By Imran Jariullah1, Muhammad Ghayassudin 1, Syeda Alisha Ali2, Muhammad Ali1, Wahb Noor Zia1, Afshan Nafees1, Ramsha Waseem1, Khadijah Abid3
- Surgery Department, Kulsum Bai Valika Social Security Site Hospital, Karachi, Pakistan
- Neurosurgery Department, Aga Khan University Hospital, Karachi, Pakistan
- Public Health Department, SZABIST University, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD12-4/007
How to cite: Jariullah I, Ghayassudin M, Ali SA, Ali M, Zia WN, Nafees A, Waseem R, Abid K. Role of Injection Lidocaine with and without Triamcinolone Acetonide in the Management of Chronic Pain in Post-Operative Inguinal Hernioplasty. Pak J Med Dent. 2023;12(4): 32-36. Doi: 10.36283/PJMD12-4/007
Background: Inguinal hernioplasty, also called Lichtenstein repair, is a common surgical procedure for inguinal hernia which can lead to chronic groin pain. Local anesthetic blocks combined with corticosteroids like lidocaine and triamcinolone have been used for post-operative pain management. This study aimed to compare the efficacy of lidocaine with triamcinolone acetonide versus lidocaine alone for chronic pain management in patients who underwent inguinal hernioplasty.
Methods: A randomized control trial study was conducted at the Department of Surgery, Kulsoom Bai Valika Hospital, Karachi, Pakistan, from June 2022 to June 2023. The study included patients undergoing inguinal hernioplasty who were over 18 years of age. Group 1 (n=75) received a combination of lidocaine with triamcinolone acetonide, while group 2 (n=75) received lidocaine alone. Pain levels were assessed using the visual analog scale (VAS) during 1st week, 1st month, and 3rd month after the surgery.
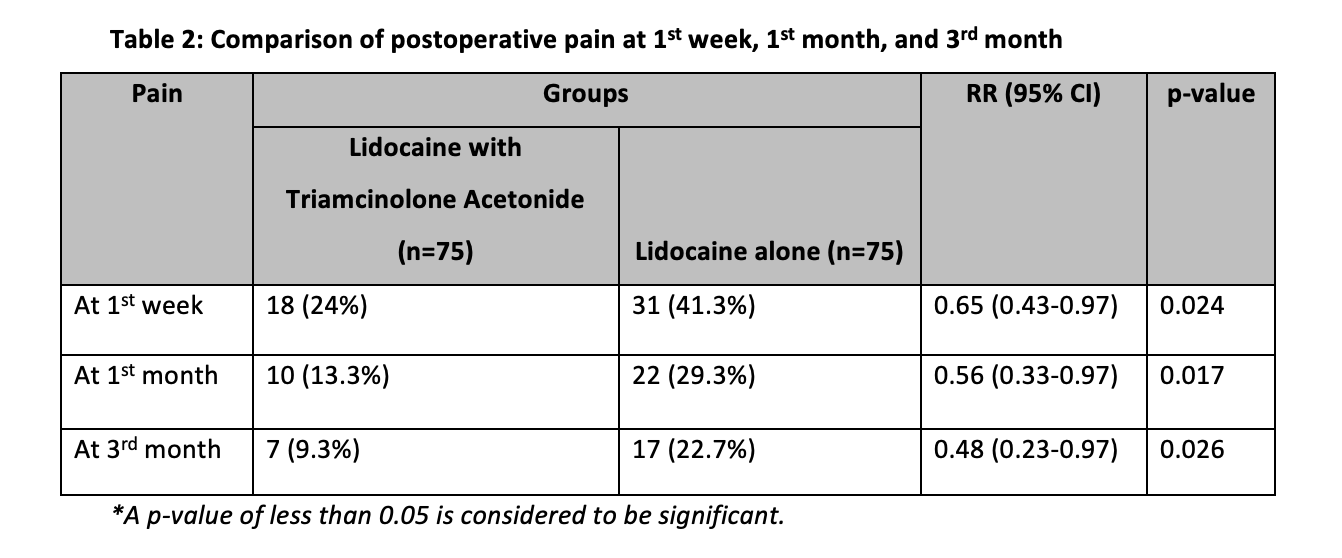
Results: In group 1, the incidence of pain in the 1st week was 25%, significantly lower than the 41.3% in group 2 (p=0.024). The risk ratio (RR) was 0.65 (95% CI=0.43-0.97, p=0.037). In the 1st month, group 1 had a 13.3% incidence of pain compared to 29.3% in group 2 (p=0.017), with an RR of 0.56 (95% CI=0.33-0.97). Similarly, in the 3rd month, group 1 had a 9.3% incidence of pain compared to 22.7% in group 2 (p=0.026), with an RR of 0.48 (95% CI=0.23-0.97).
