By Husson Ara1, Nasreen Naz1, Ayesha Walid1, Anila Rahim1, Sundus Aziz1
1. Dow Institute of Radiology, Dow University of Health Sciences, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/006
How to cite: Ara H, Naz N, Walid A, Rahim A, Aziz S. Evaluating Adenomyosis with Transvaginal Sonography: Diagnostic Precision and Clinical Relevance. Pak J Med Dent. 2024;13(1): 24-30. Doi: 10.36283/PJMD13-1/006
Background: Adenomyosis is an important benign gynecological condition among females with variable signs and symptoms. Prompt detection of suspicious cases is important for the effective management of the disease. The objective of the current study was to determine the frequency of adenomyosis on transvaginal ultrasound (TVS), its diagnostic accuracy, and the identification of associated factors in women with symptoms of adenomyosis.
Methods: This cross-sectional study was carried out at the radiology department of Dow University Hospital, Karachi, Pakistan from January 2022 to March 2023. All married females of reproductive age group presented with symptoms of adenomyosis for more than 7 days were included. Adenomyosis on TVS and histopathology were noted. Moreover, associated factors of adenomyosis were also studied.
Results: Of 280 patients, adenomyosis on TVS was observed in 180 (64.3%) patients whereas on histopathology in 176 (62.9%) patients. Diagnostic accuracy of adenomyosis on TVS showed that sensitivity was 89.20%, specificity 77.88%, positive predicted value 87.22%, negative predicted value 81.00%, and accuracy was found to be 85.00%. A significantly higher proportion of adenomyosis was observed among women who had infertility (p<0.001), symptoms of dysmenorrhea (p <0.001), dyspareunia (p<0.002), urinary symptoms (p <0.001), and GI symptoms (p<0.001).
Conclusion: TVS is a valuable imaging modality for identifying adenomyosis, especially in patients with clinical symptoms. Furthermore, there is a significant association between adenomyosis and various clinical symptoms, including infertility, dysmenorrhea, dyspareunia, urinary symptoms, and gastrointestinal symptoms.
Keywords: Adenomyosis, Ultrasonography, Histopathology
Adenomyosis is a common medical ailment of gynecology that occurs when endometrial tissue grows abnormally in the myometrium of the uterus. Adenomyosis occurs when the normal boundary between the endometrial basal layer and the myometrium is disrupted 1-3. The cause of this disruption is not fully understood but may be due to uterine trauma, pregnancy, postpartum endometritis, or cesarean delivery. The initial histopathological finding of this pathology was referred to as osteosarcoma adenoids uterinum4. However, most of the patients with adenomyosis are asymptomatic. It is reported that painful menstruation, heavy vaginal bleeding during menstruation, and pelvic pain are the common presenting symptoms5. Pelvic tenderness is elicited on examination. Recent data suggest the prevalence of adenomyosis is around 10%-31%6,7. According to another study, adenomyosis is found in 20.9% of patients8. In the Pakistani population, adenomyosis is found in 68.3% of the patients9. A theory of altered lymphatic pathway has been proposed for adenomyosis development 10.
Ultrasound, hysterosalpingography and magnetic resonance imaging (MRI) are the common modalities usually used for evaluation of adenomyosis. Hysterosalpingography is a minimally invasive technique for diagnosis but carries the risk of radiation exposure11. Transvaginal ultrasound (TVS) is the preferred initial imaging investigation. It is cheap, non-invasive without ionizing radiation, and readily available modality12. MRI is the modality without ionizing radiation and its excellent spatial resolution and soft tissue contrast make it useful for adenomyosis evaluation. However, it is an expensive modality and not readily available.
The rationale of the study is that adenomyosis is an important benign gynecological condition among females. Menorrhagia as a result of adenomyosis can cause significant blood loss which may lead to anemia and significant morbidity. Moreover, dysmenorrhea and chronic pelvic pain are other presenting symptoms that may impair the quality of life in women13. Therefore, it is important to diagnose it early so that prompt management can be initiated. This study evaluated the frequency, diagnostic precision, and clinical relevance of adenomyosis using TVS. Moreover, it also revealed the most frequent radiological features of adenomyosis on TVS and its association with the patient’s clinical symptoms.
