By Muhammad Mohsin Haider1, Kulsoom Fatima Rizvi1, Lubna Khan1, Sidra Arshad1, Misbah Rahman2, Maria Moin1, Niha Ahmed1
- Community Dentistry Department, Bahria University Dental College, Bahria University Health Sciences, Karachi, Pakistan
- Islamic International Dental College and Hospital IIDC, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/011
How to cite: Haider MM, Rizvi KF, Khan L, Arshad S, Rahman M, Moin M, Ahmed N. Dental Care Evaluation Among Children with Cerebral Palsy: A Special School Survey in Karachi. Pak J Med Dent. 2024;13(1): 57-63. Doi: 10.36283/PJMD13-1/011
Background: Children with Cerebral Palsy (CP) face malfunctioning in the motor system and go through difficulties in hearing, eating, sight, and musculoskeletal systems and are also mentally impaired. This may render them unable to maintain proper oral hygiene. The objective of this study was to evaluate oral hygiene in children with cerebral palsy in Karachi’s special schools.
Methods: A cross-sectional study with a total of 80 CP children was conducted in special schools in Karachi using a purposive sampling technique. CP children aged 12-15, who consented via guardians/school and were able to comply with the procedure were included. CP children on medications or systemic diseases were excluded. Proforma containing demographic details, and dental history questions were asked. Oral examination was done using the Plaque index, Gingival index, and Oral hygiene index simplified was observed.
Results: In this study, there were 48 (60%) males and 32 (40%) females. The mean ± SD of age was 14.4 ±1.4. Independent t-test showed that there was a significant association of gingival index means with the institutes selected (p=0.004). The other parameters PI and OHIS did not show any association. Mean PI (mean 1.99, SD 0.62) and GI (mean 1.9, SD 0.60) showed moderate plaque and gingival inflammation and poor oral hygiene index (mean 3.31, SD 1.3). ANOVA showed associations of PI, GI & and OHIS with dental habits.
Conclusion: CP children have poor oral hygiene status and therefore need early diagnosis and prompt treatment to prevent complications.
Keywords: Cerebral Palsy, Periodontitis, Oral Hygiene Index.
Children with CP suffer from a group of movement and posture disorders. They also have problems with sensing the stimulus and its comprehension and communication1. The global prevalence of CP is 2 to 2.5 per 1000 live births2. Children with CP may have uncontrolled salivation, difficulty chewing and swallowing, respiratory issues, and poor oral hygiene. The studies reveal that oral health is one of the most common underlying factors for most of the complications3. Throughout their lifetime, people with Special Health‑Care Needs (SHCN) can be at more risk for oral diseases 4. Different studies show that the major cause of bad oral health in CP children is either deficient or complete lack of body and brain harmony. Due to the lack of this harmony, these children cannot perform their oral hygiene practices normally and their oral health is affected2,5,6. Among other oral diseases, dental caries and periodontal diseases are more common and the risk of these diseases is directly proportional to the severity of neuromuscular disorders7.
Research shows that children affected by CP depict a higher frequency of gingival hyperplasia & and related bleeding8,9. This can be due to the simple reason that children with CP are not able to maintain their oral hygiene daily due to hypersensitive oral mucosa and lack of manual dexterity to clean oral cavities10,11. Medicines that are used to prevent seizures such as DPH, sodium valproate, and phenobarbital, are also cause of gingival overgrowth and other diseases of periodontium9-11.
All these factors can be involved in biofilm formation in teeth. In addition, spastic quadriplegic CP & choro athetoid CP make patients handicapped because of involuntary, constant head movements & maintenance of a good oral environment becomes next to impossible. There is little data available in Pakistan that investigates the association between Cerebral Palsy and oral hygiene status. Evaluation of the correlation between changes in body composition and periodontal disease progression is essential to control the disease in the initial stages. Therefore, the objective of this study was to evaluate oral hygiene in children with cerebral palsy in Karachi’s special schools using indices of plaque, gingival health, and oral hygiene.
