By Mahzareen1, Saba Zaidi1, Naveeduddin Ahmed1
- Neurology Department, Liaquat National Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/019
How to cite: Mahzareen, Zaidi S, Ahmed N. A Rare Cause of Dementia in a Young Adult – A Case Report. Pak J Med Dent. 2024;13(1): 108-111. Doi: 10.36283/PJMD13-1/019
Frontotemporal dementia is a clinically and pathologically heterogeneous group of disorders with two main phenotypes; the commoner being a disorder of behavior and function. This dementia is most common before age 60 with more than half being seen in the age range 45-65 years. We report the case of a 27-year-old gentleman who presented with behavioral & personality changes 2 years before his presentation in our clinic. A neurological examination revealed a restless patient with gibberish speech and a positive snout reflex. The rest of the examination was non-focal. MRI brain showed significant atrophy of frontal and temporal lobes with intact parietal and occipital cortex. Based on clinical and radiological findings, we made the diagnosis of Frontotemporal dementia. Our case emphasizes the need to differentiate young-onset dementia from primary psychiatric disorders which are relatively more common at a young age.
Keywords: Frontotemporal dementia, Nervous system diseases, Young adult.
Frontotemporal dementia is characterized by personality, behavioral, and cognitive changes due to progressive atrophy of the frontal or temporal lobes1. 30-50% of the cases have noticeable family history2. Many patients who have young-onset dementia present with features consistent with schizophrenia3. We report the case of a 27-year-old gentleman who presented with behavioral and personality changes 2 years before presentation in our OPD. There was significant cognitive decline and his primitive reflexes were positive, this leads us to diagnose dementia rather than primary affective or psychotic disorder. Our patient meets the diagnostic criteria of probable behavioral variant FTD.
A 27 years old man, right-handed, residing in Afghanistan presented with 2 years history of altered behavior. He had symptoms including anger outbursts, weeping spells, and difficulty in expressing himself. His brother further added that there was a lack of inhibition resulting in inappropriate behavior such as outbursts, touching unknown persons, public micturition, and diminished social understanding. They have noticed restlessness, irritability, aggressiveness, violent outbursts, and excessive sentimentality. Although his language was fluent but was full of paraphasic errors. There was no history of mood, anxiety, or auditory or visual hallucinations. Neither there was any guilt, self-blame, or suicidal thoughts in the beginning. Family history was not significant as far as dementia or primary psychiatric illness is concerned. He was managed on lines of schizophrenia and his symptoms progressively worsened. He received a combination of typical or atypical antipsychotics but there was a failure to respond. Neurological examination revealed a young boy of average height and build, conscious having gibberish speech. He was yelling and crying during interviews at the clinic. He had difficulty in following commands. Mini-mental state examination was limited due to impaired comprehension. He did not remember the date/time/year or country/city; on repetitive asking. Not able to calculate as well. There were full extra-ocular movements in all directions and no facial asymmetry. Bulk, tone, and power were normal and reflexes were intact. Gait was normal with no gross ataxia. Plantars were flexor. Primitive reflex like the snout reflex was positive. Considering a case of medically refractory psychiatric illness and progressive cognitive decline we proceeded with neuroimaging. MRI brain showed significant atrophy of bilateral frontal, anterior temporal lobes, and head of caudate atrophy. (Figure 1) TSH and vitamin B12 levels were normal. Functional neuroimaging (FDG-PET) and genetic studies were not available in our setup. His CSF studies, EEG, and autoimmune encephalitis panel were normal. Although he was diagnosed as a case of primary psychiatric disorder progressive cognitive decline, poor response to antipsychotics, and atrophy in neuroimaging led us towards a neurodegenerative process. According to the international consensus diagnostic criteria of behavioral variant of frontotemporal dementia if the patient fulfills the three features, then he comes under the heading of possible FTD in our case there was behavioral disinhibition, apathy, and loss of sympathy. Further adding the significant functional decline in our case with atrophy of the frontal and temporal lobe made him the case of probable behavioral variant of FTD. So, a clinical-radiological diagnosis of probable frontotemporal dementia was made.