This cross-sectional study was carried out at the radiology department of Dow University Hospital, Ojha campus Karachi, Pakistan from January 2022 to March 2023. Ethical approval was obtained from the Institutional Review Board of Dow University of Health Sciences prior commencement of the study (IRB #: IRB-2323/DUHS/Approval/2021/659). Moreover, signed informed consent was also obtained from all study participants before the enrolment in the study. All married females of reproductive age group between 18-50 years presented with symptoms of adenomyosis for more than 7 days were included. Patients already diagnosed with adenomyosis and presented with follow-up after treatment, diagnosed cases of uterine fibroids, and already diagnosed cases of pelvic inflammatory disease were excluded.
Patients’ records were evaluated for the diagnosis of adenomyosis determined by hysterectomy and for sonography performed within 2 months of surgery. Sonograms were evaluated by radiologists without knowledge of the extent of adenomyosis. Sonographic categories included visualization of the endometrium, presence of a diffuse uterine process, presence of fibroids, and normal findings. Pathologic results included mild, focal, and severe adenomyosis.
Epi Info sample size calculator was used and the estimated sample size was 280. Clinically suspected adenomyosis was defined as based on the presence of menorrhagia (any episode of bleeding during the menstrual cycle lasting for more than 7 days) or dysmenorrhea (any episode of painful menstruation of any intensity during the menstrual cycle) or pelvic pain (Visual analog Scale VAS score 4-10).
Adenomyosis on TVS was labeled as positive based on the presence of any one of the following characteristics: Globular uterus (rounded configuration of uterus) asymmetrical anteroposterior myometrial wall or indistinct endometrial myometrial interface (poor differentiation of endometrial myometrial interface) or myometrial cysts or hyperechoic linear striations or heterogeneous appearance of myometrium. On histopathology, adenomyosis was defined as the presence of endometrial glands and endometrial stroma within the myometrium of the uterus. This information along with baseline characteristics such as age, parity, infertility, and previous in-vitro fertilization (IVF) were noted along with symptoms such as dysmenorrhea, dyspareunia, urinary symptoms, or gastrointestinal (GI) symptoms. Additionally, sonographic characteristics such as rounded Globular configuration of the uterus, asymmetry of the anteroposterior wall of the myometrium, poor definition of the endometrial-myometrial junction, myometrial cysts, sub-endometrial linear echogenic striations, heterogeneous myometrium, and asymmetrical thickening was observed.
SPSS version 24 was used for statistical analysis. Mean standard deviation (SD) was reported for quantitative variables whereas frequency and percentages were calculated for qualitative variables. Independent t-test and chi-square test were applied to see the mean difference and association of adenomyosis with baseline characteristics. The p-value of ≤0.05 was considered significant. Additionally, the diagnostic accuracy of TVS in diagnosing adenomyosis was assessed by calculating sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) using contingency tables taking histopathology findings as the gold standard.
Of 280 patients, the mean age of the patients was 44.51 ±13.16 years. There were 172 (61.4%) parous women whereas previous cesarean section was observed in 141 (50.4%) patients. In addition, infertility was observed in 172 (61.4%) and previous IVF was observed in 107 (38.2%) patients. Dysmenorrhea was the most common symptom observed in 237 (84.6%) patients followed by dyspareunia in 192 (68.6%), urinary symptoms in 182 (65.0%), whereas GI symptoms were observed in 179 (63.9%) patients.
Ultrasonographic findings showed that a rounded Globular configuration of the uterus was observed in 116 (41.4%) patients, asymmetry of the anteroposterior wall of myometrium in 99 (35.4%), poor definition of endometrial-myometrial junction in 115 (41.1%), myometrial cysts in 127 (45.4%), sub endometrial linear echogenic striations in 93 (33.2%), heterogeneous myometrium in 138 (49.3%), and asymmetrical thickening in 90 (32.1%) patients. Adenomyosis on TVS was observed in 180 (64.3%) patients whereas on histopathology in 176 (62.9%) patients (Figure 1).