A cross-sectional study was conducted in special schools in Karachi using a purposive sampling technique. The sample size was calculated using the mean and SD difference of significant outcome variable age, Probing pocket depth (PPD), Clinical Attachment Level (CAL), and Oral Hygiene Index Simplified (OHI-S) in the Cerebral palsy group (6 ± 1.871) keeping the Confidence interval 95% and power 80%, the sample size per was calculated as 58 which we raised it to 80 as per convenience12.
The study population was children with CP which included the age range 12-15, who were mentally stable, able to comply with the examination, and had written informed consent from the parents and caregivers. Excluded were children who had vision & and hearing impairments, were on antibiotics, antiepileptics, or other medications used within 3 months, underlying systemic diseases, and underwent dental treatment within the last 6 months. The study instrument used was a self-designed proforma which consisted of demographic details, medical and dental history, and lastly examination i.e., Plaque index, gingival index, and oral hygiene index. For examination of the oral cavity the use of dental mirrors and CPI probe after seating the patient on a normal chair with appropriate light. The examination of all the CP children was done by a senior dentist from the Department of Community Dentistry.
Data was analyzed using SPSS Version 20. The normality of data was determined by applying the Kolmogorov–Smirnov test and the Shapiro–Wilk test. Descriptive statistics were used. A T-test was used for continuous variables. ANOVA test was used to compare means between groups.
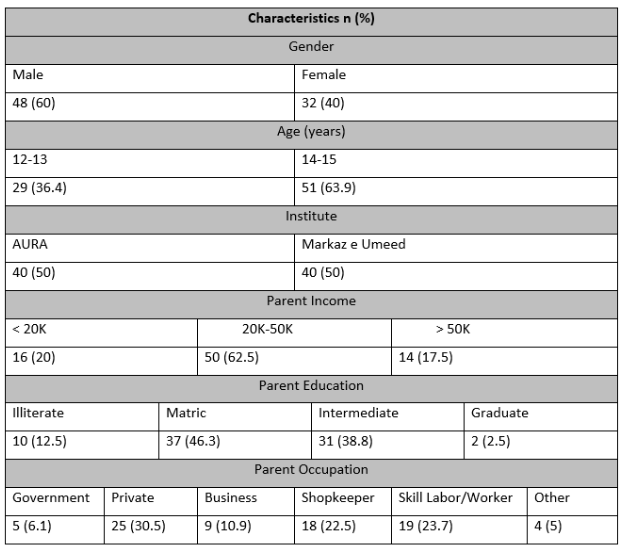
The given data is based on a sample size of 80 individuals, and the percentages for each variable have been provided. The gender distribution shows that 60% of the sample size was male, while the remaining 40% was female. In terms of age, 36.4% of the sample size fell in the age range of 12-14 years, and 63.9% fell in the age range of 15-18 years. Regarding parent education, 12.5% of the sample size had illiterate parents, while 46.3%, 38.8%, and 2.5% had parents with Matric-Intermediate, graduate, and post-graduate education, respectively. The parent occupation data shows that 6.1% of the sample size had parents in other occupations, while 30.5%, 10.9%, 22.5%, 23.7%, and 5% had parents in Skill Labor/Worker, Government, Private, Business, and Shopkeeper occupations, respectively. In terms of parent income, 20% of the sample size had a parent income of less than 20K, 62.5% had a parent income ranging from 20K to 50K, and 17.5% had a parent income greater than 50K. Finally, the data shows that 50% of the sample size was from AURA, while the remaining 50% was from Markaz e Umeed.
Table 1: Demographic details of the participants.
The above data pertains to a sample population of n = 80 and presents various variables related to dental health. The brushing dependency variable indicates that 34% of individuals brush their teeth independently, while 46% do so with assistance. Brushing frequency shows that 60% brush their teeth once a day, while 20% brush twice a day. The brushing duration variable is divided into three categories, where 29% brush for less than a minute, 34% brush for 1-2 minutes, and 17% brush for more than 2 minutes. The dental visit variable indicates that 31% have never visited a dentist, while 16% visit less than every 6 months and 33% visit more than every 6 months. In terms of treatments offered, 72% have not received any treatment, while only 2%, 1%, and 5% have undergone scaling, restorative procedures, and extraction, respectively. Use of antibiotics is reported by only 2% of individuals, while 76% do not use antibiotics at all. Finally, the variable on any systemic disease indicates that 66% do not have any disease, while 10%, 3%, and 1% have CNS, urogenital, and asthma-related diseases, respectively.