Conclusion: Lidocaine with triamcinolone acetonide is an effective approach for managing chronic postoperative pain in inguinal hernioplasty.
Keywords: Chronic Pain, Hernioplasty, Local anesthetic, Lidocaine.
Inguinal hernioplasty, also referred to as the Lichtenstein repair, is a widely performed medical procedure in general surgery, with an astonishing global annual volume exceeding 20 million surgeries1. The current standard technique for inguinal hernia repair is tension-free open hernioplasty, commonly known as the Lichtenstein repair2, 3.
This approach has proven effective, resulting in successful outcomes with minimal post-operative complications, shorter recovery periods, and no significant long-term issues2, 4. Nonetheless, amidst its overall success, the development of chronic groin pain, ranging from mild to severe intensity, has emerged as a notable complication following the procedure2, 4.
Although chronic pain following inguinal hernia repair has been thoroughly researched, the treatment remains difficult1, 5, 6. Almost 8% to 16% of patients report chronic pain within six months of hernioplasty, that significantly associated with quality of life7. The use of local anesthetic blocks, such as opioids and non-steroidal anti-inflammatory medications (NSAIDs), as well as other techniques, have historically been used to enhance pain outcomes during inguinal hernioplasty5, 8. These pain medications can give temporary relief but be associated with adverse side effects like nausea, vomiting, sedation, and opioid addiction9.
In recent times, local anesthetic blocks combined with corticosteroids have been used for postoperative pain management in various surgical procedures5, 6, 10, 11. Among the commonly used local anesthetic agents, lidocaine stands out as a potent amide-type anesthetic that has undergone extensive study and widespread application in diverse surgical settings for effective pain relief5, 6, 11. Simultaneously, triamcinolone acetonide, a well-known synthetic corticosteroid, has been employed alongside local anesthetics due to its powerful anti-inflammatory properties, making it a valuable drug in pain management strategies10, 12.
The utilization of lidocaine with triamcinolone for pain management has been investigated in various contexts. Geh et al. reported satisfactory outcomes (80%) and minimal complications (3%) when utilizing this combination therapy for musculoskeletal pain13. Another research by Amjad et al. showed the use of local anesthesia with an injection of triamcinolone acetonide was more efficacious in post-herpetic neuralgia than local anesthesia alone14. Additionally, Emperumal et al. found that intra-articular injections of triamcinolone acetonide alongside lidocaine showed favorable outcomes in terms of temporomandibular joint pain 15. However, research is very limited specifically addressing the application of this combination therapy for post-operative pain management in inguinal hernioplasty. Therefore, the objective current study was to compare the efficacy of lidocaine with triamcinolone acetonide versus lidocaine alone for chronic pain management in patients who underwent inguinal hernioplasty. This study would improve the pain management strategies and patient outcomes in this commonly performed surgical procedure.
This study was a randomized control trial study. The study was conducted at the Department of Surgery of Kulsumbai Valika Social Security Site Hospital, Karachi, Pakistan from June 2022 to June 2023. Patients who unedging for inguinal hernioplasty were recruited for the study. The inclusion criteria were patients of age more than 18 years and of any sex. Patients having a history of hypersensitivity to local anesthetics or steroids, or current systemic corticosteroid therapy, and those with coagulation disorders were excluded from the study. The sample size of 144≈150 (75 patients in each group) was determined based on the proportion of patients having chronic pain post inguinal hernia repair as 16%7, bond on an error as 6%, and 95% confidence level. Open epi online sample size calculator was used for sample size calculation.
The institutional review board (IRB) gave its approval to the study protocol (Ref# 3158). All participants provided informed permission before enrolment and received information regarding the goals, methods, potential hazards, and advantages of the study. Confidentiality of participant data was strictly maintained, and all ethical principles were adhered to throughout the study.