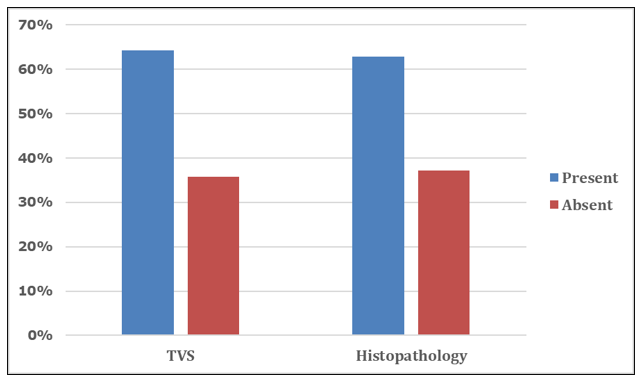
Figure 1: Frequency of adenomyosis on TVS and histopathology (n=280)
The comparison of adenomyosis on TVS with baseline characteristics is shown in detail in Table 2. A significantly higher association of adenomyosis was found among women who had infertility (p <0.001), history of PID (p-value <0.001), endometriosis (p-value <0.001), had symptoms of dysmenorrhea (p <0.001), dyspareunia (p 0.002), urinary symptoms (p <0.001), and GI symptoms (p <0.001). Similarly, significant associations of adenomyosis on histopathology were observed with infertility (p-value <0.001), history of PID (p-value <0.001), endometriosis (p-value <0.001), dysmenorrhea (p-value <0.001), dyspareunia (p-value <0.001), urinary symptoms (p-value <0.001), and GI symptoms (p-value <0.001) (Table 1).
Table 1: Comparison of baseline characteristics with adenomyosis findings on TVS and histopathology (n=280)
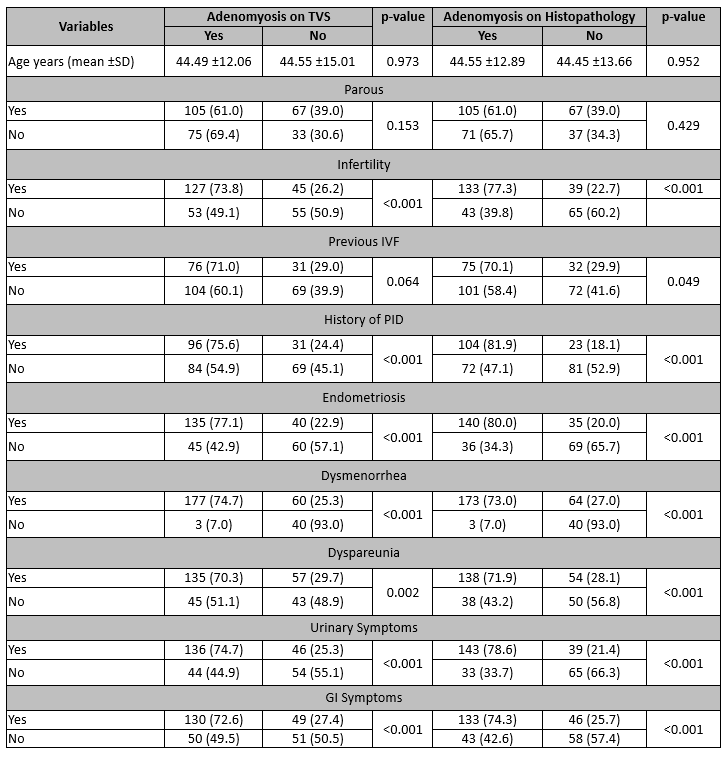
CS: Cesarean Section, IVF: In Vitro Fertilization, GI: Gastrointestinal, TVS: Transvaginal Ultrasound. Independent t-test applied, Chi-Square test applied, p-value ≤0.05 considered as significant.
Diagnostic accuracy of adenomyosis on TVS taking histopathology as the gold standard showed that sensitivity was found to be 89.20%, specificity 77.88%, PPV 87.22%, NPV 81.00%, and overall diagnostic accuracy was found to be 85.00% (Table 2).
