By Muhammad Ali1, Muhammad Ghayasuddin1, Syeda Mahnoor Ali Shah2, Ramsha Waseem1, Wahb1, Khadijah Abid3
- General Surgery Department, Kulsoom Bai Valika Hospital, Karachi, Pakistan
- Advanced Laboratory Pvt Limited, Karachi, Pakistan
- Public Health Department, SZABIST, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/009
How to cite: Ali M, Ghayasuddin M, Shah SMA, Waseem R, Wahb, Abid K. Comparison of Skin Staples versus Skin Sutures After Inguinal Hernioplasty in Terms of Surgical Site Infection. Pak J Med Dent. 2024;13(1): 44-49. Doi: 10.36283/PJMD13-1/009
Background: Surgical site infection is a major concern following inguinal hernia repair, potentially leading to extended hospital stays, increased morbidity, patient discomfort, and higher healthcare costs. This study aimed to conduct a comparative analysis between skin staples and skin sutures in inguinal hernioplasty, explicitly focusing on their impact on surgical site infection rates.
Methods: From September 2022 to June 2023, a randomized control trial study was carried out at the Surgery Department, Kulsoom Bai Valika Hospital Karachi. A total of 100 patients who underwent Lichtenstein tension-free mesh hernioplasty were allocated into two groups: the stapler group (n=50) and the polypropylene suture group (n=50). The patients were monitored for 3 to 6 hours post-surgery and safely discharged on the first postoperative day. Follow-up was scheduled 7 days after surgery to assess wound complications, specifically surgical site infections. Comparison between both groups was done using the Chi-square/Fisher exact test for surgical site infection and independent samples t-test for pain score. The level of significance was set at 5%.
Results: The incidence of postoperative pain was slightly lower in the stapler group compared to the suture group (10% vs. 16%), this difference was not statistically significant (p=0.544). Moreover, the surgical site infection rate was significantly lower in the stapler group (3%) than in the suture group (12%) with p=0.012.
Conclusion: When securing the mesh in inguinal hernia cases, the utilization of skin staples was considered a safe approach and was associated with lower surgical site infection as compared to skin sutures.
Keywords: Hernia, Surgical wound infection, Surgical mesh, Postoperative complications
Hernia repair is a prevalent surgical procedure performed worldwide, with a staggering number of over 20 million individuals undergoing the treatment annually1,2. Among the different types of hernias, inguinal hernia is the most frequent one, accounting for 73% of all hernia cases, with a lifetime risk of 3% in females and 27% in males1,3. However, the procedure has challenges, literature reveals that surgical site infection (0.48%), bleeding (0.86%), and other complications (0.41%) are significantly associated with inguinal hernia repair1, 3. Surgical site infection is a major concern following inguinal hernia repair, potentially leading to extended hospital stays, increased morbidity, patient discomfort, and higher healthcare costs4,5. Identifying and minimizing risk factors of surgical site infection is crucial for achieving successful outcomes4, 5.
Numerous techniques have been explored for wound closure aimed at decreasing the rate of surgical site infections. Among the various methods, two primary approaches have gained popularity i.e., skin staples and skin sutures6-9. Polypropylene sutures, known for their monofilament structure and biologically inert properties, are the established method for securing the mesh along the posterior inguinal canal wall. Their use is associated with a lower likelihood of infections8, 9. However, there has been a recent adoption of skin staples made from stainless steel, which offer the advantage of easier placement and result in a remarkable 80% reduction in wound closure time when compared to polypropylene sutures6, 7, 10.
Research by Khulique et al. also found lower surgical site infection in mesh securing with skin staples as compared to conventional pro-lene 2/0 sutures (3.1% vs 12.3%, p=0.048). However, there was an insignificant difference in the incidence of seroma formation (p=0.403) and urinary retention between both groups (p=0.380) 11. Similarly, Munghate et al. reported 24% of wound infections in the suture group and 4% in the stapler group (p=0.001) 6.