Patients were categorized into two groups based on their exposure. Group 1 included patients who had received 0.5% lidocaine 4ml with 40 mg triamcinolone acetonide in addition to standard care, while group 2 included patients who had received 0.5% lidocaine 4ml alone in addition to standard care. Baseline data regarding age, gender, BMI, and comorbidities were recorded for all patients. After hernioplasty, patients were regularly followed up to observe post-operative pain levels at specific time intervals i.e., 1 week, 1 month, and 3 months. Pain score was assessed using a visual analog scale (VAS) and a pain score equal to or greater than 4 was deemed as positive. All the data was recorded on the pre-designed questionnaire.
Statistical analysis was performed using SPSS version 27. Mean and SD were reported for numeric data like age and BMI. Frequency and percentage were reported for categorical data like gender, comorbid, and post-operative pain at different time points. Comparison between both groups for post-operative pain at 1 week, 1 month, and 3 months was done using the Chi-square test. The risk ratio along with a 95% confidence interval (CI) was also calculated. The significance level was set at p<0.05.
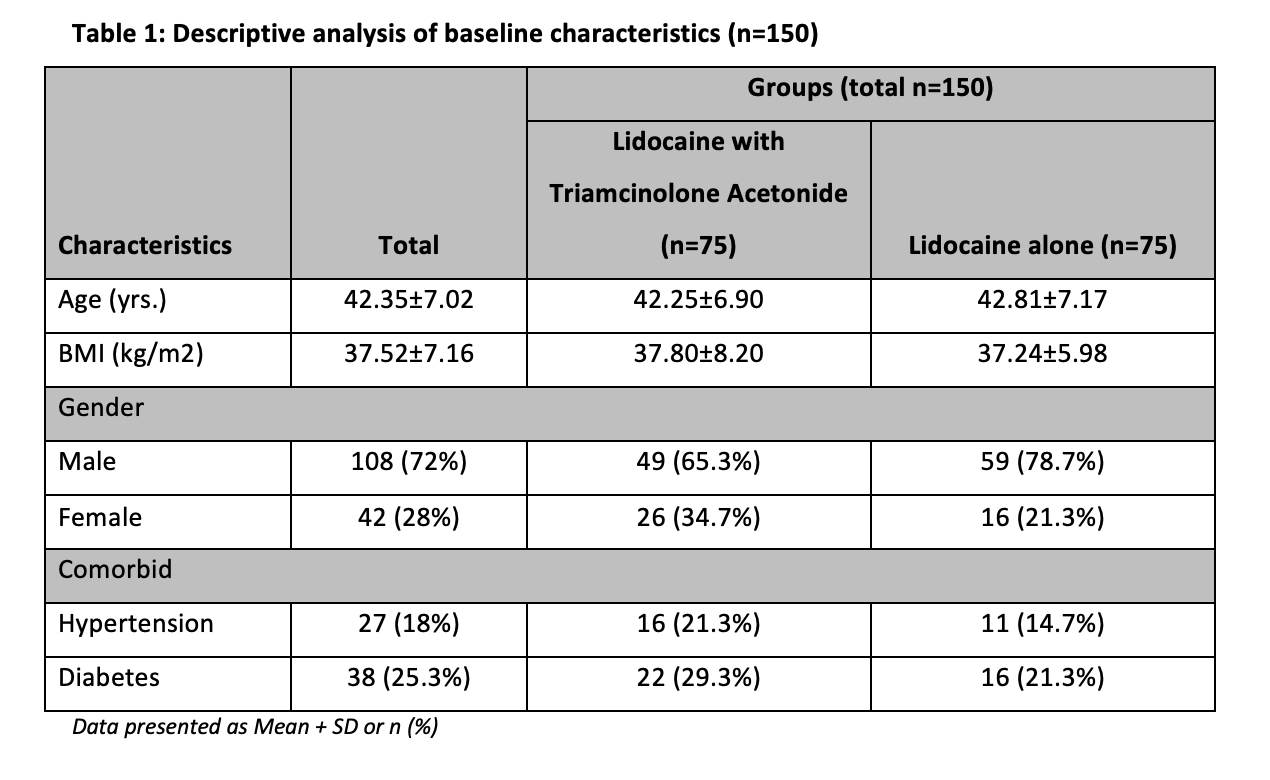
Of 150 patients, the overall mean age (years) was 42.35 + 7.02, and the overall mean BMI was 37.52 + 7.16 kg/m². Out of the total patients, 108 (72%) were male, and 42 (28%) were female. About 38 (25.3%) patients had diabetes and 27 (18%) patients had hypertension. The group-wise distribution of baseline characteristics is displayed in Table 1.
