By Hiba Siddiqui1, Tuba Laiq1, Shabbir Hussain1, Amna Qadri2
- Oncology Department, Ziauddin University Hospital, Karachi, Pakistan
- Histopathology Department, Ziauddin University Hospital Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD12-4/017
How to cite: Siddiqui H, Laiq T, Hussain S, Qadri A. Primary Pancreatic Lymphoma: A Rare Clinical Entity. Pak J Med Dent. 2023;12(4): 90-93. doi: 10.36283/PJMD12-4/017
Pancreatic adenocarcinoma is one of the most aggressive malignant diseases, rarely, pancreatic lymphomas are diagnosed. The final diagnosis of primary pancreatic lymphoma demands histopathology of the lesion; however, radiological features and tumor markers can help to give an idea about the disease. The most important difference between primary pancreatic lymphomas and pancreatic adenocarcinoma is the different treatment modalities the response to treatment and finally good prognosis in primary pancreatic lymphoma cases. Clinically it is difficult to differentiate the symptoms of primary pancreatic lymphomas from other carcinomas of the pancreas. Rarely patients may experience B- symptoms of lymphomas that are night sweats and fever in the case of primary pancreatic lymphomas.
Keywords: Pancreas, Lymphoma, Adenocarcinoma, Prognosis.
Pancreatic cancers are mostly considered an aggressive disease with poor prognosis. Most of the time, patient experiences symptoms when the disease becomes locally advanced or with distant metastasis. As a result, which mortality rate in the case of pancreatic neoplasms is getting high across the globe1. About 97.8% of pancreatic cancer cases in Pakistan have led to mortality according to Statistics 2. Unfortunately, there is not a single standard investigation for screening patients who are at high risk of pancreatic cancer3.
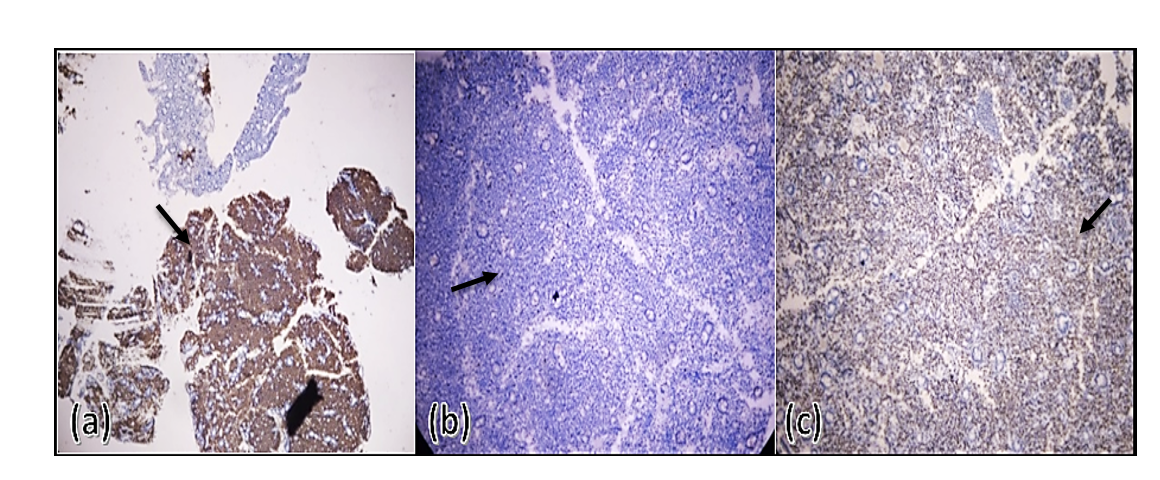
The diagnosis of primary pancreatic lymphoma is based on histopathology and immunohistochemistry like CD20, CD3, CD15, CD10, BCL2, and BCL6. The most common histopathology of pancreatic malignancy is adenocarcinoma4. Although primary pancreatic lymphoma is very rare. The commonest histopathology of primary pancreatic lymphoma (PPL) is Non-Hodgkin’s Lymphoma5. PPL represents only 0.1% of malignant lymphomas, 0.6% of extra nodal lymphomas, and 0.2% of all pancreatic tumors6. Diffuse large B cell lymphoma (DLBCL) is the most common type of non-Hodgkin lymphoma globally, representing approximately 30–40% of all cases in different geographic regions7. Most of the time, this entity is misdiagnosed as another clinical carcinoma of the pancreas. However, the prognosis of PPL is very good.