Table 2: Diagnostic accuracy of adenomyosis on TVS with histopathology (n=280)
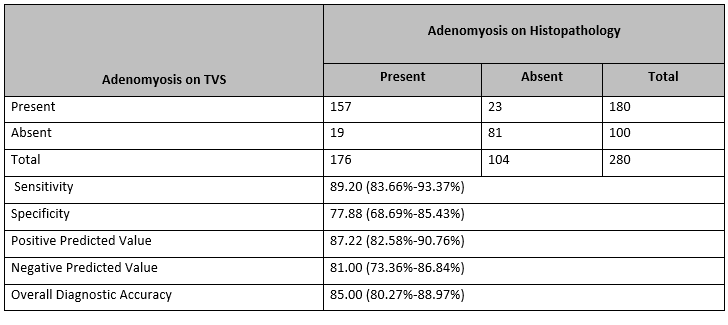
TVS: Transvaginal Ultrasound
Sonography has emerged as a primary preferred and valuable tool in the diagnostic workup of adenomyosis due to its non-invasive nature and widespread availability. The findings of the study revealed that the sensitivity of TVS in detecting adenomyosis was found to be 89.20%, specificity 77.88%, PPV 87.22%, NPV 81.00%, and overall diagnostic accuracy 85.00%. These values suggest that sonography can be a reliable tool for evaluating adenomyosis, with a relatively high sensitivity for ruling out the condition and a respectable specificity for confirming its presence. This finding is consistent with previous studies that have also reported somewhat similar diagnostic accuracy parameters14-16. A recent international study by Maudot et al has reported moderate sensitivity as compared to the current study findings. According to their study findings, sensitivity was found to be 52%, specificity 85%, PPV 77%, and NPV 86%17. The author emphasized that within the field of gynecology, TVS stands out as the most frequently employed non-invasive diagnostic procedure. Furthermore, it is the initial and preferred diagnostic method for adenomyosis due to its widespread acceptance and cost-effectiveness, despite its moderate diagnostic accuracy. In a systematic review and meta-analysis carried out by Liu et al, it was noted that the diagnostic performance of TVS was found to be high and comparable to the performance of MRI18.
Our study yielded valuable insights into the frequency of adenomyosis detection using sonography. The overall frequency of adenomyosis in the studied population was found to be 64.3%. This finding is somewhat consistent with previous research suggesting that adenomyosis is a prevalent condition among women of reproductive age, although the reported prevalence can vary significantly across different populations17,19.
Furthermore, our study explored the relationship between patient clinical demographics and adenomyosis detection. We observed that patients presented with infertility, endometriosis, pelvic inflammatory disease dysmenorrhea, dyspareunia, and urinary and GI symptoms were found to have a significantly higher likelihood of adenomyosis. This observation aligns with existing literature suggesting that adenomyosis may be more common in specific subgroups of the population, providing important clinical context for identifying at-risk individuals20-22.
Among features of TVS, sub-endometrial linear striations were found to be the most specific feature for adenomyosis in a previous study15. Moreover, the enlarged globular uterus had high accuracy for adenomyosis diagnosis. There may be focal or diffuse thickening of the uterine myometrium with indistinct endometrial myometrial and heterogeneous appearing uterine myometrium. This appearance has been described as Venetian blind shadowing23. In the current study, heterogeneous myometrium, and myometrial cysts were found to be the most frequent features along with a poor definition of the junctional zone between endometrium and myometrium with associated globular uterine enlargement. First and foremost, our findings emphasize the importance of considering adenomyosis as a potential diagnosis in women presenting with symptoms such as dysmenorrhea and pelvic pain, especially in those who fall within the identified at-risk demographic groups. Healthcare providers should be aware of the utility of sonography as a non-invasive and accessible diagnostic tool for adenomyosis.
Furthermore, the diagnostic accuracy parameters we reported highlight the value of sonography in the initial assessment of adenomyosis. This imaging modality can aid in triaging patients for further evaluation and treatment planning. It has been reported in the literature that the widespread availability of ultrasound and the rising expenses associated with MRI have resulted in TVS being favored as the primary imaging modality for initial assessments, with MRI being reserved for non-invasive diagnosis where the diagnosis is uncertain or ambiguous17,24,25. However, it is essential to recognize that sonography, while valuable, may not be the definitive diagnostic tool in all cases. In instances where clinical suspicion remains high despite negative sonographic findings, additional imaging modalities or invasive procedures may be warranted.