Table 2: Dental and medical history of the participants.
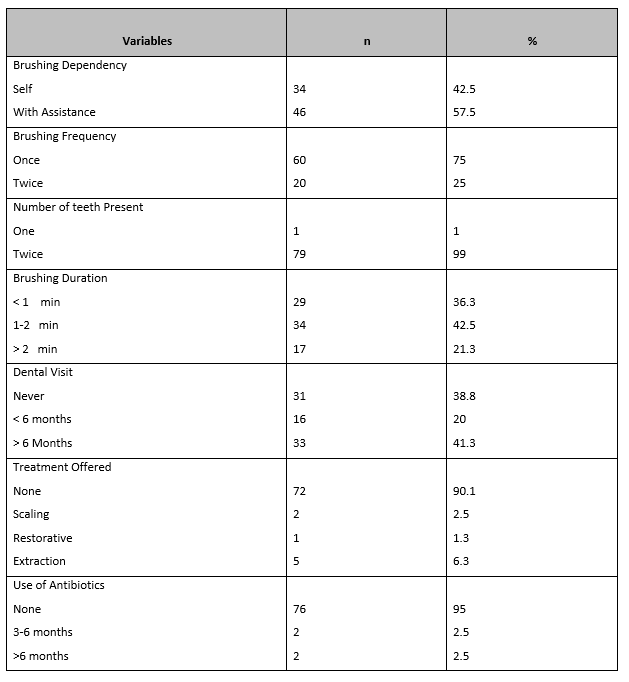
Table 3: Association of clinical dental parameters with CP.
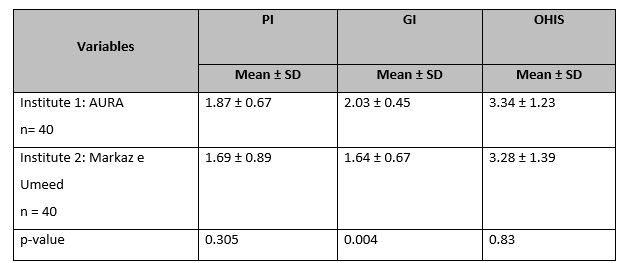
p-value <0.05 is considered significant.
Independent t-test showed that there was a significant association of gingival index means with the institutes selected (p=0.004). The other parameters PI and OHIS did not show any association. Table 3
Table 4: Association of demographics, medical, and dental variables with PI, GI, and OHI.
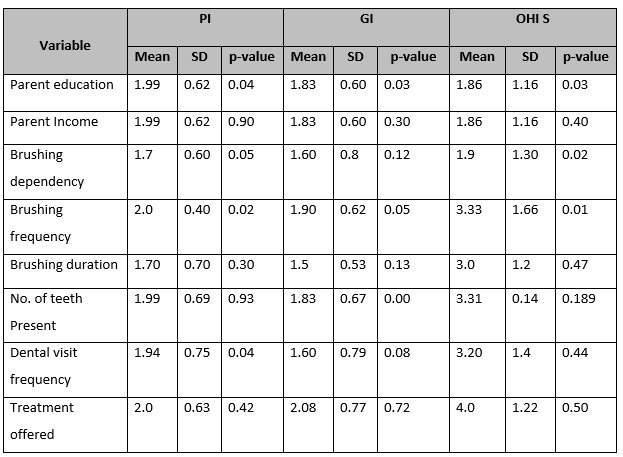
p-value <0.05 is considered significant.