CASE PRESENTATION
Here we report a case of a 50-year-old male patient with no known co-morbid who presented to the Emergency department of Dr. Ziauddin Hospital on 20th November 2021 with complaints of severe epigastric pain for 15 days, nausea and vomiting for 1 week and decreased appetite 5 days. The examination was done and showed yellow discoloration of the sclera and there was a hard, tender, and irregular mass in the epigastric region, which measured approximately 10 x 12 cm, while the remaining of the examination was unremarkable. Baseline investigations were done which showed ESR of > 100 mm/hr., total bilirubin of 2.06 mg/dl out of which direct bilirubin was 1.59 mg/dl, alkaline phosphatase was 228 U/L, SGPT of 97 U/L, SGOT of 49 U/L, GGT 275 IU/L, serum lipase 88 U/L, serum amylase 25 IU/L. Tumor markers were also done including CA-19-9, CEA, and AFP which were all within normal limits. An ultrasound abdomen was later done which showed a hypoechoic and swollen body of the pancreas. The patient was priorly admitted to a tertiary care setup about 20 days back for the same complaints and a contrast-enhanced CT scan of the abdomen was done which revealed a large heterogeneously enhancing mass in the retroperitoneum with its epicenter at the level of renal vessels and its measured 10.9 x 7.5x 8.5 cm. It was encasing the superior mesenteric artery; the proximal part of the right renal vein, the confluence of the superior mesenteric and splenic veins, as well as the proximal portal vein with its mild narrowing. It was also partially encasing the inferior vena cava and the abdominal aorta. It was also encasing the common bile duct causing its narrowing; it was also inseparable from the third part of the duodenum. Multiple enlarged lymph nodes were also reported along the coeliac axis, gastrohepatic region, peripancreatic region, and retroperitoneum. ERCP (Endoscopic retrograde cholangiopancreatography) was done on 16th November 2021, which showed a stricture at the mid and distal common bile duct (CBD), so a metallic CBD stent was placed, but biopsies were not taken.
The patient was admitted again to our hospital under the care of the Gastroenterology team for the above-mentioned complaints and symptomatic treatment was started. The Oncology team was taken on board and was advised for an upper GI endoscopy with biopsy for histopathology. Endoscopy was done on 23rd November 2021 and showed large growth at the ampulla with CBD stent in place, Scope was passed beyond growth in the duodenum and biopsies were taken. Histopathology revealed an ampullary region lesion suggestive of Diffuse Large B-cell lymphoma (DLBCL). Immunohistochemical staining showed CD20 diffuse positive in sheets of large cells, CD3 negative in sheets of large cells and patchy positive in T-lymphocytes, CD10 dim positive in sheets of large cells and BCL-6 was diffusely positive in sheets of large cells. Ki-67 was positive in up to 80-90% of large cells and Mum-1 was negative in large cells. TdT was negative and CKAE1/AE3 was positive in epithelial cells but negative in tumor cells. The patient was having severe symptoms of sub-acute obstruction and he had a nasogastric tube passed through which he was having continuous gastric contents aspiration. Due to his bad general condition, the patient’s disease with its prognosis was discussed with the family, and with the family’s consent, he was started with definitive radiotherapy keeping in mind locally advanced pancreatic adenocarcinoma but later it was reported as having DLBCL of the pancreas. Radiotherapy also is one of the treatment options of DLBCL so it was continued and completed as per lymphoma protocols. He was then planned to start with chemo-immunotherapy with R-CHOP protocol (Rituximab-Cyclophosphamide, Doxorubicin, Vincristine, and Prednisolone). The patient responded very well. Clinically patient’s performance status improved after 2 cycles of R-CHOP. Unfortunately, after 2 cycles of R-CHOP, the patient caught a COVID-19 infection and expired due to respiratory failure.
