By Hira Shaikh1, Shafqat Ali Shaikh2, Bushra Ayub3, Arfa Badar3
- Public Health Department, Dow University of Health Science, Karachi, Pakistan
- Otolaryngology and Head & Neck Surgery Department, Patel Hospital, Karachi, Pakistan
- Learning Research Centre, Patel Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD12-4/008
How to cite: Shaikh H, Shaikh SA, Ayub B, Badar A. Poor Oral Health Care Practices by Diabetic Patients. Pak J Med Dent. 2023;12(4): 37-44. Doi: 10.36283/PJMD12-4/008
Background: Sustained poor hyperglycemic control is devastating to oral mucosa that needs top-notch care of oral health. The study aimed to assess the strength of knowledge, attitude, and practices of oral health in diabetic patients, and its associated demographic factors.
Methods: This study was carried out on diabetic patients who came into the Endocrine OPD of Patel Hospital in Karachi. The study was conducted on 363 patients for more than a year. Genders with age greater than 18 years and had at least one natural tooth, were included. The study was analyzed by SPSS software version 21, applying the Mann-Whitney U Test and the Kruskal-Wallis test for categorical variables and mean scores for knowledge, attitude, and practices.
Results: In our study, 64.2% were females with a median age of 56 years. The education level was 20.7%, 23.7%, 19.8%, and 37.5% tertiary, secondary, primary, and formal, respectively. The socioeconomic status was 21%, 57%, and 22%, were belonging to low, middle, and upper, respectively. The age of participants was found weak but positively correlated with knowledge (r= −0.108, p =0.040*) and negatively correlated with attitude (r= -0.004, p= 0.946. Employment status and anti-diabetic therapy had an insignificant association with knowledge, attitude, and practices regarding oral health in diabetic patients (p > 0.05).
Conclusion: The diabetic patients had adequate knowledge regarding oral health but poor attitudes and practices. They are at risk of developing oral health complications; however, it is the responsibility of physicians and dental health professionals to counsel them.
Keywords: Diabetes Mellitus, Knowledge, Oral Health.
Diabetes is a chronic endocrinological disorder that results from long-term poor glycemic control1. Universally since 1980 it expanding from 4.7% to 9 %2 with an overall prevalence rate in Pakistan was 26.3% in 2016-20173. Pakistan ranked as 3rd highest proportion of diabetic patients worldwide4. World Health Organization (WHO) estimated that, by 2030, diabetes would be the seventh chief reason of death5. Persistent reduced hyperglycemic control can harm almost all tissues in the body6. It is associated with macro and microvascular complications in different tissues and affects oral health7. Several studies have re-counted that diabetic patients are at a greater risk for oral health problems, such as dental caries, gingivitis, periodontitis, tooth loss, delayed mucosal wound healing, mucosal neuro-sensory disorders, oral candidiasis as equaled to non-diabetes8. Destruction of periodontal tissue seen in diabetes due to exaggerated inflammatory response after AGE–RAGE (Receptor for AGE) interaction9.
Currently, it is believed that there is a bidirectional relationship between oral health issues and Diabetes Mellitus10. Despite the bidirectional link between diabetes and periodontal disease, researchers from several countries report that diabetic patients often have a low level of oral health knowledge, awareness, and compliance with good oral health behaviors11, most of the patients were unaware of the serious oral health complications of their disease and the need for proper preventive care8. There are no clear or specific guidelines for oral health care among diabetic patients12.
Bowyer et al. stated that, in the UK, 69.1% of diabetic patients had never received any oral health advice related to their disease 11. Sinduja Palati et al., described in their study that only 29.13% had any knowledge about oral lesions while the rest had no knowledge and considered these lesions to be normal changes with increasing age 13. Diabetic patients and their families need to be taught how to practice new skills of lifestyle, including early diagnosis, glycemic control, following medication instructions, physical activity, having a proper diet, and more important of these skills are controlling diabetes and preventing or delaying its complications14. These patients should be active contributors in the learning process and in setting interactive goals15.
Few studies have been conducted in Pakistan that primarily focus on diabetic patients’ knowledge, attitudes, and practices regarding oral health maintenance. Such data are important to plan public health programs and identify the lacking areas of the disease, so they can be improved by designing patient-tailored diabetes educational interventions in Pakistan. Thus, the study aimed to assess the strength of knowledge, attitude, and practices of oral health in diabetic patients, and its association with demographic factors.