ANOVA and independent t-test showed that all three clinical parameters i.e., PI, GI, and OHIS were significantly associated with parent education and brushing frequency respectively. However, only PI and OHIS were found to be significantly associated with brushing dependency (t-test). GI was significantly associated with the number of teeth present (t-test) and PI was associated with dental visit frequency (ANOVA). Table 4
Figure 1 shows a bar graph with means of PI, GI, and OHI at different levels. Both the PI and GI means are at the moderate stage while the OHI mean shows a poor category.
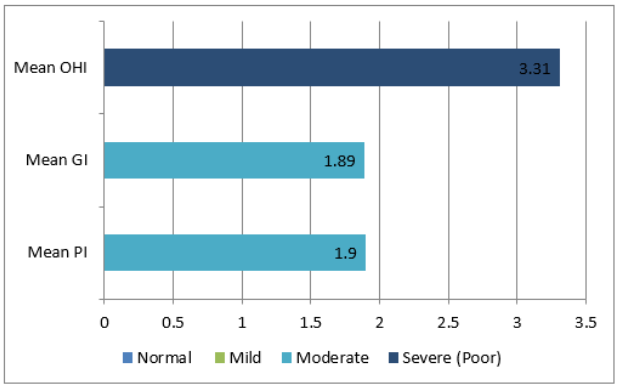
Figure 1: Clinical interpretation of the dental parameters.
This Cross-Sectional Analytical study offered a chance to evaluate the oral health issues among kids with CP in particular schools in Karachi, an area that has never been examined. A sample size of 80 individuals was identified from 2 centers of AURA and Markaz e Umeed. Although time-consuming and resource-intensive, this allowed for the collection of a sizable and representative sample. The sample size ranged from (12 to 15) years old, with 60% men and 40% women. The current study was approved by the Ethical Review Committee (ERC) of Bahria University Health Sciences and met all inclusion and exclusion criteria.
To provide an accurate depiction of the oral wellness condition of CP children, a wide range of oral health parameters were taken into account during the oral health assessment, including periodontal index, gingival index, and oral health index. Children with CP performed similarly to other children without CP control group in terms of PI and OHIS, adverse in terms of gingival health. Children with CP frequently have periodontal conditions as a result of insufficient oral hygiene. Several investigations have shown that periodontal hyperplasia and associated bleeding are more common in children with CP. The primary contributing factors are difficulties with daily oral hygiene, intraoral sensitiveness, orofacial motor disorders, malocclusion, and physical capacities13. A significant additional factor is the usage of antiepileptic drugs, notably phenytoin. Children with CP have worse gingival health than children from control groups as documented in numerous literature14. Furthermore, current research revealed similar variations related to gingival health.
As the present data elaborates, the (brushing dependency variable) indicates that 34% of individuals brush their teeth independently, while 46% do so with assistance. This is due to children’s weak control of the neuromuscular region, which prevents them from establishing prime oral hygiene, older children in particular. Furthermore, the usage of anticonvulsive effects, which may cause periodontal hyperplasia, is most likely a contributing element to the CP group’s higher prevalence of gingival hyperplasia15.
Many investigations have shown that gum hyperplasia and associated bleeding are more common in children with CP5. The same causes that lead to dental caries and biofilm accumulation may be responsible for this high incidence. The main contributing factors include difficulties with performing routine, intraoral sensitivity, Orofacial motor dysfunction, and oral hygiene16. Gingival hyperplasia predicts that another significant cause of periodontal problems is the use of antiepileptic drugs, particularly phenytoin17.
Another study reveals as children get older, with spastic quadriplegic CP mostly face difficulties regarding oral hygiene. Due to the difficulty of maintaining proper dental hygiene due to the uncontrollable head movements that occur continuously, choreoathetoid CP may also be linked to periodontal disease18. Moreover, only PI and OHIS were found to be significantly associated with brushing reliance in the current study, while PI was connected with the frequency of dental visits.
