9 (10%) of the patients while the other occupations accounted for 8(8.88%) of the patients collectively26. Similarly, our research found that ocular foreign bodies have a strong association with the profession.
In another study conducted by Ijaz et al on 329 patients out of which 149(45.3%) had ocular surface foreign bodies in the right eye, 170(51.6%) in the left eye, and 10(3.1%) had bilateral ocular surface foreign bodies. Out of the total patients 64(19.4%) had upper tarsal foreign bodies, 220 (76.6%) had corneal foreign bodies, and the other 24 (7.4%) patients collectively had scleral, medical canthal, lower forniceal, and lower lid foreign bodies. Only 48(14.5%) of the patients had worn protective wear at their workplaces27. Patients in our study were found with a similar lack of awareness regarding protective measures with only 74(17.3%) wearing protective wear.
A study was conducted in Nepal by Shrestha T. et al. on corneal foreign bodies. According to their research, 43.33% of patients were related to some kind of metallic industry 18.33% belonged to construction work and 16.67% were farmers. The most common type of corneal foreign body was metallic28. Upon comparison, our results also had metallic corneal foreign bodies (62.1%) as the most common type found in patients.
A study done by Shah P et all on 100 patients found ocular surface foreign bodies were more common than intra-ocular foreign bodies. Ocular foreign bodies were more common in Male (80%) than female (20%). Metallic foreign bodies were found in 43% and vegetable material in 38% of cases. Cornea was the commonest site of foreign body (67%) followed by conjunctiva (22%)29. Our study showed similar results with the male gender being more commonly affected and the cornea being seen as the most common site in 290 (68%) patients.
In our study, there is a strong association found between the type of foreign body and profession. Most of the patients belong to the metallic industry (62.1%) and the most common type of foreign body was metallic which involves the peripheral cornea. The male and female ratio was observed at 6:1. The complication was observed in the corneal foreign body which varies from epithelial defect, rust ring formation, and corneal abscess formation. In our study, 82.7% did not use protective glasses. The majority of patients were not aware of the sight-threatening complication of the ocular surface of a foreign body. We counsel them about the importance of wearing protective shields during work, washing their eyes immediately after the incidents with tap water, avoiding rubbing their eyes, use of un-prescribed drugs, and the consequences of attempting the self-removal of corneal foreign bodies.
Ocular surface foreign bodies are a common occurrence in the working-class population, particularly among middle-aged men due to their professions. While these cases are generally treatable without complications, delayed clinical intervention can lead to severe vision-threatening issues. To address this, we aim to provide education on occupational hazards, raise awareness about the importance of using protective eyewear or shields, and emphasize the timely removal of foreign bodies to reduce the occurrence of ocular surface foreign bodies and related complications.
I would like to acknowledge the hospital staff and doctors for their immense contribution.
The authors have no conflict of interest.
Ethical approval was taken from the institute’s ethical committee, ERC Ziauddin University1491019MAOPH.
The consent of the patients was taken before the writing of the manuscript.
AK was the main contributor to data collection analyzing the patients and writing the manuscript. MA was a contributor to data collection. AM and MN were responsible for discussion research. FZ references and proofreading the article. AF analyzed and interpreted the patient data.
- Sharma S, Paha A. Study of the socio-demographic profile of patients presenting with ocular surface foreign bodies in a rural setting. J Med Sci Clin Res. 2018;6(11):852-857. DOI: https://dx.doi.org/10.18535/jmscr/v6i11.149
- Sharma S, EpiKhadka D, Shrestha A, Shrestha N, Suwal B, Hamal D, Shrestha R, Khatri. Epidemiological pattern of corneal foreign bodies and utilization of protective eye devices: a hospital-based cross-sectional study. Int J Occup Saf Health. 2023;13(1):87-96. doi: https://doi.org/10.3126/ijosh.v13i1.45153
- Agrawal C, Girgis S, Sethi A, Sethi V, Konale M, Lokwani P, et al. Etiological causes and epidemiological characteristics of patients with occupational corneal foreign bodies: A prospective study in a hospital-based setting in India. Indian J Ophthalmol. 2020;68(1):54-57. doi: 10.4103/ijo.IJO_623_19
- Tuladhar S, Dhakal S, Poudel S, Poudel B. Profile of Ocular Trauma in a Tertiary Centre in Western Nepal. J Gandaki Med Coll Nepal.2018;10(2):6-10. DOI:10.3126/JGMCN.V10I2.20801
- Zungu T, Mdala S, Manda C, Twabi HS, Kayange P. Characteristics and visual outcome of ocular trauma patients at Queen Elizabeth Central Hospital in Malawi. PLOS ONE. 2021;1-11. doi: 10.1371/journal.pone.0246155. e Collection 2021
- Bahoo MLA, Jamil AZ. Types of ocular surface foreign bodies and their correlation with location in the eye. Pak J Ophthalmol. 2018;34(1):25-28. DOI: https://doi.org/10.36351/pjo.v34i1.15
- Hussain A, Shaukat Q, Mahmood N. Metallic Corneal Foreign body. Prof Med J. 2019;26(4):688-691. DOI: 10.29309/TPMJ/2019.26.04.3379
- Ayyildiz T, Ozturk Y. Investigating the Factors That Affect The Frequency Of Visits Due To Corneal Foreign Bodies. Sanamed. 15(2):107-110. DOI: 10.24125/sanamed.v15i2.411
- Sun F, Zhou Y, Dong L, Qin H. Relationship between the use and type of eye protection and work-related corneal and conjunctival foreign body injuries. Inj Prev. 2021;27(6):521-526. doi: 10.1136/injuryprev-2020-043958.