The current study was carried out on diabetic patients who came into the OPD of the Endocrinology department of Patel Hospital in Karachi, Pakistan and visited the hospital from the date 1st March till 1st July 2022. ERC approval has been taken from the institute having ERC# PH/IRB/2022/015.
This was an analytical cross-sectional study, recruiting eligible 363 diabetic patients following the criteria. Those patients who were diagnosed with Type I or Type II Diabetes Mellitus, for more than 1 year, both genders were included with age greater than 18 years and had at least one natural tooth. Those diabetic patients, who were physically or psychologically compromised, were excluded from the study.
The questionnaire aimed to evaluate the knowledge, attitude, and practices of diabetic patients, in addition to demographic variables. In endocrine OPD, all the selected patients were explained about the objective of the research project, that the study was questionnaire-based, the information was kept confidential and ensured that it will not cause any effect on the treatment process and by this study; we can improve the oral health in diabetic patients. Inform and written permission was taken and a questionnaire was filled out according to the reaction of the participant. The confidentiality of the patients was ensured during the filling of the questionnaire. The questionnaire included questions about sociodemographic history, and their diabetic history.
The statistics were analyzed through SPSS, version 21. The confidence interval (CI) was taken as 95%, while a p-value <0.05 was considered significant. Age was summarized with median and IQR. Categorical variables were tabulated with frequencies and percentages. The normality of the data was assessed by the Shapiro-Wilk test. As the statistics were not normally distributed, non-parametric tests were performed. Spearmen’s test was performed for the test of correlation between age and mean scores of knowledge, attitude, and practices. While, Mann Whitney U Test and Kruskal Wallis test were performed between categorical variables (gender, education, socioeconomic status, employment status, co-morbidities, addiction history, type of diabetes, family history of diabetes, diabetic treatment, duration of diabetes) and mean scores of knowledge, attitude, and practices.