Low income and poor dental health are connected, according to surveys19. Therefore, it is assumed that socioeconomic issues will likewise have an impact on the quality of life. The present study also depicted parent income, with 20% earning less than 20K, 62.5% of parent income ranging from 20K-50K, and 17.5% of parents earning 50K and established a highly significant link between poor family income and a detrimental effect on CP children’s oral health-related quality of life (OHRQoL). According to De Camargo and Antunes et al., investigations of a few socioeconomic elements in CP youngsters. They demonstrated a connection between increased levels of unidentified dental decays and the requirement for oral care and a poor family income20. These patients may have poorer OHRQoL and may suffer as a result of this fact. Therefore, it is crucial to evaluate these disorders as a whole when discussing oral health and OHRQoL in patients receiving special treatment. An additional study by Akhter, Rahena, et al. showed the link between dental health and quality of life using questionnaires which concluded that children with CP had considerably lower OH-QoL than children who were normally developing21.
The findings of the current study demonstrated that parents of children with cerebral palsy need more instruction on how to maintain their children’s oral hygiene and how to effectively clean their teeth with an electric toothbrush because parental education and brushing frequency were significantly correlated with three clinical indicators, including PI, GI, and OHIS. Programs for parents having children with disabilities in oral health care have also been advocated by other studies22-23.
The study had some limitations. Due to accessibility constraints, not all of the city’s CP clinics could be included in this study. Another potential weakness of the study is that the questionnaires were filled out by parents, which may not accurately reflect the children’s situations and feelings. The authors suggest that the relationship between cerebral palsy and dental decays of the deciduous teeth, periodontal condition, Angle’s Class II malocclusion, and anterior open bite in CP children needs further study. To more clearly identify the relationship between tooth damage and cerebral palsy, more research is needed. From an early age, cerebral palsy patients should be continuously monitored to promptly identify and treat any oral lesions.
Periodontal disease severity, communication skills severity, and low family income are all factors that have a detrimental effect on children with CP. To better understand the effects of diseases and socioeconomic variables on patients’ lives and to design appropriate therapies based on the characteristics of each population, it is crucial to evaluate OHRQoL in all patient groups.
None
The authors declare no conflict of interest.
Ethical approval of the study was obtained from the ethical review committee of the institute.
Informed consent was taken before obtaining the data.
All authors contributed equally to the manuscript.
- Cardoso AM, Gomes LN, Silva CRD, de SC Soares R, De Abreu MHN, Padilha WW, et al. Dental caries and periodontal disease in Brazilian children and adolescents with cerebral palsy. International journal of environmental research and public health. 2015;12(1):335-353. doi: 10.3390/ijerph120100335
- Abanto J, Carvalho TS, Bönecker M, Ortega AO, Ciamponi AL, Raggio DP. Parental reports of the oral health-related quality of life of children with cerebral palsy. BMC Oral Health. 2012;12(1):1-8. https://doi.org/10.1186/1472-6831-12-15
- Akhter R, Hassan NMM, Nadkarni M, Martin EF, Khandaker G. Oral health in children with cerebral palsy. Cerebral Palsy-Clinical and Therapeutic Aspects: IntechOpen; 2018. https://doi.org/10.5772/intechopen.79452
- Wasnik M, Chandak S, Kumar S, George M, Gahold N, Bhattad D. Dental management of children with cerebral palsy-a review. Journal of Oral Research & Review. 2020;12(1). DOI: 10.4103/jorr.jorr_19_19
- El Ashiry EA, Alaki SM, Nouri SM. Oral health quality of life in children with cerebral palsy: parental perceptions. Journal of Clinical Pediatric Dentistry. 2016;40(5):375-387. https://doi.org/10.17796/1053-4628-40.5.375
- Ciamponi A. Dental caries prevalence in the primary dentition of cerebral-palsied children. The Journal of Clinical Pediatric Dentistry. 2003;27(3):287-292.
- MEGGIORIN F. Paralisi cerebrale infantile in età pediatrica (0-16 anni): l’igiene dentale. https://hdl.handle.net/20.500.12608/38094
- Du RY, McGrath C, Yiu CK, King NM. Oral health in preschool children with cerebral palsy: a case–control community‐based study. International Journal of Paediatric Dentistry. 2010;20(5):330-335.https://doi.org/10.1111/j.1365-263X.2010.01062.x
- Guare RdO, Ciampioni AL. Prevalence of periodontal disease in the primary dentition of children with cerebral palsy. Journal of dentistry for children. 2004;71(1):27-32.
