By Khalida Nasreen1, Samia Ghulam Mohammad1
- Obstetrics & Gynaecology Department, Bahria University Health Sciences Campus, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD13-1/020
How to cite: Nasreen K, Mohammad SG. A Multilobulated Intramural Fibroid in Pregnancy: A Clinical Case Report. Pak J Med Dent. 2024;13(1): 112-115. Doi: 10.36283/PJMD13-1/020
Leiomyoma is the most common benign tumor of the female reproductive tract. It is prevalent among women in the age group 30 to 50 years. Other than placental estrogens and progesterone, a range of endocrine and paracrine factors have their impact on fibroid blood supply, growth rate, and risk of degeneration during the gestational and puerperal periods. The current case report is about a 30-year-old primigravida with pregnancy and a large fibroid presenting with complications such as malpresentation and pressure symptoms, ending up in a cesarean section at 36 weeks delivering a live baby with a birth weight of 2.5 kgs and a large fibroid weighing 6.4 kg. During the pregnancy, there was adequate fetal development, without major maternal complications. There were four crucial issues: tailored pregnancy surveillance, the decision of time and route of delivery, postpartum hemorrhage management, the decision to perform an interval myomectomy, and the management of decreasing blood loss perioperatively.
Keywords: Leiomyoma, Labor Presentation, Postpartum Hemorrhage.
Uterine leiomyomas are benign smooth muscle tumors of the uterus. It is the commonest benign tumor of female genital tract incidence being 20 – 40%. Their incidence in pregnancy has been reported to be 1-4%1, 2. They remain asymptomatic, except in 10-30 % of the cases where they present with complications. The main course of treatment is often to manage them conservatively followed by myomectomy after delivery2. Pregnancy with fibroid has become increasingly common as most women delay their first pregnancy until later than 30 years of age which eventually leads to complications in pregnancy3. Uterine fibroids in pregnancy which are larger than 5cm and multiple tend to present with obstetric complications4. They are variably linked to spontaneous abortion, intrauterine growth restriction (IUGR), anemia, multiple blood transfusions, infection, pain due to degeneration of fibroid, malposition of fetus, preterm delivery, preterm premature rupture of membranes (PPROM), malpresentation, placental abruption, uterine inertia, increased rates of cesarean section, postpartum hemorrhage, retention of the placenta, hysterotomy and obstetric hysterectomy. Fetal outcomes may also be affected leading to decreased Apgar scores in low birth weight babies4-8.
We are discussing a case of a patient with a large multilobulated intramural fibroid occupying the whole posterior lateral wall of the uterus in pregnancy. Our patient was a 30-year-old primigravida married for 10 months, with planned spontaneous conception diagnosed with pregnancy with fibroid uterus at 8 weeks of gestation in a secondary-level facility. Diagnosis of fibroid was an incidental finding on an ultrasound done for confirmation of pregnancy and dating. On the initial ultrasound, it was suspected as a single broad-based sub-serosal pedunculated fibroid arising from the fundus and right posterior lateral wall of the uterus about 14 x 30 cm in size.
The patient was being supervised in this secondary health care unit where she was advised to continue her pregnancy and was started on progesterone therapy for prophylaxis against miscarriage. The patient remained asymptomatic all this time. However, the size of the fibroid kept on increasing, and eventually at 26 weeks she was referred to a tertiary care center with a specialized Gynecologist for the continuous medical care and management of her pregnancy.
At 26 weeks when she came to us, she was vitally stable with no signs of pallor, or respiratory distress and no pedal edema. Upon abdominal examination, the abdomen was distended and there was a big abdominopelvic mass measuring about 40 cm from the symphysis pubis, firm in consistency and mobile. On the ultrasound, it measured about 18 x 35 cm occupying the right side of the abdomen extending up to the right lateral fundal region of the uterus, pushing the gravid uterus towards the left. Anteriorly, it pushed the anterior abdominal wall, posteriorly pressing over the retro peritoneum causing a pressure effect, pressing the right ureter resulting in mild hydronephrosis. The baby at 27 weeks by dates was at 26 weeks of gestation on ultrasound with normal AFI. Her Hemoglobin was 11.2 g/dl, blood group B positive and serum electrolytes and urea creatinine were all normal.
We aimed to prolong the pregnancy as the patient remained asymptomatic, except for feeling pressure symptoms and mild discomfort due to a distended abdomen. Routine antenatal care was given, with two weekly antenatal visits. She was continued on progesterone therapy till 36 weeks of gestation. All her ultrasound reports till 36 weeks were normal, with normal fetal biometric parameters and AFI. Throughout her antenatal period, the fetus was with breech presentation.