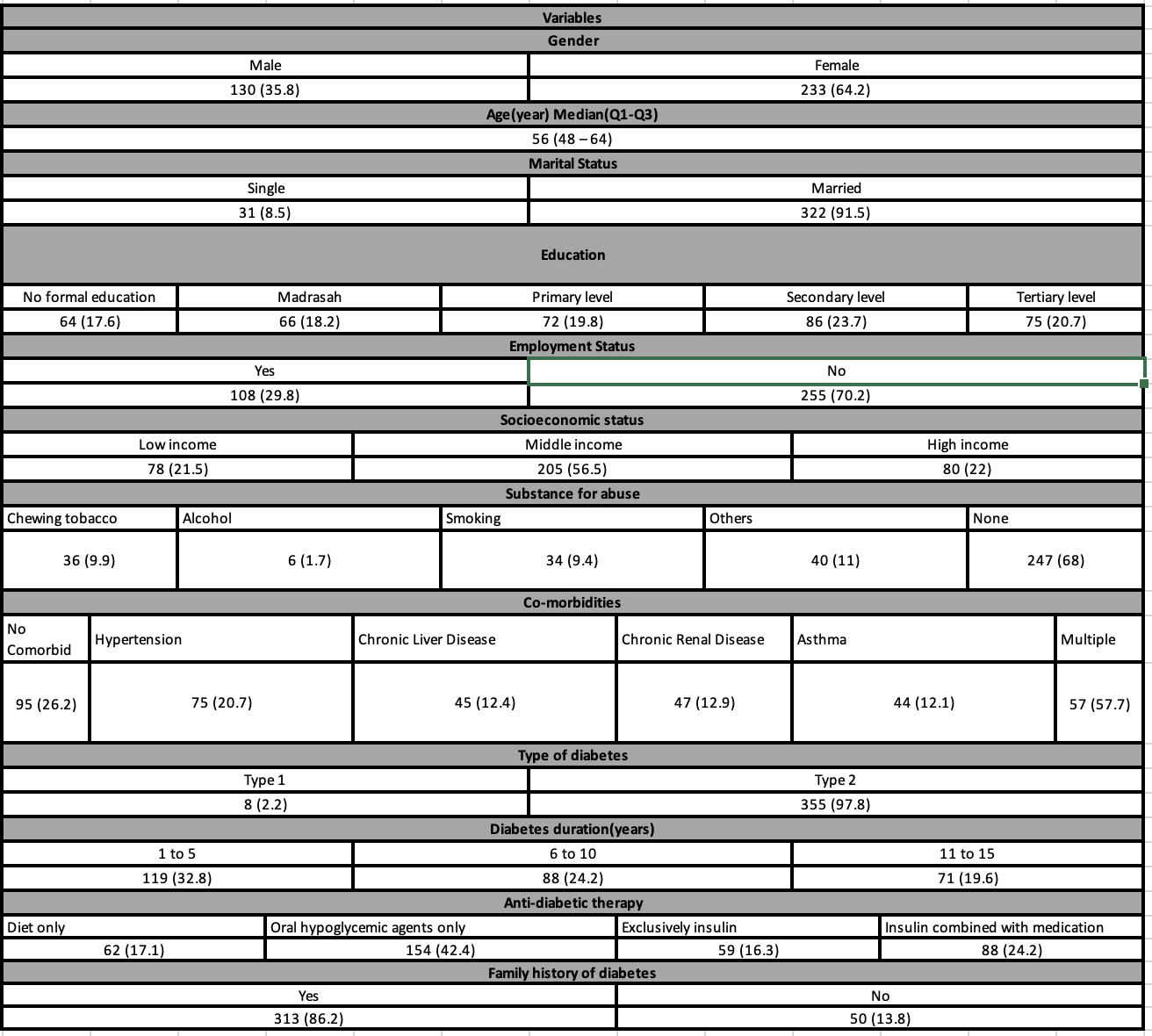
In our study, there were 363 patients included, 64.2% of them were female, with a median age of 56 ranging from 24 to 86 years. Twenty-seven percent of diabetic patients had tertiary education, twenty-three percent had secondary school, nineteen percent had elementary education, and thirty-five percent had no formal education. In terms of socioeconomic status, 21% of patients were classified as having a low socioeconomic position, 56.5% as having a middle socioeconomic status, and 22% as having a higher socioeconomic status. Only 29.9% of diabetic patients had jobs, and 70.2% were jobless.
We examined the medical and diabetes histories of the patients and found that 68% of them had no history of addiction, 9.9% were chewed tobacco users, 9.4% were smokers, and 1.7% were alcoholics. In terms of co-morbidities, 26.2% of the patients had none, 20.7% had hypertension, 12.4% had chronic liver disease, 12.1% had asthma, 12.9% had chronic renal disease, and 15.7% had numerous illnesses. Regarding anti-diabetic therapy, 17.1% of diabetic patients manage their condition solely through diet, 42.4% of diabetic patients take oral hypoglycemic medications, 16.3% of patients only use insulin, and 24.2% use insulin in conjunction with oral hypoglycemic medications and anti-diabetic therapy. In terms of family history, 86.2% of patients had a history of diabetes, whereas 13.8% did not. Every single value as displayed in Table 1
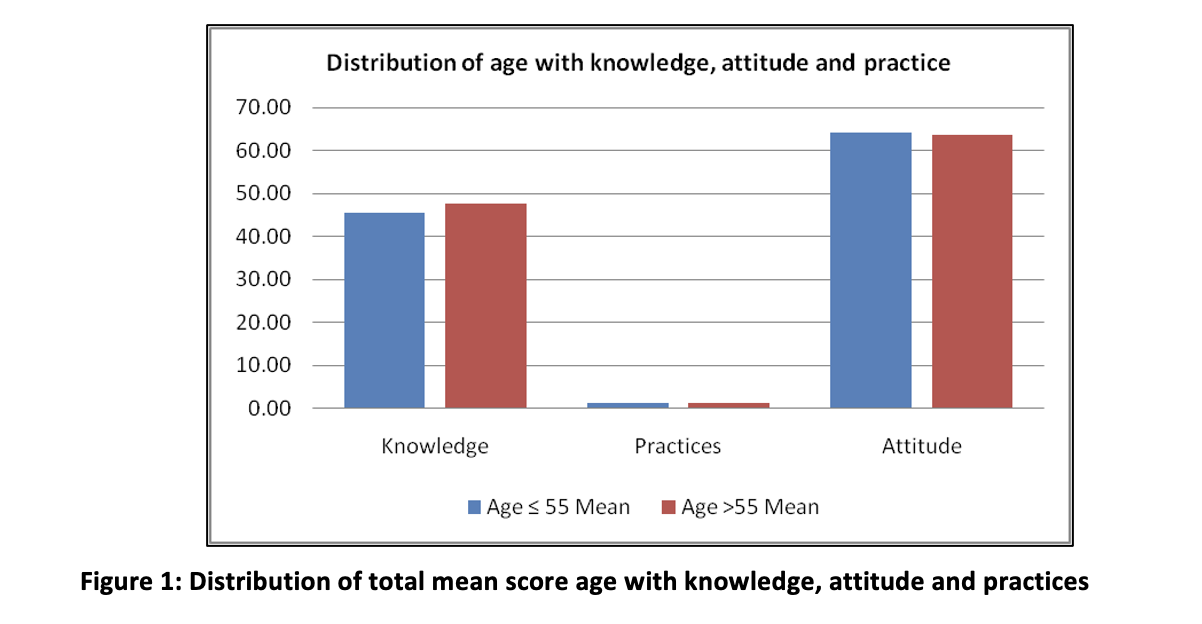
In the age group >55 the total average score of knowledge was 47.71 slightly greater than the age group in ≤55 with a weak and negative correlation with a significant p-value (r = − 0.108, p = 0.040*). Concerning the practices with compare to age groups we have seen same total average score in both groups with a weak and negative correlation with an insignificant p-value (r = -0.005, p = 0.929). Similarly in the age group we have seen that the total mean score was same in both groups with a weak and negative correlation (r = -0.004, p = 0.946) with insignificant p-value, as shown in figure 1.