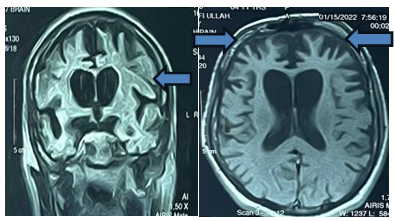
Figure 1: MRI brain FLAIR & T1 axial sequence showing significant atrophy of bilateral frontal, anterior temporal lobes, and head of caudate atrophy.
Frontotemporal dementia is a leading cause of young onset dementia, with about 5–17% of cases diagnosed on biopsy presented under the age of 70. It can present as a consolidation of clinical features, varying from behavioral alteration to significant language dysfunction. Research conducted on the prevalence of young onset dementia showed youngest individual in their cohort had FTD symptoms at age 20 years and was found to have MAPT (microtubule-associated protein tau) mutation. Three causes of young-onset dementia are hereditary, sporadic, or multifactorial. (4)6.
Young-onset FTD includes cases before the age of 30, they usually present with frequent abrupt mood changes, increased agitation, and aggression, disinhibition, loss of empathy, and decline in working memory. There are three clinical types of FTD: behavioral variant (bv FTD) and two forms of primary progressive aphasia, which include non-fluent or fluent aphasia. In addition, FTD can combine with another neurodegenerative diseases like Corticobasal degeneration, progressive supranuclear palsy, and amyotrophic lateral sclerosis (ALS). Approximately 30–50% of FTD cases have some family history of dementia, Parkinsonism, or ALS, and 10–20% have a genetic cause. A positive family history of dementia/parkinsonism/ALS classically shows a pattern of Autosomal Dominance with high penetrance, with at least one first-degree relative being affected 4.
There is a substantial relation between behavioral variants of frontotemporal dementia and psychiatric disorders owing to symptoms such as apathy, disinhibition, and stereotyped behavior5. Primary psychiatric disorder had been diagnosed in a large number of patients presenting earlier than the identification of frontotemporal dementia6. Patients with dementia are usually diagnosed with psychiatric illness either because their symptoms might start with psychiatric complaints or because these symptoms of dementia are mistakenly taken as those of a primary affective disorder. Psychiatric misdiagnosis is moderately common in dementias, particularly the FTD. Frontotemporal dementia consists of various clinical syndromes including behavioral variant frontotemporal dementia, semantic dementia, and progressive non-fluent aphasia. Behavioral variant FTD is defined by persistent alteration in behavior, mood, and personality. Behavioral changes may include unconstrained, oppression, lack of insight, social improperness, excessive playfulness, and overeating. Patients’ construct weakens ethical decisions and usually shows unsocial behaviors like obscene exposure, turbulent driving, and wrongdoing. Mood disturbances including passivity, exhilaration, and annoyance are common; and personality changes include a lack of communal friendliness, compassion, self-confidence, and forwardness. Because of these clinical presentations, patients with behavioral variant FTD usually receive diagnoses of depressive disorder, bipolar affective disorder, or schizophrenia. A literature review showed that in 252 patients with different types of dementia, 28.2% were labeled with a primary psychiatric disorder before dementia. The percentage of previous psychiatric diagnosis varies from <12% in patients with progressive nonfluent aphasia, corticobasal degeneration, or amyotrophic lateral sclerosis to 24.3% in Semantic dementia, 23.1% in Alzheimer’s disease and 50.7% in behavior variant FTD7.