- Guerreiro PO, Garcias Gd. Oral health conditions diagnostic in cerebral palsy individuals of Pelotas, Rio Grande do Sul State, Brazil. Ciência & Saúde Coletiva. 2009;14(5):1939. DOI:10.1590/S1413-81232009000500036
- de Carvalho RB, Mendes RF, Prado Jr RR, Neto JMM. Oral health and oral motor function in children with cerebral palsy. Special Care in Dentistry. 2011;31(2):58-62. https://doi.org/10.1111/j.1754-4505.2011.00180.x
- Mohammed SR, Anand N, Chandrasekaran S, Mahalakshmi K, Padmavathy K. Evaluation of periodontal status and detection of Dialister pneumosintes in cerebral palsy individuals: A Case–Control study. Indian Journal of Dental Research. 2018;29(6):768. DOI: 10.4103/ijdr.IJDR_582_15
- UK NGA. Cerebral palsy in under 25s: assessment and management. 2017. PMID: 28151611 Bookshelf ID: NBK419326
- Jan BM, Jan MM. Dental health of children with cerebral palsy. Neurosciences Journal. 2016;21(4):314-318. DOI: https://doi.org/10.17712/nsj.2016.4.20150729
- Yoshida RA, Gorjão R, Mayer MPA, Corazza PFL, Guare RO, Ferreira ACFM, et al. Inflammatory markers in the saliva of cerebral palsy individuals with gingivitis after periodontal treatment. Brazilian oral research. 2019;33. https://doi.org/10.1590/1807-3107bor-2019.vol33.0033
- Lansdown K, Irving M, Mathieu Coulton K, Smithers‐Sheedy H. A scoping review of oral health outcomes for people with cerebral palsy. Special Care in Dentistry. 2022;42(3):232-243 https://doi.org/10.1111/scd.12671
- Hanci F, Türay S, Dilek M, Kabakuş N. Epilepsy and drug-resistant epilepsy in children with cerebral palsy: A retrospective observational study. Epilepsy & Behavior. 2020;112:107357. https://doi.org/10.1016/j.yebeh.2020.107357
- Zorii І, Pryimak K, Bidenko N, Kolenko Y, Volonyk I. Mathematical modeling of oral hygiene in children with cerebral palsy depending on the degree of severity of motor impairment and electroneuromyography parameters. 2023.
- Jahan I, Sultana R, Muhit M, Akbar D, Karim T, Al Imam MH, et al. Nutrition interventions for children with cerebral palsy in low-and middle-income countries: a scoping review. Nutrients. 2022;14(6):1211. https://doi.org/10.3390/nu14061211
- Jahan I, Muhit M, Hardianto D, Laryea F, Chhetri AB, Smithers‐Sheedy H, et al. Epidemiology of cerebral palsy in low‐and middle‐income countries: preliminary findings from an international multi‐centre cerebral palsy register. Developmental Medicine & Child Neurology. 2021;63(11):1327-1336. https://doi.org/10.1111/dmcn.14926
- Akhter R, Hassan NMM, Martin EF, Muhit M, Smithers-Sheedy H, Badawi N, et al. Caries experience and oral health-related quality of life (OHRQoL) of children and adolescents with cerebral palsy in a low-resource setting. BMC Oral Health. 2019;19:1-6. https://doi.org/10.1186/s12903-018-0704-2
- Karaseridis K, Dermata A. Cerebral palsy: Oral manifestations and dental management. Balkan Journal of Dental Medicine. 2023;27(1):1-7. DOI: 10.5937/bjdm2301001K
- Mopagar DG, Raurale A, Pendyala G, Sonawane P, Hadpe H, Kankerej U. Dental and medical management of children with cerebral palsy: Case series with. Medical Science. 2023;27:e118ms2845. doi: https://doi.org/10.54905/disssi/v27i132/e118ms2845
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