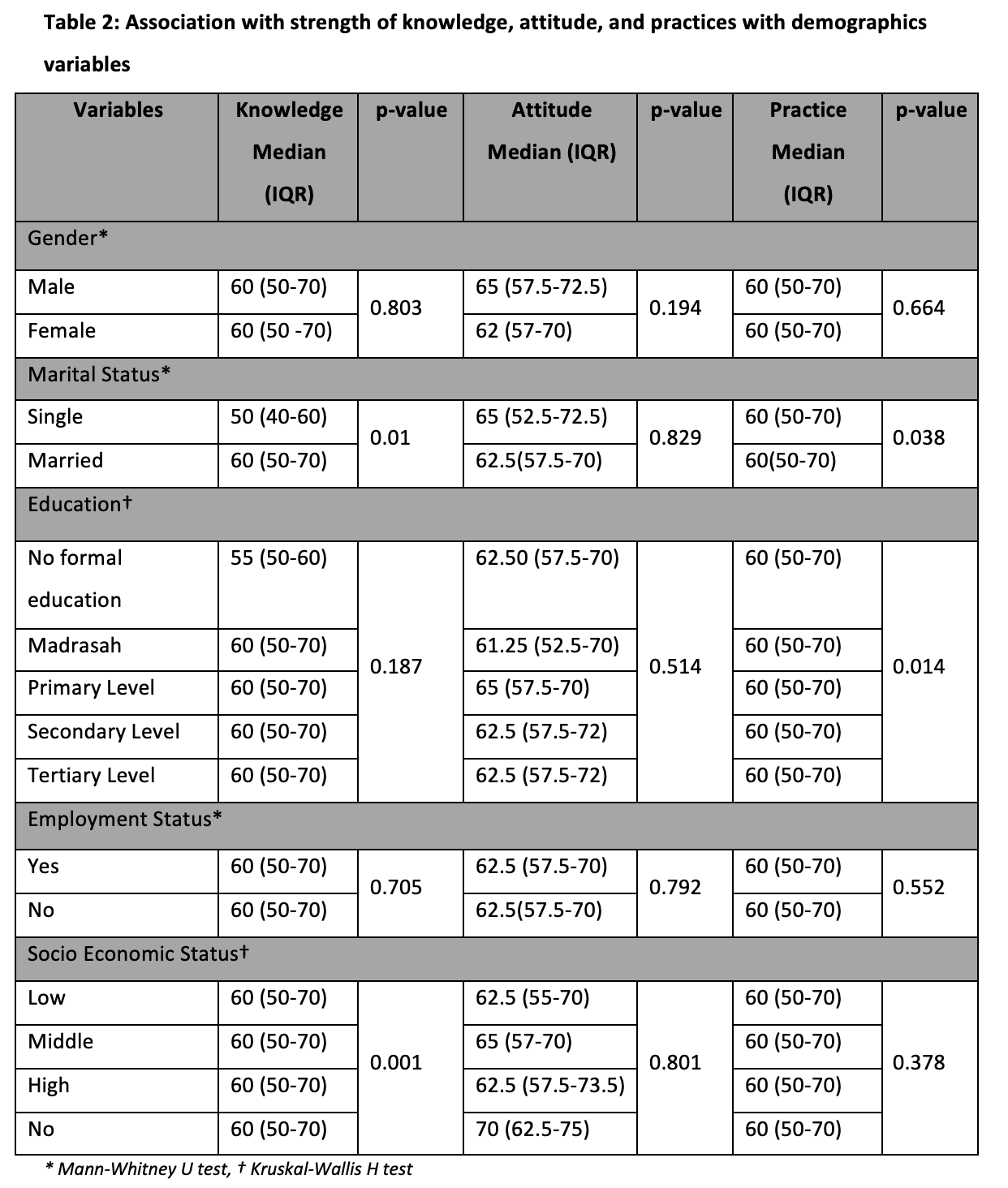
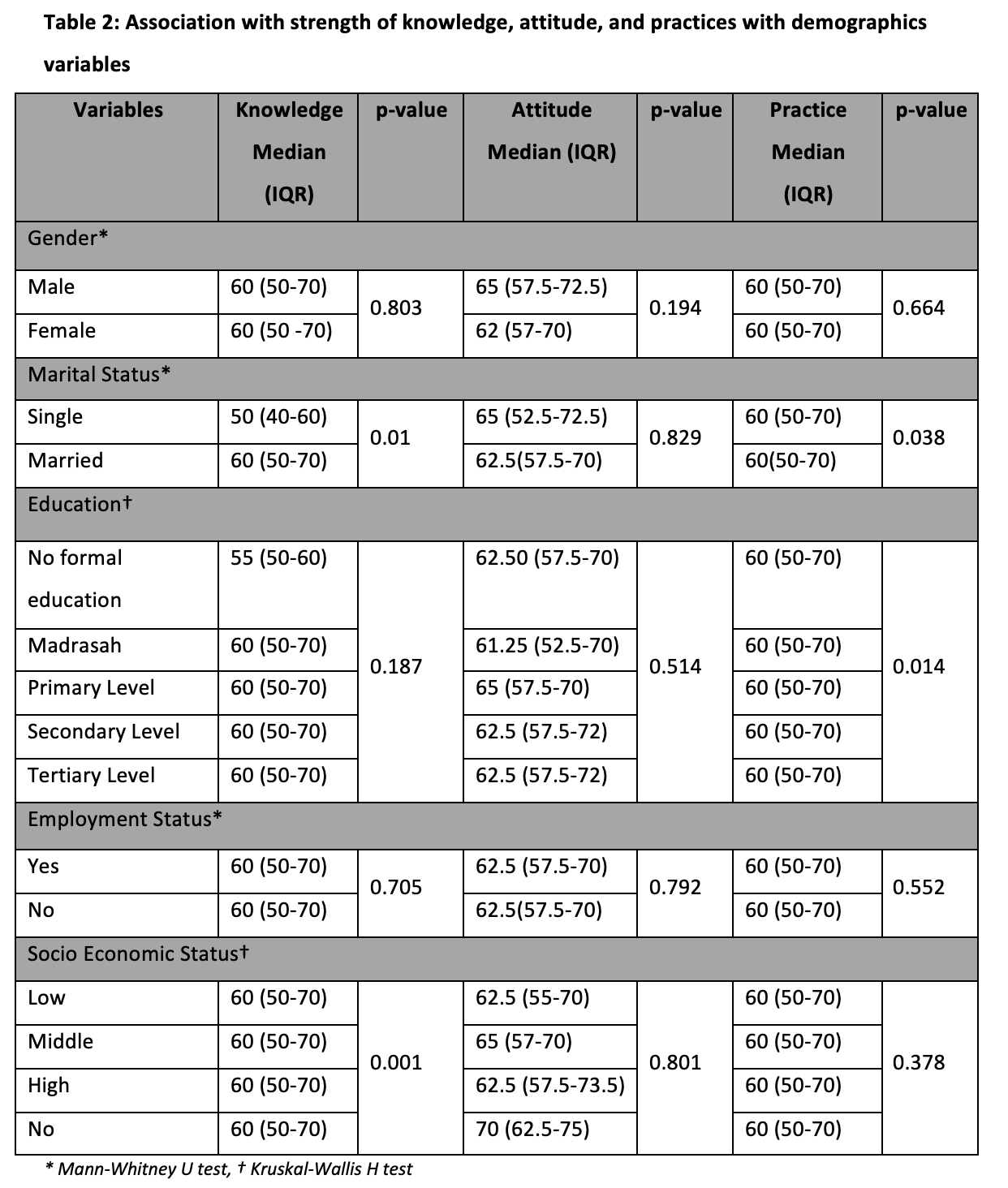
We found no evidence of a significant relationship between knowledge, attitude, and practices for either gender (p > 0.05). Marital status does not significantly affect knowledge or attitude (p>0.05), but it does significantly affect practices (p=0.038), which revealed that married diabetic patients often practice more oral hygiene than unmarried patients. According to our findings, education has a negligible impact on diabetes patients’ oral health knowledge and attitudes (p>0.05), but it has a substantial impact on their practices (p=0.014), demonstrating a more realistic approach to oral health in patients with higher educational attainment. Patients with diabetes who made a middle-class income were better informed and had a significant link with oral health (p=0.001), but there was no correlation with attitudes or behaviors related to oral health (p>0.05). Each and every value as displayed in Table 2.