In Pakistan, the prevalence of inguinal hernias is considerable, impacting both males and females.11 Given the healthcare landscape of the country, it becomes imperative to find effective strategies for mitigating the occurrence of surgical site infections following inguinal hernioplasty. Therefore, this study aimed to conduct a comparative analysis between skin staples and skin sutures in inguinal hernioplasty, specifically focusing on their impact on surgical site infection rates. The findings from this research are expected to play a pivotal role in optimizing surgical outcomes and enhancing post-operative recovery for patients in Pakistan.
From September 2022 to June 2023, a randomized control trial study was carried out at the Department of Surgery, Kulsoom Bai Valika Hospital in Karachi, Pakistan. Sample size calculation was performed on the Open Epi sample size calculator. The total sample size was 96 i.e. 48 patients in each group were estimated using statistics of wound infection as 24% in the suture group6 and 4% in the stapler group, power of test as 80% and 95% confidence level6. However, we have included 50 patients in each group. Patients of age more than 18 years of either gender having inguinal hernias, who underwent elective hernioplasty under general or spinal anesthesia were included in the study. Patients with congenital, irreducible, and sliding or massive scrotal hernias, strangulated and obstructed hernias, and patients with hypertension, diabetes, or coagulation disorders were not included in the study.
Ethical approval of the study was obtained from the ethical review committee. Written informed consent was obtained from all the eligible patients and information regarding age, gender, and BMI was collected. A total of 100 patients who underwent Lichtenstein tension-free mesh hernioplasty were divided into two groups: the polypropylene suture group (n=50) and the stapler group (n=50). The polypropylene suture group consisted of 50 patients, where a 7.5×15 cm mesh was secured using interrupted 2/0 Prolene sutures. In contrast, the stapler group also comprised 50 patients, with skin closure performed using a stainless-steel stapler used for securing the mesh. Subsequently, the wound was cleansed with pyodine, and an aseptic dressing was applied in both groups. Patients in both groups received Injections of Augmentin 1.2 gm during anesthesia induction and tablet Brufen as needed. Patients in both groups were monitored for three to six hours period until they had emptied their bladders, and they were safely discharged on the first postoperative day. Dressing guidelines and methods remained the same in both groups i.e., Mepore dressing opened after 72 hours of surgery and onwards changed 24 hourly.
A follow-up review was scheduled in the outpatient department 7 days after surgery for clip/stitch removal and to gather information regarding wound complications. Complications were categorized as surgical site infections (presence of pus discharge, inflammation, or fever > 100 °F) and post-operative pain (pain score>4 assessed using a visual analog scale). To ensure adequate follow-up, contact numbers of the patients were obtained. Bias and confounding factors were effectively managed by strictly adhering to the exclusion criteria.
The collected data was managed and analyzed using SPSS version 23. Mean and SD were reported for numeric data like age, BMI, and pain score. Frequency and percentage were reported for gender and surgical site infection. Comparison between both groups was done using the Chi-square/Fisher exact test for surgical site infection and independent samples t-test for pain score. The level of significance was set at 5%.
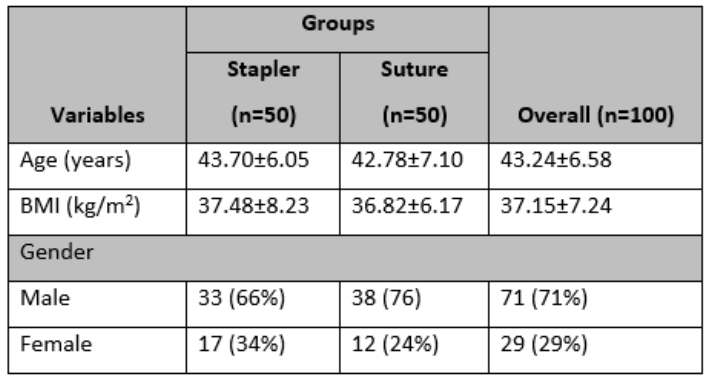
A total of 100 patients were included who underwent Lichtenstein tension-free mesh hernioplasty. The mean age of the patients was 43.24±6.58 years and the mean BMI of the patients was 37.15±7.24 kg/m2. Of 100 patients, 71% were males and 29% were females. In both groups, most of the patients were males. (Table 1)
Table 1: Baseline characteristics of study samples.