She was admitted for surgery at 36 weeks after which a course of dexamethasone was given to her to improve fetal lung maturity. The baby was in a breech position, and an elective cesarean section was planned with 2 units of blood arranged on hemoglobin of 10.8g/dl. A high-risk informed consent was taken from the patient and relatives for myomectomy, chances of cesarean hysterectomy, ICU admission, and fetal risks explained.
A fresh ultrasound report at this point showed a subserosal fibroid of 28 x 36 cm originating from the right posterior wall of the uterus, pushing the uterus to the left side of the abdomen, superiorly reaching up to the epigastric region and in a downward direction pressing upon the urinary bladder.
Her Cesarean section was planned under spinal anesthesia, a midline infra umbilical skin incision was given. Fig 1 shows the outline of the uterus with fibroid through the abdominal incision. Upon opening of the abdomen, the fibroid was found to be intramural arising from the posterior wall, and occupying almost the entire anterior surface of the uterus as it was dextrorotated to the left so that the right tube was lying anteriorly.
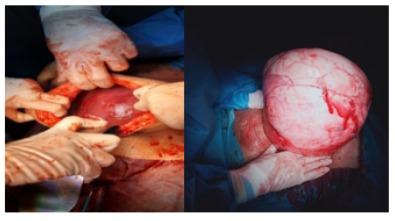
Figure 1: a) shows incision and dextrorotation of uterus b) demonstrates outline of uterus andfibroid.
The uterus was manipulated to correct the anatomy and to find a space to make the incision for easy delivery of the baby. It was repositioned with the help of assistance and a lower segment transverse incision was given into the uterus, the amniotic sac was punctured with artery forceps to deliver a breech baby boy of 2.5 k.gs with an adequate amount of liquor and APGAR scores of 8 and 10 at 1 and 5 minutes. After the placenta and membranes were delivered, the uterus was carefully stitched in a single layer, and hemostasis secured. About 1200ml of blood was lost during the procedure. She was then transfused with 2 units of blood postoperatively. Analgesics and antibiotics were given and meticulous monitoring was done for postpartum hemorrhage in the postoperative period.
The patient remained hospitalized for three days on intravenous antibiotics after which she was discharged on oral antibiotics with a plan of myomectomy after 3 months. The postoperative period remained uneventful. She visited on the 10th postoperative day for the opening of stitches which were healthy.

Figure 2: a) Fibroid measuring 20x35cm is removed, b) shows fibroid post-removal, and c) displays the weight of fibroid.
Her myomectomy was later done after 3 months through the same midline infra umbilical skin incision and an intramural fibroid of about 6.4 kg was removed from the uterus, 2 points of blood were transfused postoperatively (figure 2). Hemorrhage was controllable and the uterus was conserved restoring the normal anatomy. The postoperative period remained uneventful, and the fibroid was sent for a histopathology report which confirmed leiomyoma. She has also advised contraception for the next 2 years.
Different fibroid features for example its site, size, single or multiple; affect pregnancy outcomes in various ways. These facts can be used to help counsel women about the risks related to pregnancy and stratify their management accordingly.
Fibroid uterus has often been related to adverse pregnancy outcomes with reasons not very well explained8. Fibroids are not very symptomatic most of the time except being reported in 10-30 % of the cases where large fibroids may present with complications like lower abdominal pain in the 2nd and 3rd trimesters indicative of red degeneration of fibroid or preterm labor4, 10, 12. the incidence of early miscarriages is also more common with multiple or multilobulated fibroids while patients with sub mucous fibroids are also at risk of recurrent miscarriages8. The risk of preterm labor is also greatly increased with both multiple fibroids and fibroids greater than 5 cm in size10, 11.
Multiple fibroids in the lower segment of the uterus or cervical fibroids increase the probability of cesarean section as they cause malpresentation, abnormal lie, interference in head engagement, incoordinate uterine contractions, labor dystocia, and obstructed labor in some cases12,13, 14, 15. A fibroid uterus greater than 5 cm in size also increases the risk of postpartum hemorrhage at delivery due to interference in contraction.
Myomectomy at the time of cesarean delivery is associated with severe hemorrhage and should be considered in carefully selected cases like sub-serous or pedunculated fibroids. However cesarean myomectomy with large fibroids in the hands of experienced surgeons in tertiary care settings with stepwise de-vascularization is reasonably safe15-17.
Pregnancy with fibroids is usually asymptomatic but can be associated with various adverse events during pregnancy which include but are not limited to high cesarean section rates, threatened preterm labor, post postpartum hemorrhage. However, good selection criteria need to be applied to personalize patient care for optimal results. Cesarean myomectomy can be performed with good results in carefully selected cases, as was obtained in this case report.