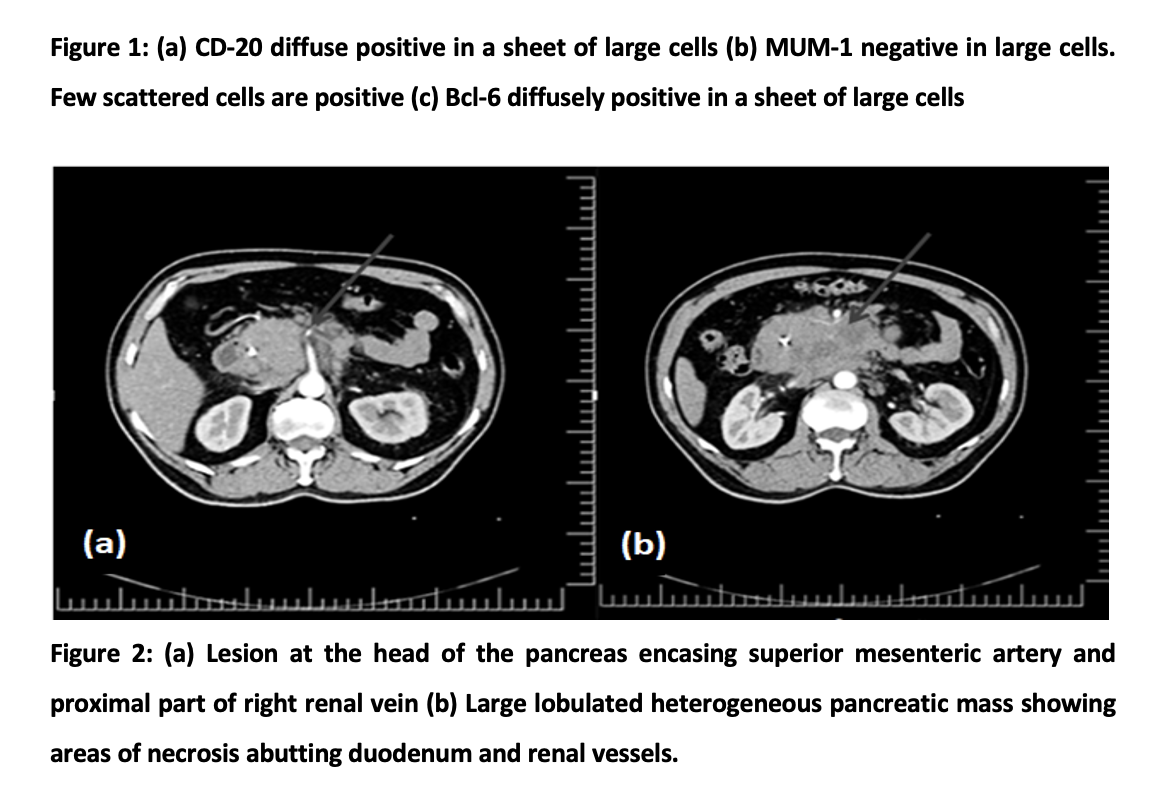
Primary pancreatic lymphoma (PPL) is an exceptionally rare extranodal type of lymphoma that originates from the pancreas. This rarity poses several diagnostic challenges, as symptoms of PPL may mimic those of more prevalent pancreatic diseases, such as pancreatic adenocarcinoma or pancreatitis. PPL may present with symptoms of acute pancreatitis8. Clinically it is difficult to differentiate the symptoms of PPL from other carcinomas of the pancreas. To diagnose PPL, a combination of imaging studies, tissue sampling through biopsy, and immunohistochemistry are typically employed. Computed tomography (CT) scans and magnetic resonance imaging (MRI) are commonly used imaging modalities to study the extent of the tumor. Rarely a patient may experience night sweats and fever in the case of PPL. Certain studies suggest that pancreatic lymphomas show certain imaging features which may help to diagnose and differentiate it from pancreatic adenocarcinoma, but for definite diagnosis histopathology is mandatory9. Some of the features that are absent in pancreatic lymphomas while present in pancreatic adenocarcinoma are pancreatic duct dilatation, bile duct dilatation, and peripancreatic vascular invasion. Enlarged retroperitoneal lymph node below the renal vein has been observed in pancreatic lymphoma more as compared to pancreatic adenocarcinoma10. Furthermore, a diffuse enlargement pattern, infiltrating or replacing the majority of the pancreatic gland points more toward lymphomatous disease rather than carcinoma5.