We have gathered both the clinical and diabetes histories. Co-morbidities were found to have little impact on knowledge and attitude (p>0.05), but a substantial impact on practices (p=0.037), indicating that patients with multiple diseases typically practice better oral health self-care. Smoking was associated with better oral health attitudes among diabetic patients (p=0.046), although these patients were not interested in participating in any procedures, indicating that they generally believed they should take care of their oral health but rarely did. We discovered that patients with type II who had lengthier histories had knowledge that was significantly associated with them (p = 0.05), but not with their attitudes or behaviors (p>0.05). Family history of diabetes had a minor relationship with knowledge and behaviors (p>0.05) but a substantial relationship with attitude (p=0.00013), as shown in Table 3
Table 3: Association with strength of knowledge, attitude, and practices with clinical history
Oral health in Pakistan has always been neglected and given less privilege. Oral health must be given equal importance to general health16. Diabetes is a chronic systemic disease that has a significant impact on oral cavity tissues, which directly influences general health17. In the current study, it was seen that the old age diabetic patients had statistically significant results about knowledge of oral health but the attitude and practices showed statistically insignificant results. Oral health awareness plays a pivotal role in diabetic patients improving their self-care practices18. In our survey, female patients who had diabetes were in greater fraction and the median age was 55 years which is the same as reported by Ismaeil et al.1 We did not see any significant link with respect to gender but contrary to our study, Myriam et al, found that women had a better attitude because they tend to brush more as compared to men19.
In Iran, Razie et al, also reported in their study that old-age diabetic patients had good knowledge20, but contrary to our study the attitude and practices of older age patients with diabetes were also statistically significant in their study. In our survey, we saw that married were more anxious regarding their oral health than those who were unmarried and supported the study of Shaifiur Rehman et al, who reported that married diabetic patients used to practice better oral hygiene to keep their married life healthy21.
Education plays a vital role in one’s daily basis of life. We have seen in our study that, diabetic patients who had tertiary-level education had good practices but did not find an association between knowledge and attitude. On the contrary, we have seen in the study of Prakash Poudel, showed in their study that their patients had more awareness, had sufficient knowledge of oral-related health problems, were more prepared for treatment, and had higher acquiescence to most favorable oral health manners9. In the current study, we have seen that diabetic patients with middle to high socioeconomic status were more knowledgeable about oral health; they had a significant association with oral health, similar to the study with Kh, Shafiur Rehman et al, showed that diabetics with high income were used to get better health education and health facilities for oral health21.
Regarding co-morbidities, we have seen that patients who had systemic diseases other than diabetes revealed a significant association with practices concerning oral health, similar to the study held in Ethiopia by Yimer et al22. Diabetic patients who were smokers had better attitudes toward oral health (p=0.046*) but were not interested in doing any practices, showing these patients usually believed that they must care for it but usually did not. The same result shown in the study conducted by Monera Alhuwais in Kuwait23 reported less than 50% of participating smoker-diabetic patients were unaware of the fact that they have a great chance of developing oral-related health problems. Patients with type II diabetes had better knowledge about oral health than patients with type 1 diabetes, similar results also showed in the study of Afifa Ehsan et al, and that patients suffering from type II diabetes mellitus had ample oral health perception and elevated percentage of oral health semblance24.
Diabetic patient having their family history had a great attitude toward oral health. Similar results were also seen in a survey done by Ghada et al held in Egypt, which revealed that diabetic patients with a positive family history were more knowledgeable about their oral health25. Patients having diabetes for more than 15 years have a sufficient understanding regarding oral health. Still, their good knowledge was not reflected in their attitude and practices, similar to our study related to Shruti et al conducted in India26. They stated that diabetic patients suffered from disease for a long period, they regularly exercised and consulted their physicians on a yearly basis and that reflected they had good overall awareness about diabetes mellitus with respect to oral health.