In the 1st week after the procedure, group 1 had a lower incidence of pain compared to group 2 (24% vs 41.3%, p=0.024). The risk ratio (RR) was 0.65 with a 95% confidence interval (CI) of 0.43-0.97, indicating a significant reduction in the risk of pain in group 1 at this time point. Similarly, in the 1st-month post-procedure, group 1 showed a significantly lower incidence of pain compared to group 2 (13.3% vs. 29.3%, p=0.017). The RR was 0.56 with a 95% CI of 0.33-0.97, further confirming the substantial reduction in the risk of pain in group 1 at this time point. Moving on to the 3rd month after the procedure, the trend continued, with group 1 exhibiting a significantly lower incidence of pain compared to group 2 (9.3% vs. 22.7%, p=0.026). The RR was 0.48 with a 95% CI of 0.23-0.97, indicating a substantial decrease in the risk of pain in group 1 at this time point. (Table 2)
Post-operative chronic pain is a significant issue after inguinal hernia repair, affecting 8% to 16% of patients within six months and negatively impacting their quality of life7, 16. To address this, the current study compared the effectiveness of using triamcinolone acetonide along with lidocaine versus lidocaine alone for chronic pain after Lichtenstein repair. Lidocaine, a local anesthetic, blocks nerve signals and provides analgesia, while triamcinolone acetonide, a corticosteroid, reduces inflammation at the surgical site 5, 14, 17, 18. The current study findings showed that patients receiving triamcinolone acetonide with lidocaine experienced significantly lower chronic pain at different time points compared to those who received lidocaine alone, suggesting that this intervention consistently reduced postoperative pain at 1st week, 1st month, and 3rd month. The study’s results indicate the potential benefits of using this combination to improve the post-operative experience for patients undergoing inguinal hernioplasty.
Other studies have also demonstrated the effectiveness of using local anesthesia with steroids to treat different types of pain 10, 19-22. the study by Geh et al. showed successful outcomes in managing musculoskeletal pain in 80% of patients with minimal complications13. Amjad et al. found that combining local anesthesia with triamcinolone acetonide provided superior pain relief for patients with postherpetic neuralgia compared to local anesthesia alone14. Emperumal et al. reported positive results in managing temporomandibular joint pain through intra-articular injections of triamcinolone acetonide alongside lidocaine15.
The study by Verhagen et al. compared a combination of corticosteroids, lidocaine, and hyaluronic acid and a neurectomy over six weeks for the treatment of chronic pain. They found baseline pain score was similar in both groups (p=0.86), however, the success rate of neurectomy was significantly higher than combination therapy (p=0.001) 23. Furthermore, Bahari et al. discovered that combining triamcinolone acetonide with bupivacaine resulted in significantly lower pain scores, reduced opiate requirements in the first 24 hours post-surgery, and shorter inpatient stays after lumbar discectomy, compared to other groups using only one of these agents or a control22. Similarly, Boelens et al. evaluated a diagnostic workup and treatment protocol for chronic abdominal pain caused by suspected anterior cutaneous nerve entrapment syndrome (ACNES). They found that trigger point lidocaine injections with corticosteroids provided significant pain reduction in a majority of patients, and neurectomy was effective for refractory cases21.
The administration of local anesthesia with steroids for the management of pain is not only efficacious but also offers various advantages as compared to traditional pain medications like NSAIDs and opioids 10, 19, 20. While NSAIDs and opioids can temporarily relieve pain, they are significantly associated with various side effects like sedation, vomiting, nausea, and addiction to opioids. In contrast, local anesthesia with steroids acts directly at the pain side, minimizing systemic adverse effects and decreasing the requirement for systemic pain medications10, 19, 20, 24, 25. Furthermore, the use of local anesthesia with steroids can lead to improved post-operative recovery and reduced hospital stay. Effective pain management is closely linked to patient satisfaction and faster recovery, as patients experience less discomfort and are better able to engage in early mobilization and physical activity. The shorter hospital stay can also contribute to cost savings for both patients and healthcare facilities 10, 19, 20, 24, 25.