The definitive diagnosis of PPL is based on tissue samples obtained from the pancreatic lesion through fine-needle aspiration or core biopsy. Although immunohistochemistry helps to identify specific markers on the lymphoma cells, aiding in distinguishing PPL from other types of pancreatic tumors. There are no specific biochemical markers for PPL, but according to some studies, an elevated serum LDH and β2-microglobulin have an important diagnostic and prognostic value in pancreatic lymphoma11. The tumor marker CA19-9 elevation is mostly suggestive of pancreatic adenocarcinoma9. Sometimes in the case of PPL CA19-9 can be elevated if a biliary obstruction is present11. In our case, the CA 19-9 level was within normal range along with radiological proven biliary obstruction.
We report here a rare case of Primary Pancreatic Lymphoma (PPL) in a 50-year-old male who was initially thought of as having pancreatic adenocarcinoma. PPL is not very common, but still, one should keep in mind the differential diagnosis of pancreatic masses with low CA-19-9. The final diagnosis of primary pancreatic lymphoma demands histopathology of the lesion; however, radiological features and tumor markers can help to give an idea about the disease. The most important difference between PPL and Pancreatic adenocarcinoma is the different treatment modalities the response to treatment and finally good prognosis in PPL cases. The patient presented in this case report gives the reader an idea about the diagnosis of these cases with pancreatic masses. Furthermore, the tumor marker CA-19-9 should be considered one of the important tools to diagnose PPL if a patient present without biliary obstruction, and the other important feature is the imaging features as seen on CT scans.
The authors would like to acknowledge hospital staff and doctors for their immense contribution.
The authors declare no conflict of interest.
The consent of the patient was taken before writing the case report.
All authors contributed equally to this case report write-up.
- Zhu H, Li T, Du Y, Li M. Pancreatic cancer: challenges and opportunities. BMC medicine. 2018;16(1):1-3. DOI: https://doi.org/10.1186/s12916-018-1215-3
- Ali SM, Adnan Y, Ali SA. Pancreatic Cancers: A Review of Studies from Pakistan and Comparison with Global Trends. Pakistan Journal of Public Health. 2021;11(2):120-127. DOI: https://doi.org/10.32413/pjph.v11i2.741
- Kamisawa T, Wood LD, Itoi T, Takaori K. Pancreatic cancer. The Lancet. 2016;388(10039):73-85. DOI: 1016/S0140-6736(16)00141-0
- Adamska A, Domenichini A, Falasca M. Pancreatic ductal adenocarcinoma: current and evolving therapies. International journal of molecular sciences. 2017;18(7):1338. DOI 3390/ijms18071338
- Baysal B, Kayar Y, İnce AT, Arıcı S, Türkmen İ, Şentürk H. Primary pancreatic lymphoma: a rare cause of pancreatic mass. Oncology Letters. 2015;10(3):1701-1703. DOI 3892/ol.2015.3412
- Facchinelli D, Boninsegna E, Visco C, Tecchio C. Primary pancreatic lymphoma: recommendations for diagnosis and management. Journal of Blood Medicine. 2021; 12:257. DOI: 2147/JBM.S273095
- Li S, Young KH, Medeiros LJ. Diffuse large B-cell lymphoma. Pathology. 2018;50(1):74-87. DOI: 1016/j.pathol.2017.09.006
- Shnitser A, Halegoua-DeMarzio D, Loren DE. Primary pancreatic lymphoma presents as acute pancreatitis. Gastroenterology & Hepatology. 2016;12(7):456-458.
- Anand D, Lall C, Bhosale P, Ganeshan D, Qayyum A. Current update on primary pancreatic lymphoma. Abdominal Radiology. 2016;41(2):347-355. DOI: 1007/s00261-015-0620-8
- Huang Z, Li M, He D, Wei Y, Yu H, Wang Y, Yuan F, Song B. Two-dimensional texture analysis based on CT images to differentiate pancreatic lymphoma and pancreatic adenocarcinoma: a preliminary study. Academic radiology. 2019;26(8): e189-195. DOI: 1016/j.acra.2018.07.021
- He H, Tan F, Xue Q, Liu L, Peng Y, Bai G, Zhang M, Gao S. Clinicopathological characteristics and prognostic factors of primary pulmonary lymphoma. Journal of Thoracic Disease. 2021;13(2):1106-1117. doi: 10.21037/jtd-20-3159.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