One key limitation is the relatively small sample size inherent to a single-center study. Larger, multi-center studies with more diverse patient populations are needed to provide more robust estimates of sonography’s diagnostic accuracy in detecting adenomyosis. Second, the diagnostic criteria used in sonography for adenomyosis may not be standardized across all institutions and radiologists. Variations in the interpretation of sonographic findings, such as uterine wall thickness and myometrial cysts, could impact diagnostic accuracy.
TVS in the evaluation of adenomyosis is an important reliable diagnostic tool. The most reliable sonographic finding is the presence of sub-endometrial linear striation with other features that support the diagnosis of adenomyosis including heterogenous myometrium, myometrial cysts, and globular configuration of the uterus. A considerably higher number of patients with clinical features of infertility, endometriosis, pelvic inflammatory disease, dysmenorrhea, dyspareunia, and urinary and GI symptoms were found to have a higher prevalence of adenomyosis on TVS and detected positive on histopathology.
We are grateful to Prof Dr Nasreen Naz for her support and guidance.
There was no conflict of interest among the authors.
Ethical approval was obtained from the Institutional Review Board of Dow University of Health Sciences for the study (IRB #: IRB-2323/DUHS/Approval/2021/659).
Signed informed consent was obtained from all study participants before the enrolment in the study.
HA, NN, AW conception and design of the study. HAM AW, AR data acquisition and analysis. HA, SA drafting of the manuscript. NN, AW critical review of the manuscript. All authors approved the final version of the manuscript.
- Kobayashi H, Kishi Y, Matsubara S. Mechanisms Underlying Adenomyosis-Related Fibrogenesis. Gynecol Obstet Invest. 2020;85(1):1-12. doi: 10.1159/000502822.
- Stratopoulou CA, Donnez J, Dolmans MM. Origin and Pathogenic Mechanisms of Uterine Adenomyosis: What Is Known So Far. Reprod Sci. 2021;28(8):2087-2097. doi: 10.1007/s43032-020-00361-w.
- Chapron C, Vannuccini S, Santulli P, Abrão MS, Carmona F, Fraser IS, et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum Reprod Update. 2020 ;26(3):392-411. doi: 10.1093/humupd/dmz049.
- Antero MF, Ayhan A, Segars J, Shih IM. Pathology and Pathogenesis of Adenomyosis. Semin Reprod Med. 2020;38(2-03):108-118. doi: 10.1055/s-0040-1718922.
- Loring M, Chen TY, Isaacson KB. A Systematic Review of Adenomyosis: It Is Time to Reassess What We Thought We Knew about the Disease. J Minim Invasive Gynecol. 2021;28(3):644-655. doi: 10.1016/j.jmig.2020.10.012.
- Mishra I, Melo P, Easter C, Sephton V, Dhillon-Smith R, Coomarasamy A. Prevalence of adenomyosis in women with subfertility: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2023;62(1):23-41. doi: 10.1002/uog.26159.
- Mousa M, Al-Jefout M, Alsafar H, Kirtley S, Lindgren CM, Missmer SA, Becker CM, Zondervan KT, Rahmioglu N. Prevalence of Common Gynecological Conditions in the Middle East: Systematic Review and Meta-Analysis. Front Reprod Health. 2021;3:661360. doi: 10.3389/frph.2021.661360.
- Naftalin J, Hoo W, Pateman K, Mavrelos D, Holland T, Jurkovic D. How common is adenomyosis? A prospective study of prevalence using transvaginal ultrasound in a gynecology clinic. Hum Reprod. 2012;27(12):3432-3439. doi: 10.1093/humrep/des332.
- Rubab S, Maqsood A, Rafique MS, Kundi S, Yasin A, Tariq T. Comparing Accuracies of Transvaginal Ultrasonography and Magnetic Resonance Imaging for Nonsurgical Diagnosis of Adenomyosis. J Soc Obstet Gynaecol Pak. 2022;12(3):225-229.
- Zhai J, Vannuccini S, Petraglia F, Giudice LC. Adenomyosis: Mechanisms and Pathogenesis. Semin Reprod Med. 2020;38(2-03):129-143. doi: 10.1055/s-0040-1716687.