It is important to recognize some of the study’s shortcomings. Firstly, because just one center was included in the research, it’s possible that the results cannot be applied to other healthcare environments. Second, the study’s sample size was quite small, which might have affected the results’ statistical power. Larger multicenter trials are required to verify the findings and evaluate the efficacy of the intervention in a range of patient demographics.
The combination of lidocaine with triamcinolone acetonide emerges as a robust strategy for effectively managing chronic post-operative pain in patients undergoing inguinal hernioplasty. This strategy presents a meaningful advancement in pain management, demonstrating its potential to lessen pain and improve patient recovery after the surgical procedure.
The authors would like to extend their gratitude to their institute and research committee.
The authors declare no conflict of interest.
Ethical approval was taken from the institutional review board of Kulsumbai Valika Social Security Site Hospital, reference number 3158.
IJ, MA: Conceptualization; Data curation; Formal analysis. MG, SAA, WNZ: Investigation; Methodology. AN: Project administration; Resources. KA: Software; Supervision; Validation. KA, IJ: Visualization; Roles/Writing – original draft. RW, KA: Roles/Writing – original draft; Writing – review & editing. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript
- Sharif A, Akhtar T, Akhtar M, Malik I, Hanif M, Zia N. Effect of Prophylactic Ilioinguinal Neurectomy on Postoperative Groin Pain Following Lichenstein Hernioplasty. J Coll Physicians Surg Pak 2019;29(5):406-409. DOI: 10.29271/jcpsp.2019.05.406.
- Pereira C, Rai R. Open Lichtenstein Hernioplasty Versus Laparoscopic Transabdominal Preperitoneal Mesh Repair: The Pain Factor. Cureus 2021;13(9):e18282. DOI: 10.7759/cureus.18282.
- Ersoz F, Culcu S, Duzkoylu Y, Bektas H, Sari S, Arikan S, et al. The Comparison of Lichtenstein Procedure with and without Mesh-Fixation for Inguinal Hernia Repair. Surgery Research and Practice 2016;2016:8041515. DOI: 10.1155/2016/8041515.
- Salma U, Ahmed I, Ishtiaq S. A comparison of postoperative pain and hospital stay between Lichtenstein’s repair and Laparoscopic Transabdominal Preperitoneal (TAPP) repair of inguinal hernia: A randomized controlled trial. Pak J Med Sci 2015;31(5):1062-1066. DOI: 10.12669/pjms.315.4811.
- Ahn H-m, Oh H-K, Kim D-W, Kang S-B, Koo B-W, Lee P-B. Efficacy and safety of 5% lidocaine patches for postoperative pain management in patients undergoing unilateral inguinal hernia repair: study protocol for a prospective, double-blind, randomized, controlled clinical trial. Trials 2022;23(1):767. DOI: 10.1186/s13063-022-06700-3.
- Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, et al. Local anesthetics and regional anesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev 2018;6(6):Cd007105. DOI: 10.1002/14651858.CD007105.pub4.
- Andresen K, Rosenberg J. Management of chronic pain after hernia repair. J Pain Res 2018;11:675-81. DOI: 10.2147/jpr.S127820.
- Pedroso lm, rm de-m, d. a-silva nj j. comparative study of postoperative pain between the lichtenstein and laparoscopy surgical techniques for the treatment of unilateral primary inguinal hernIA. Arq Bras Cir Dig 2017;30(3):173-176. DOI: 10.1590/0102-6720201700030003.
- Schug S, Collaborators PWG. Pain management after open inguinal hernia repair: an updated systematic review and procedure-specific postoperative pain management (PROSPECT/ESRA) recommendations. Acta Anaesthesiologica Belgica 2020;71:45-56.