Of 100 patients, 13 (13%) patients had post-operative pain. Figure 1 shows post-operative pain (VAS>4) was lower in the stapler group as compared to the suture group (10% vs 16%) after a follow-up of 7 days. However, this difference was statistically insignificant with p=0.544.
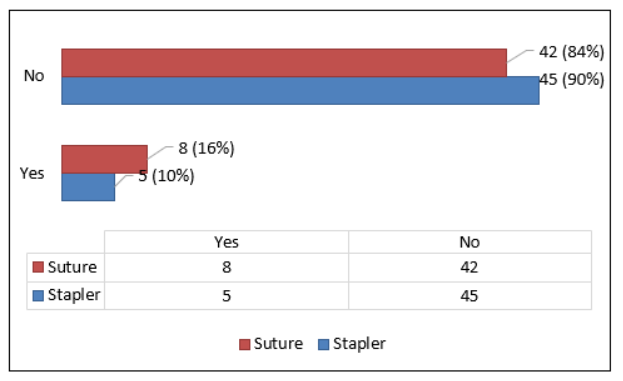
Figure 1: The distribution of post-operative pain (VAS>4) among both groups.
Of 100 patients, 15 (15%) patients developed surgical site infection. Figure 2 shows surgical site infection rate was lower in the stapler group as compared to the suture group (3% vs 12%) after a follow-up of 7 days. Moreover, this difference was statistically significant with p-value=0.012.
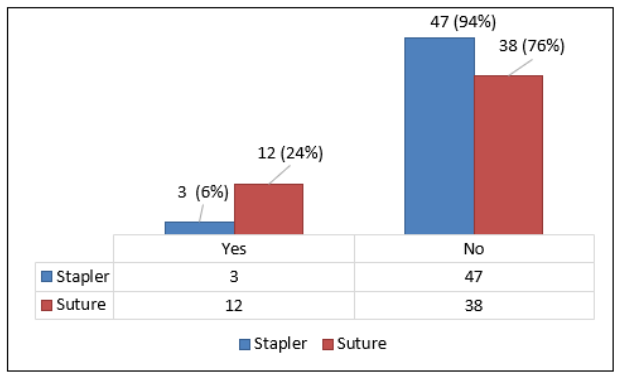
Figure 2: The distribution of surgical site infection (presence of pus discharge, inflammation, or fever > 100 °F) among both groups.
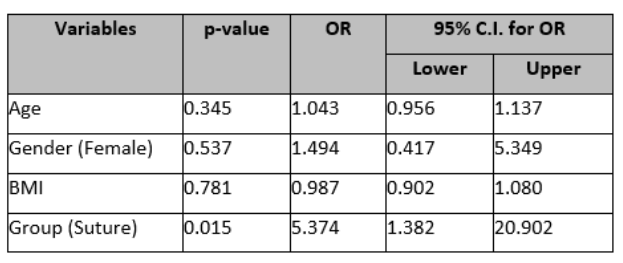
The age is not statistically significant in predicting surgical site infection. The odds ratio is 1.043, suggesting a very slight increase in the odds of surgical site infection for a one-unit increase in age (p=0.345). Gender is also not statistically associated with surgical site infection (p=0.537). However, the odds ratio is 1.494, indicating that, on average, females have 1.494 times higher odds of surgical site infection as compared to males. Furthermore, the odds of surgical site infection are 5.374 higher in the suture group as compared to the stapler group (p=0.015). (Table 2)
Table 2: Multivariate logistic regression analysis for surgical site infection
The management of inguinal hernia has undergone continuous evolution for more than 150 years6, 12. Numerous modifications have been implemented in this approach, demonstrating varying levels of effectiveness6-9, 11, 13. Among these advancements, Lichtenstein introduced the tension-free inguinal hernioplasty, which has proven to be a highly effective and safe technique with a lower recurrence rate9, 14, 15. Initially, the mesh fixation on the posterior inguinal canal wall was performed using polypropylene 2/0 suture. However, this method significantly impacted patients’ quality of life and recovery16. In recent decades, a new approach has emerged, utilizing staples instead of polypropylene sutures for mesh fixation. This innovative method has been associated with reduced operative time and complications such as wound infection6, 7, 11, 17. Consequently, the current study aims to compare the use of skin staplers and sutures for securing the mesh, with a specific focus on evaluating the occurrence of surgical site infections.