Good knowledge but poor practices towards oral health in patients with diabetes speculate the community that these patients give less importance to the consequences of bad oral health. The purpose of our survey was to evaluate the strength of knowledge, attitude, and practices among patients having diabetes regarding the link between diabetes and oral health status. Our study aims to assess the role of education of patients with diabetes rather than comparing the differences between them. Overall, the assessment of our survey suggests that in general, most diabetic patients were aware of the consequences on oral health, although, these patients had good knowledge of the risks associated with oral health problems. However, being good oral-related health knowledge, the attitude and practices of most of the involved individuals were unsatisfactory; speculate that these patients gave less importance to the consequences of bad oral health.
It was found that the majority of diabetic patients had an adequate level of knowledge concerning their oral health, by the large, attitudes and practices were not good enough to maintain good oral hygiene. Such adequate knowledge but poor oral hygiene practices reflect that our population is vulnerable to developing oral health complications. Therefore, it is recommended that oral health practitioners, endocrinologists, and general physicians should encourage and create awareness in diabetic patients to maintain proper oral hygiene and continue regular dental visits.
I like to acknowledge hospital staff and doctors for their immense support in data collection.
The authors have no conflict of interest.
The ERC was taken from the Patel Hospital ethical review committee. The acceptance of the ERC no: PH/IRB/2022/015.
HS did the conception, drafting, data collection, data entry, analysis, and final version of drafting in the whole manuscript. SAS did the data collection, drafting, and revision of the final version of the manuscript. BA did the final drafting, data analysis, and interpretation of the results and AB contributed to initial drafting and the planning of the study and data entry.
- Ismaeil FMR, Ali N. Diabetic Patients Knowledge, Attitude and Practice toward Oral Health. Journal of Education and Practice. 2013;4:19-25.
- Zhou B, Lu Y, Hajifathalian K, Bentham J, Di Cesare M, Danaei G, Bixby H, Cowan MJ, Ali MK, Taddei C, Lo WC. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. The lancet. 2016 Apr 9;387(10027):1513-1530.DOI: 10.1016/S0140-6736(16)00618-8
- Basit A, Fawwad A, Qureshi H, Shera AS; NDSP Members. Prevalence of diabetes, pre-diabetes and associated risk factors: second National Diabetes Survey of Pakistan (NDSP), 2016-2017. BMJ Open. 2018 Aug 5;8(8):e020961. doi: 10.1136/bmjopen-2017-020961.
- Azeem S, Khan U, Liaquat A. The increasing rate of diabetes in Pakistan: A silent killer. Ann Med Surg (Lond). 2022 Jun 3;79:103901. doi: 10.1016/j.amsu.2022.103901.
- Kavya G, Reddy MNT, Muthukuru R. Assessment of the Awareness among Diabetic Patients of Their Risk for Oral Disease as Complication Associated With Diabetics.Int Healthc Res J.2018;2(9):217-222. DOI: 10.26440/ihrj.v2i9.179
- Masood Mirza K, Khan AA, Ali MM, Chaudhry S. Oral health knowledge, attitude, and practices and sources of information for diabetic patients in Lahore, Pakistan. Diabetes Care. 2007;30(12):3046-3047. doi: 10.2337/dc07-0502.
- Bangash RY, Khan AU, Manzoor MA. Diabetic patients; level of awareness about oral health knowledge, attitude and practices. Pakistan Oral & Dental Journal. 2011 Dec 1;31(2).
- Al Amassi BY, Al Dakheel RS. Oral hygiene practice of adult diabetic patients and their awareness about oral health problems related to diabetes. Journal of Dentistry and Oral Hygiene. 2017;9(2):8-14. DOI: 10.5897/JDOH2017.0219
- Poudel P, Griffiths R, Arora A, Wong VW, Flack JR, Barker G, et al. Oral health status, knowledge, and behaviours of people with diabetes in Sydney, Australia. 2021;18(7):3464.doi.org/10.3390/ijerph18073464
- AlShwaimi E, Idrees M, Berri Z, El-Sakka H, Kujan O. Association between Diabetes Mellitus and Periodontal Diseases: A Survey of the Opinions of Dental Professionals. Med Princ Pract. 2019;28(2):141-149. doi: 10.1159/000495881.
- owyer V, Sutcliffe P, Ireland R, Lindenmeyer A, Gadsby R, Graveney M, Sturt J, Dale J. Oral health awareness in adult patients with diabetes: a questionnaire study. Br Dent J. 2011 Sep 23;211(6):E12. doi: 10.1038/sj.bdj.2011.769.