- Wilson MM, Mathan JJ. Corneal foreign body and rust ring removal in a remote setting: further tips and tricks when support is afar. Emerg Crit Care Med. 2022;2(3):103-104. DOI: 10.1097/EC9.0000000000000028
- Zimmerman DR, Shneor E, Millodot M, Gordon-Shaag A. Corneal and conjunctival injury is seen in urgent care centers in Israel. Ophthalmic Physiol Opt. 2019;39(1):46-52. doi: 10.1111/opo.12600
- Sen E, Celik S, Inanc M, Elgin U, Ozyurt B, Yılmazbas P. Seasonal distribution of ocular conditions treated at the emergency room: a 1-year prospective study. Arq Bras Oftalmol. 2018;81(2):116-119. DOI: 10.5935/0004-2749.20180026
- Rosli AH, Abdurrahman MY, Kamal KM. Deeply Embedded Corneal Foreign Bodies with Fungal Keratitis Secondary to Rambutan Fruit Fall. Cureus. 2022;14(2). DOI: 10.7759/cureus.22413
- Prakash Kumar D, Kumar S, Joshi NK. An Investigation to Assess the Prevalence of Ocular Trauma in the Rural Population of Bihar Rohtas District. Eur J Mol Clin Med.8(04):2021.
- Yilmaz M, Ceylanoglu KS, Sen EM. The Effect of COVID-19 Pandemic on Eye-Related Emergency Department Visits: A Comparison of 2-Year Results. Beyoglu Eye J. 2022;7(3):223-230. doi: 10.14744/bej.2022.58966. eCollection 2022.
- Martin-Prieto S, Álvarez-Peregrina C, Thuissard-Vasallo I, Catalina-Romero C, Calvo-Bonacho E, Villa-Collar C, Sánchez-Tena MÁ. Description of the epidemiological characteristics of work-related eye injuries in Spain: a retrospective study. BMJ Open. 2020;10(10):1-7. doi: 10.1136/bmjopen-2019-035696
- Onkar, Abhishek. Commentary Tackling the corneal foreign body. Indian J Ophthalmol. 2020;68(1):57-58. DOI: 10.4103/ijo.IJO_1625_19
- Chou, HD., Chen, KJ., Kang, E.YC. et al. Eye irrigation is a first-line treatment and diagnostic method for emergency department patients who complain of ocular foreign bodies. Sci Rep. 2021;11:23386. DOI https://doi.org/10.1038/s41598-021-02989-3
- Meida NS, Setyawati I. The Influence of Corneal Foreign Body on Eye Infection. Adv Health Sci Res. 2019;15:58-60. DOI 10.2991/icosihsn-19.2019.14
- Ambikkumar A, Arthurs B, El-Hadad C. Corneal foreign bodies. Can Med Assoc J. 2022, 194 (11). doi: 10.1503/cmaj.211624.
- Agrawal S, Raj SJS, Modaboyina S, Bafna R, Gupta S, Das D. Management of impacted corneal foreign bodies: A review .2021;7(2):131-138. https://doi.org/10.18231/j.ijooo.2021.028
- Pouryahya, P., Meyer, A., Ling, Z., & Ooi, A. I Feel Something in My Eye; A Retrospective Study on the Outcome of Patients with Corneal Foreign Bodies Presenting to Emergency Department. Surg Med Open Access J. 2020;3(5):1-7. DOI:10.31031/SMOAJ.2020.03.000573
- Hoskin AK, Mackey DA, Keay L, Agrawal R, Watson S. Eye Injuries across history and the evolution of eye protection. Acta Ophthalmol. (Copenh.). 2019;97(6):637–643. https://doi.org/10.1111/aos.14086
- Rebattu B, Baillif S, Ferrete T, Risso K, Rabot A, Babeau F, Nahon-Estève S, Martel A. Corneal foreign bodies: are antiseptics and antibiotics equally effective? Eye (Lond). 2023;37(13):2664-2672. doi: 10.1038/s41433-022-02380-0.
- Bahoo MLA, Jamil AZ, Khalid MS. Ocular surface foreign body and their association with the profession. Pak J Med Health Sci. 12(2):495-498. https://www.researchgate.net/publication/327780637_Ocular_surface_foreign_bodies_and_their_association_with_profession
- Kar AS. Different Types of Corneal Foreign Bodies Post Injury and its Correlation with Specific Occupation. Int J Contemp Med Res. 2020;7(12):L1-5.
- Ijaz R, Anam A, Hameed Z, Malik IQ. Ocular surface foreign bodies: Their incidence, clinical characteristics, and demographic patterns. Pak Postgrad Med J. 2022;33(2):30-33. DOI: https://doi.org/10.51642/ppmj.v33i02.479
- Shrestha T, Parajuli S, Sharma S, Shrestha R, Singh P. Clinical Profile of Patients Presenting with Corneal Foreign Bodies: A Cross-Sectional Study Conducted in a Tertiary Hospital in Nepal. Nepal J Ophthalmol. 2022;14(27):59-64. DOI: 10.3126/nepjoph.v14i1.38010
- Shah P, Karambelkar V H. Clinical Evaluation of Ocular Foreign Bodies. Indian J Forensic Med Toxicol. 2020;14(3):550-556. DOI: https://doi.org/10.37506/ijfmt.v14i3.10423
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