We found the mean age of patients in the stapler group was 43.70±6.05 years, while in the suture group, it was 42.78±7.10 years. Similarly, Wani et al., reported mean ages of 46.75 ± 12.02 years in the suture group and 46 ± 12.10 years in the stapler group in their study at Srinagar18. Likewise, Khan et al. conducted a similar study in Pakistan and found a similar pattern of age distribution, with a mean age of 48.9±14.3 years in the suture group and 46.4±14.1 years in the stapler group19. These consistent findings regarding the mean age of patients in both the stapler and suture groups across different studies may be attributed to the common occurrence of inguinal hernia in various age groups and the standardized selection criteria employed by researchers.
In our study, most of the participants with inguinal hernia were males and had a mean BMI of 37.15±7.24 kg/m2. Ali et al. in their research also found that most of the patients were males, and had a mean BMI of 35.7 kg/m2 15. Wani et al. also observed a higher proportion of males than females.18 The predominance of male patients with higher mean BMI in all studies, may suggest possible gender and BMI-related factors contributing to inguinal hernia occurrence20-22.
In the current study, we found a similar proportion of post-operative pain in both groups (p=0.544). The same findings were reported by previous studies, where they also observed the same proportion of pain in both groups6, 23. Furthermore, Garg and colleagues reported that the duration of pain was comparable in both groups, spanning 2 days24. In contrast, Khan and colleagues discovered a notable reduction in pain within the stapler group in contrast to the suture group, with a significant p-value of 0.02619. The lack of significant difference in postoperative pain observed in our study and the cited studies may be attributed to advancements in surgical techniques and anesthesia management, standardized post-operative pain management protocols, and balanced representation of patient characteristics between the stapler and suture groups.
The present study revealed a notable decline in the occurrence of surgical site infections within the stapler group in contrast to the suture group (3% vs. 12%, p=0.012). Even after adjustment in the multivariate logistic regression model, the odds of surgical site infection remain significantly higher in the suture group as compared to the stapler group. Likewise, Khulique et al. discovered a decreased frequency of surgical site infections when employing skin staples for mesh fixation compared to the traditional prolene 2/0 sutures (3.1% vs. 12.3%, p=0.048) 11. Similarly, Munghate et al. reported a higher incidence of wound infection in the suture group (24%) compared to the stapler group (4%, p=0.001) 6. Attaullah et al. found only two cases of surgical site infection in the staple group and 12 cases in the polypropylene suture group in a similar study25. However, Wani et al. found no significant difference in wound infection rates between the suture group and stapler group, and Garg et al. reported no cases of wound infection in either group during the post-operative period18, 24. The observed significant differences in surgical site infection rates between the stapler and suture groups in various studies can be attributed to the different methods of mesh fixation, which might affect wound healing and infection risk. Additionally, variations in patient populations, surgical techniques, and post-operative care protocols may also contribute to the differences in infection rates observed among the studies.
The study has a few limitations. One limitation of the study is that it was conducted at a single center, which may limit the generalizability of the findings to other healthcare settings or populations. Additionally, the follow-up period for assessing complications was relatively short (7 days), which might not capture delayed-onset complications. A longer follow-up duration could have provided a more comprehensive understanding of the outcomes. Lastly, the study did not account for potential confounding variables such as patients’ comorbidities or smoking status, which might influence surgical site infection rates. For future studies, we recommend conducting multicenter randomized controlled trials with longer follow-up periods and incorporating comprehensive data on potential confounding factors (e.g., comorbidities, smoking status) to further validate the benefits of using skin staples over skin sutures for mesh fixation in inguinal hernioplasty and to explore potential predictors of surgical site infection.