- Almeneessier AS, Almunaiseer NS, Alnufaiy BM, Bahammam SO, Alyousefi NA, Batais MA, et al. Assessment of dental health status, knowledge, and practice among Saudi diabetic patients attending general practice Clinic. Journal of Nature and Science of Medicine . 2020;3(4):292.DOI: 10.4103/JNSM.JNSM_64_20
- Palati S, Ramani P, Shrelin HJ, Sukumaran G, Ramasubramanian A, Don KR, Jayaraj G, Santhanam A. Knowledge, Attitude and practice survey on the perspective of oral lesions and dental health in geriatric patients residing in old age homes. Indian J Dent Res. 2020;31(1):22-25. doi: 10.4103/ijdr.IJDR_195_18.
- Awartin FJP. Oral health knowledge and practices in Saudi diabetic female patients. Pakistan Oral and Dental Journal. 2009;29(1):149-152.
- Malekmahmoodi M, Shamsi M, Roozbahani N, Moradzadeh R. A randomized controlled trial of an educational intervention to promote oral and dental health of patients with type 2 diabetes mellitus.BMC Public Health. 2020;20(1):287.doi.org/10.1186/s12889-020-8395-4.
- Singh A, Gambhir RS, Singh S, Kapoor V, Singh J. Oral health: How much do you know? – A study on knowledge, attitude and practices of patients visiting a North Indian dental school. Eur J Dent. 2014;8(1):63-67. doi: 10.4103/1305-7456.126244.
- Alhazmi1 YA, Parveen S, Alfaifi WH, Najmi NM, Namazi SA et al. Assessment of Knowledge, Attitude and Practice of Diabetic Patients towards Oral Health: A Cross-sectional Study. World Journal of Dentistry. 35(45):47. https://doi.org/10.5005/jp-journals-10015-1922
- Bukhsh A, Khan TM, Sarfraz Nawaz M, Sajjad Ahmed H, Chan KG, Goh BH. Association of diabetes knowledge with glycemic control and self-care practices among Pakistani people with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2019 Aug 14;12:1409-1417. doi: 10.2147/DMSO.S209711.
- Saad MA, Saleh SM, EssamEldin WJADJ. Knowledge, attitude, and reported practices of a group of ministry of health dentists towards patients with diabetes mellitus in Alexandria, Egypt. 2019;44(1):24-31.DOI: 10.21608/adjalexu.2019.57572
- Meshki R, Khataminia M, Jokar Z, Veisi MS. Oral health knowledge, attitude and practice among children and adolescents with type 1 diabetes. J Family Med Prim Care. 2022;11(8):4429-4434. doi: 10.4103/jfmpc.jfmpc_1983_21.
- Rahaman KS, Majdzadeh R, Holakouie Naieni K, Raza O. Knowledge, Attitude and Practices (KAP) Regarding Chronic Complications of Diabetes among Patients with Type 2 Diabetes in Dhaka. Int J Endocrinol Metab. 2017;15(3):e12555. doi: 10.5812/ijem.12555.Mekonnen Y, Hussien N. Self-care Related Knowledge, Attitude, and Practice and Associated Factors Among Patients with Type 2 Diabetes in JMC, Ethiopia. Diabetes Metab Syndr
- Obes. 2021;14:535-546. doi: 10.2147/DMSO.S296112.
- Alhuwais M, Alkanderi A, Jospeh B. Attitudes and Awareness of Diabetic Patients in Kuwait Towards Their Oral Health.. Int J Oral Dent Health. 2021;7:133. DOI: 10.23937/2469-5734/1510133
- Ehsan A, Riaz F, Raza A, Sahu EH, Rathore E, Abdullah U, et al. Knowledge and Awareness of Oral Health in Type 2 Diabetes Mellitus Patients Visiting A THQ Hospital in Punjab, Pakistan. Pakistan Journal of Medical and Health Sciences. 2022;16(05):227. doi.org/10.53350/pjmhs22165227
- El-Khawaga G, Abdel-Wahab F. Knowledge, attitudes, practice and compliance of diabetic patients in Dakahlia, Egypt. European Journal of Research in Medical Sciences. 2015;3(1).Vol. 3 No. 1, 2015ISSN 2056-600X
- Shanmukappa SM, Nadig P, Puttannavar R, Ambareen Z, Gowda TM, Mehta DS. Knowledge, Attitude, and Awareness among Diabetic Patients in Davangere about the Association between Diabetes and Periodontal Disease. J Int Soc Prev Community Dent. 2017;7(6):381-388. doi: 10.4103/jispcd.JISPCD_390_17.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