Definitive diagnosis of neurodegenerative disorders usually requires histopathology, functional neuroimaging like FDG-PET scans, and specific genetic studies related to young onset dementia. Living in a developing country with limited diagnostic facilities we can rely more on the clinical presentation, specific neurological findings, and then structural neuroimaging. We can rule out the other possible differentials on CSF studies and autoimmune antibodies, as in the above-mentioned case. Our case fulfilled the defined international consensus diagnostic criteria of probable FTD as mentioned above. Being a well-known entity of neurodegenerative disorder, there are limitations to what we can offer to patients suffering from frontotemporal dementia. The particular dementia treatment like Memantine and Rivastigmine can be thought about in such cases although Donepezil worsens behavioral symptoms in some cases. Even though antipsychotics carry risks as well, we usually consider atypical antipsychotics and SSRIs to control agitation. Trazodone can be given for sleep disturbance.
We need to discuss the caregivers regarding their role in patient management and end of the life decisions as well. To handle patients like these, we need to spread awareness to imply non-pharmacological strategies, such as; the identification of triggers for agitated behavior, relaxation therapies including music and, in our culture, religious poetry, massage, and keeping them clean with extreme dietary care to fulfill their caloric needs. With the progression of the disease process, these people lack social insight which is; recognition of family members and wandering outside, givers should place a bracelet or a card in their pocket as a mark of identification.
FTD is one of the familiar causes of young-onset dementia and is often presented as a psychiatric illness like depression, schizophrenia, obsessions, compulsive thoughts, or bipolar disorder. The rapid decline in socio-emotional and language – two characteristic human abilities – is devastating, particularly when onset of the dementia is in late middle age. Awareness regarding the variability in possible presentation associated with FTD can aid in early and accurate identification. Differentiation of dementia among the young, from that of primary psychiatric disorder, is difficult at times and it requires detailed history, and clinical and radiological evidence to reach a consensus. This case report highlights this fact.
None to declare
None to declare
The consent of the patients was taken before the writing of the manuscript.
All authors contributed equally.
- Merrilees J, Klapper J, Murphy J, Lomen-Hoerth C, Miller BL. Cognitive and behavioral challenges in caring for patients with frontotemporal dementia and amyotrophic lateral sclerosis. Amyotrophic lateral sclerosis: official publication of the World Federation of Neurology Research Group on Motor Neuron Diseases. 2010;11(3):298-302. doi: 10.3109/17482961003605788.
- Goldman JS, Farmer JM, Van Deerlin VM, Wilhelmsen KC, Miller BL, Grossman M. Frontotemporal Dementia:: Genetics and Genetic Counseling Dilemmas. The neurologist. 2004;10(5):227-234. doi: 10.1097/01.nrl.0000138735.48533.26.
- Kelley BJ, Boeve BF, Josephs KA. Young-onset dementia: demographic and etiologic characteristics of 235 patients. Archives of neurology. 2008;65(11):1502-1508. doi: 10.1001/archneur.65.11.1502.
- Goldman JS. Genetic testing and counseling in the diagnosis and management of young-onset dementias. Psychiatric Clinics. 2015;38(2):295-308. doi: 10.1016/j.psc.2015.01.008.
- Pose M, Cetkovich M, Gleichgerrcht E, Ibáñez A, Torralva T, Manes F. The overlap of symptomatic dimensions between frontotemporal dementia and several psychiatric disorders that appear in late adulthood. International Review of Psychiatry. 2013;25(2):159-167. doi: 10.3109/09540261.2013.769939.
- Woolley JD, Khan BK, Murthy NK, Miller BL, Rankin KP. The diagnostic challenge of psychiatric symptoms in neurodegenerative disease: rates of and risk factors for prior psychiatric diagnosis in patients with early neurodegenerative disease. The Journal of Clinical Psychiatry. 2011;72(2):126-133. doi: 10.4088/JCP.10m06382oli.
- Kipps CM, Hodges JR, Hornberger M. Nonprogressive behavioral frontotemporal dementia: recent developments and clinical implications of the ‘bvFTD phenocopy syndrome’. Current opinion in neurology. 2010 Dec 1;23(6):628-632. doi: 10.1097/WCO.0b013e3283404309.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