The use of skin staples for mesh fixation in inguinal hernia repair emerges as a promising approach, demonstrating both safety and a notably lower incidence of surgical site infections when contrasted with the traditional use of skin sutures. This finding underscores the potential benefits of incorporating skin staples into hernioplasty procedures, not only for enhancing patient outcomes but also for optimizing healthcare resource utilization. Further research and clinical studies are warranted to validate these findings and solidify the case for this innovative technique as a standard practice in hernia surgery.
None.
There is no conflict of interest among authors.
Ethical approval of the study was obtained from the ethical review committee of the institute (SGR-2020-187-11675).
Written informed consent was obtained from all the eligible patients.
MA, MG W: Conceptualization, Methodology design, Manuscript writing and editing, Literature review, Manuscript review. KA: Data analysis and interpretation, Manuscript review, and final approval. SMA, RW: Data collection and validation, manuscript drafting and revision, data entry and management, drafting specific sections of the manuscript, project supervision.
- Maneck M, Köckerling F, Fahlenbrach C, Heidecke CD, Heller G, Meyer HJ, et al. Hospital volume and outcome in inguinal hernia repair: analysis of routine data of 133,449 patients. Hernia 2020;24(4):747-757. DOI: 10.1007/s10029-019-02091-8.
- Melkemichel M, Bringman S, Nilsson H, Widhe B. Patient-reported chronic pain after open inguinal hernia repair with lightweight or heavyweight mesh: a prospective, patient-reported outcomes study. BJS (British Journal of Surgery) 2020;107(12):1659-1666. DOI: https://doi.org/10.1002/bjs.11755.
- Jenkins JT, O’Dwyer PJ. Inguinal hernias. Bmj 2008;336(7638):269-272. DOI: 10.1136/bmj.39450.428275.AD.
- Wilson RB, Farooque Y. Risks and Prevention of Surgical Site Infection After Hernia Mesh Repair and the Predictive Utility of ACS-NSQIP. Journal of Gastrointestinal Surgery 2022;26(4):950-964. DOI: 10.1007/s11605-022-05248-6.
- Hou Y, Collinsworth A, Hasa F, Griffin L. Incidence and impact of surgical site infections on length of stay and cost of care for patients undergoing open procedures. Surg Open Sci 2023;11:1-18. DOI: 10.1016/j.sopen.2022.10.004.
- Munghate A, Mittal S, Singh H, Singh G, Yadav M. Skin staples: a safe technique for securing the mesh in Lichtenstein hernioplasty as compared to suture. Surg Res Pract 2014;2014:958634. DOI: 10.1155/2014/958634.
- Basit A, Abbasi SH, Haider S, Kiani YM, Shah FH. To Compare Outcomes of Stainless Skin Staples and Polypropylene Sutures for Skin Closure in Clean Elective Surgeries. Isra Med J 2018;10(1):32-35.
- Tanasescu C, Moisin A, Mihetiu A, Serban D, Costache A, Bratu DG. The use of polypropylene mesh in inguinal hernia surgery: A retrospective study. Exp Ther Med 2021;22(4):1193. DOI: 10.3892/etm.2021.10627.
- Saha T, Wang X, Padhye R, Houshyar S. A review of recent developments of polypropylene surgical mesh for hernia repair. OpenNano 2022;7:100046. DOI: https://doi.org/10.1016/j.onano.2022.100046.
- Huda F, Gajula B, Singh S, et al. (March 06, 2021) Staples Versus Sutures for Skin Closure in Standard Four Port Laparoscopic Cholecystectomy: A Prospective Cohort Study. Cureus 13(3): e13725. doi:10.7759/cureus.13725.
- Khulique A, Khan S, Khan R, Sundas M, Asad H. SECURING MESH WITH SKINSTAPLES VERSUS PROLENE SUTURE IN INGUINAL HERNIA REPAIR: EFFECTS ON POST-OPERATIVE COMPLICATIONS. Pakistan Armed Forces Medical Journal 2020;70(2):433-436.