- Kilcoyne A, O’Shea A, Gervais DA, Lee SI. Hysterosalpingography in endometriosis: performance and interpretation. Abdom Radiol (NY). 2020;45(6):1680-1693. doi: 10.1007/s00261-019-02373-w.
- Cunningham RK, Horrow MM, Smith RJ, Springer J. Adenomyosis: A Sonographic Diagnosis. Radiographics. 2018;38(5):1576-1589. doi: 10.1148/rg.2018180080
- Nelsen LM, Lenderking WR, Pokrzywinski R, Balantac Z, Black L, Pokras S, et al. Experience of Symptoms and Disease Impact in Patients with Adenomyosis. Patient. 2018;11(3):319-328. doi: 10.1007/s40271-017-0284-2.
- Hussein NA, El Refaey MH. Evaluation of transvaginal ultrasound role in the prediction of adenomyosis: correlation with histopathology. Int J Reproduction, Contraception, Obstetrics Gynecol. 2021;10(8):2987-2993. doi: 10.18203/2320-1770.ijrcog20212945
- Kepkep K, Tuncay YA, Goynumer G, Tutal E. Transvaginal sonography in the diagnosis of Adenomyosis: Which findings are most accurate? Ultrasound Obstet Gynecol. 2007;30:341–345. doi: 10.1002/uog.3985.
- Shaikh A, Masroor I, Masood A, Saeed SA. Diagnostic Accuracy of Transvaginal Ultrasound in Adenomyosis Taking MRI as a Gold Standard. J Coll Physicians Surg Pak. 2023;33(10):1118-1123. doi: 10.29271/jcpsp.2023.10.1118.
- Maudot C, Vernet T, Debras E, Fernandez H, Capmas P. Diagnostic accuracy study of sonography in adenomyosis: A study of current practice. J Gynecol Obstet Hum Reprod. 2023;52(7):102604. doi: 10.1016/j.jogoh.2023.102604.
- Liu L, Li W, Leonardi M, Condous G, Da Silva Costa F, Mol BW, Wong L. Diagnostic Accuracy of Transvaginal Ultrasound and Magnetic Resonance Imaging for Adenomyosis: Systematic Review and Meta-Analysis and Review of Sonographic Diagnostic Criteria. J Ultrasound Med. 2021;40(11):2289-2306. doi: 10.1002/jum.15635.
- Tariq M, Anwar J, Amin N, Gul B, Niaz A, Nawaz KH. Diagnostic Accuracy of Ultrasound and MRI for Diagnosis of Adenomyosis Taking Histopathology as Gold Standard. Pak Armed Forces Med J. 2022;72. 10.51253/pafmj.v72iSUPPL-2.8064
- Eisenberg VH, Arbib N, Schiff E, Goldenberg M, Seidman DS, Soriano D. Sonographic Signs of Adenomyosis Are Prevalent in Women Undergoing Surgery for Endometriosis and May Suggest a Higher Risk of Infertility. Biomed Res Int. 2017; 2017:8967803. doi: 10.1155/2017/8967803.
- Orlov S, Jokubkiene L. Prevalence of endometriosis and adenomyosis at transvaginal ultrasound examination in symptomatic women. Acta Obstet Gynecol Scand. 2022;101(5):524-531. doi: 10.1111/aogs.14337.
- Isaacson K, Loring M. Symptoms of Adenomyosis and Overlapping Diseases. Semin Reprod Med. 2020;38(2-03):144-150. doi: 10.1055/s-0040-1721795.
- Chin LHQ, Li YL, Lee KH. Venetian blind shadowing on ultrasound. Abdom Radiol (NY). 2019;44(2):796-797. doi: 10.1007/s00261-018-1739-1.
- Cunningham RK, Horrow MM, Smith RJ, Springer J. Adenomyosis: A Sonographic Diagnosis. Radiographics. 2018;38(5):1576-1589. doi: 10.1148/rg.2018180080.
- Alcázar JL, Vara J, Usandizaga C, Ajossa S, Pascual MÁ, Guerriero S. Transvaginal ultrasound versus magnetic resonance imaging for diagnosing adenomyosis: A systematic review and head-to-head meta-analysis. Int J Gynaecol Obstet. 2023;161(2):397-405. doi: 10.1002/ijgo.14609.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