- Šimurina T, Mraović B, Župčić M, Graf Župčić S, Vulin M. local anesthetics and steroids: contraindications and complications – clinical update. acta Clin Croat 2019;58(Suppl 1):53-61. DOI: 10.20471/acc.2019.58.s1.08.
- Becker DE, Reed KL. Local anesthetics: review of pharmacological considerations. Anesth Prog 2012;59(2):90-101; quiz 2-3. DOI: 10.2344/0003-3006-59.2.90.
- Morelli Coppola M, Salzillo R, Segreto F, Persichetti P. Triamcinolone acetonide intralesional injection for the treatment of keloid scars: patient selection and perspectives. Clin Cosmet Investig Dermatol 2018;11:387-396. DOI: 10.2147/ccid.S133672.
- González EHH, Sosa GP, Betancourt GM. Evaluation of the treatment with triamcinolone acetonide plus lidocaine for musculoskeletal pain in orthopedics. Revista Archivo Médico de Camagüey 2013;17(5):558-571.
- amjad m, mashhood aa. acetonide with lignocaine compared with lignocaine alone in the treatment of postherpetic neuralgia. JCPSP 2005;15(11):683-685.
- Chitra Priya Emperumal YA, Mariela Padilla, Reyes Enciso, Glenn T. Clark. Efficacy of Intra-Articular Injection of Corticosteroids Combined with Local Anesthetics in the Management of Temporomandibular Joint Pain: A Retrospective Study. Archives of Anesthesiolog 2020;3(2):31-41.
- Pedersen KF, Krpata DM, Rosen MJ, Bisgaard T. Laparoscopic treatment of chronic pain following inguinal hernia repair: a narrative review of the literature. Laparoscopic Surgery 2021;5.
- Paik J, Duggan ST, Keam SJ. Triamcinolone Acetonide Extended-Release: A Review in Osteoarthritis Pain of the Knee. Drugs 2019;79(4):455-462. DOI: 10.1007/s40265-019-01083-3.
- Shanthanna H, Busse JW, Thabane L, Paul J, Couban R, Choudhary H, et al. Local anesthetic injections with or without steroid for chronic non-cancer pain: a protocol for a systematic review and meta-analysis of randomized controlled trials. Systematic Reviews 2016;5(1):18. DOI: 10.1186/s13643-016-0190-z.
- Shanthanna H, Busse JW, Thabane L, Paul J, Couban R, Choudhary H, et al. Local anesthetic injections with or without steroid for chronic non-cancer pain: a protocol for a systematic review and meta-analysis of randomized controlled trials. Syst Rev 2016;5:18. DOI: 10.1186/s13643-016-0190-z.
- Shanthanna H, Busse J, Wang L, Kaushal A, Harsha P, Suzumura EA, et al. Addition of corticosteroids to local anaesthetics for chronic non-cancer pain injections: a systematic review and meta-analysis of randomised controlled trials. British Journal of Anaesthesia 2020;125(5):779-801. DOI: https://doi.org/10.1016/j.bja.2020.06.062.
- Boelens OB, Scheltinga MR, Houterman S, Roumen RM. Management of anterior cutaneous nerve entrapment syndrome in a cohort of 139 patients. Ann Surg 2011;254(6):1054-1058. DOI: 10.1097/SLA.0b013e31822d78b8.
- Bahari S, El-Dahab M, Cleary M, Sparkes J. Efficacy of triamcinolone acetonide and bupivacaine for pain after lumbar discectomy. Eur Spine J 2010;19(7):1099-1103. DOI: 10.1007/s00586-010-1360-7.
- Verhagen T, Loos MJA, Scheltinga MRM, Roumen RMH. The GroinPain Trial: A Randomized Controlled Trial of Injection Therapy Versus Neurectomy for Postherniorraphy Inguinal Neuralgia. Ann Surg 2018;267(5):841-845. DOI: 10.1097/sla.0000000000002274.
- Abdolrazaghnejad A, Banaie M, Tavakoli N, Safdari M, Rajabpour-Sanati A. Pain Management in the Emergency Department: a Review Article on Options and Methods. Adv J Emerg Med 2018;2(4):e45. DOI: 10.22114/AJEM.v0i0.93.
- Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC clinical practice guideline for prescribing opioids for pain—United States, 2022. MMWR Recommendations and Reports 2022;71(3):1.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