- International guidelines for groin hernia management. Hernia 2018;22(1):1-165. DOI: 10.1007/s10029-017-1668-x.
- Mabula JB, Chalya PL. Surgical management of inguinal hernias at Bugando Medical Centre in northwestern Tanzania: our experiences in a resource-limited setting. BMC Research Notes 2012;5(1):585. DOI: 10.1186/1756-0500-5-585.
- Ersoz F, Culcu S, Duzkoylu Y, Bektas H, Sari S, Arikan S, et al. The Comparison of Lichtenstein Procedure with and without Mesh-Fixation for Inguinal Hernia Repair. Surgery Research and Practice 2016;2016:8041515. DOI: 10.1155/2016/8041515.
- Ali A, Bukhari SUS, Awan SA, Ahmed U, Ahmed A, Babar MW. Comparison between Desarda’s Inguinal Hernia Repair and Lichtenstein Hernioplasty in terms of Complications, Operative time, and Cost-effectiveness. Pakistan Armed Forces Medical Journal 2022;72(4):1339-1342.
- Mitura K, Garnysz K, Michałek I. Long-term follow-up of a randomized controlled trial of Lichtenstein repair vs the Valenti technique for inguinal hernia. Hernia 2019;23(3):547-554. DOI: 10.1007/s10029-019-01879-y.
- See CW, Kim T, Zhu D. Hernia mesh and hernia repair: a review. Engineered Regeneration 2020;1:19-33.
- Mumtaz Ud Din Wani AM, Mohammad Yaqoob Bhat, Shabir Ahmad Mir. A comparative study of skin staples versus sutures for fixing mesh in tension-free mesh hernioplasty. Archives of Clinical and Experimental Surgery 2018;7(1):7-12.
- Khan AA, Majeed S, Shahzadi M, Hussain SM, Ali MZ, Siddique K. Polypropylene suture versus skin staples for securing mesh in lichtenstein inguinal hernioplasty. J Coll Physicians Surg Pak 2014;24(2):88-90.
- Alansari AH, Sr., Almalawi AM, Alghamdi A, Alghamdi MS, Hazazi HA, Aljabri AA, et al. Body Mass Index Within Multifactor Predictors of Ventral Hernia Recurrence: A Retrospective Cohort Study. Cureus 2023;15(6):e41148. DOI: 10.7759/cureus.41148.
- Melwani R, Malik SJ, Arija D, Sial I, Bajaj AK, Anwar A, et al. Body Mass Index and Inguinal Hernia: An Observational Study Focusing on the Association of Inguinal Hernia With Body Mass Index. Cureus 2020;12(11):e11426. DOI: 10.7759/cureus.11426.
- Zendejas B, Hernandez-Irizarry R, Ramirez T, Lohse CM, Grossardt BR, Farley DR. Relationship between body mass index and the incidence of inguinal hernia repairs: a population-based study in Olmsted County, MN. Hernia 2014;18(2):283-288. DOI: 10.1007/s10029-013-1185-5.
- van der Zwaal P, van den Berg IR, Plaisier PW, Tutein Nolthenius RP. Mesh fixation using staples in Lichtenstein’s inguinal hernioplasty: fewer complications and fewer recurrences. Hernia 2008;12(4):391-394. DOI: 10.1007/s10029-008-0353-5.
- Garg CP, Bhatnagar AM, Parmar CD, Darshan JR, Sehgal RA. Comparative study of skin staples and polypropylene sutures for securing the mesh in lichtenstein’s tension free inguinal hernia repair: a prospective randomized controlled clinical trial. 2004.
- Attaullah, Haider SA, Rajput A, Ahmed S, Owais MA Jabeen W. Securing mesh with staples is safe and time saving in Lichtenstein inguinal hernioplasty. J Surg Pakistan. 2020; 25(1):22-26. Doi:10.21699/jsp.25.1.6.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