The authors would like to acknowledge the hospital staff for their immense contribution.
The authors declare no conflict of interest.
Informed and written consent was acquired from the patient.
All authors equally contributed to the study.
- Karia HB, Maniar D, Gosai K. Case Report of Pregnancy with Huge Fibroid. Obstet Gynecol Cases Rev 2021; 1(8):189-191. doi.org/10.23937/2377-9004/1410189.
- Eyong E, Okon OA. Large Uterine Fibroids in Pregnancy with Successful Caesarean Myomectomy. Case Rep Obstet Gynecol. 2020 10;2020:8880296. doi: 10.1155/2020/8880296.
- Morgan Ortiz F, Piña Romero B, Elorriaga García E, Báez Barraza J, Quevedo Castro E, Peraza Garay Fde J. Miomas uterinos durante el embarazo y su repercusión en el resultado obstétrico [Uterine leiomyomas during pregnancy and its impact on obstetric outcome]. Ginecol Obstet Mex. 2011; 79(8):467-473. Spanish.
- Ciavattini A, Clemente N, Delli Carpini G, Di Giuseppe J, Giannubilo SR, Tranquilli AL. Number and size of uterine fibroids and obstetric outcomes. J Matern Fetal Neonatal Med. 2015 ;28(4):484-488. doi: 10.3109/14767058.2014.921675.
- Coronado GD, Marshall LM, Schwartz SM. Complications in pregnancy, labor, and delivery with uterine leiomyomas: a population-based study. Obstet Gynecol. 2000 ;95(5):764-769. doi: 10.1016/s0029-7844(99)00605-5.
- Doğan S, Özyüncü Ö, Atak Z. Fibroids During Pregnancy: Effects on Pregnancy and Neonatal Outcomes. J Reprod Med. 2016 ;61(1-2):52-57.
- Jenabi E, Khazaei S. The effect of uterine leiomyoma on the risk of malpresentation and cesarean: a meta-analysis. J Matern Fetal Neonatal Med. 2018 ;31(1):87-92. doi: 10.1080/14767058.2016.1275553.
- Lam SJ, Best S, Kumar S. The impact of fibroid characteristics on pregnancy outcome. Am J Obstet Gynecol. 2014 ;211(4):395.e1-5. doi: 10.1016/j.ajog.2014.03.066.
- Qidwai GI, Caughey AB, Jacoby AF. Obstetric outcomes in women with sonographically identified uterine leiomyomata. Obstet Gynecol. 2006 ;107(2 Pt 1):376-82. doi: 10.1097/01.AOG.0000196806.25897.7c.
- Gupta S, Jose J, Manyonda I. Clinical presentation of fibroids. Best Pract Res Clin Obstet Gynaecol. 2008 ;22(4):615-626. doi: 10.1016/j.bpobgyn.2008.01.008.
- Salvador E, Bienstock J, Blakemore KJ, Pressman E. Leiomyomata uteri, genetic amniocentesis, and the risk of second-trimester spontaneous abortion. Am J Obstet Gynecol. 2002 ;186(5):913-915. doi: 10.1067/mob.2002.123988.
- Tîrnovanu MC, Lozneanu L, Tîrnovanu ŞD, Tîrnovanu VG, Onofriescu M, Ungureanu C, Toma BF, Cojocaru E. Uterine Fibroids and Pregnancy: A Review of the Challenges from a Romanian Tertiary Level Institution. Healthcare (Basel). 2022 6;10(5):855. doi: 10.3390/healthcare10050855.
- Stout MJ, Odibo AO, Graseck AS, Macones GA, Crane JP, Cahill AG. Leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes. Obstet Gynecol. 2010 ;116(5):1056-1063. doi: 10.1097/AOG.0b013e3181f7496d.
- Abam DS, Kasso T. Uterine Fibroids and Pregnancy: A Review of the Challenges. Obstetrics. InTech; 2017. Available from: http://dx.doi.org/10.5772/intechopen.71761
- Klatsky P. C., Tran N. D., Caughey A. B., Fujimoto V. Y. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. American Journal of Obstetrics and Gynecology. 2008;198(4):357–366. doi: 10.1016/j.ajog.2007.12.039.
- Zhao R., Wang X., Zou L., et al. Adverse obstetric outcomes in pregnant women with uterine fibroids in China: a multicenter survey involving 112, 403 deliveries. PLoS One. 2017;12. doi: 10.1371/journal.pone.0187821.
- Radhika BH, Naik K, Shreelatha S, Vana H. Case series: Pregnancy Outcome in Patients with Uterine Fibroids. J Clin Diagn Res. 2015 ;9(10):QR01-4. doi: 10.7860/JCDR/2015/14375.6621.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
