By Sehar Mudassar1, Usra Naeem1, Ghulam Muhaiyudin 1, Usman Saeed1
- Health Professional Technology Department, The University of Lahore, Pakistan Senior Registrar, Department of Nephrology, Dr. Zia Uddin University Hospital, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD12-4/012
How to cite: Mudassar S, Naeem U, Muhaiyudin G, Saeed U. Frequency and Risk Factors of Surgical Site Infection with and without Antibiotic Prophylaxis in Adults Undergoing Minor Trauma Surgery. Pak J Med Dent. 2023;12(4): 63-68. Doi: 10.36283/PJMD12-4/012
Background: Trauma surgeons are more likely to experience surgical site infections (SSI). Preoperative antibiotic prophylaxis was a common strategy in trauma procedures. This research aimed to determine the frequency and risk factors of surgical site infection with and without antibiotic prophylaxis in adults undergoing minor trauma surgery.
Methods: A descriptive cross-sectional investigation was carried out. The surgical emergency and trauma units at Jinnah Hospital and THQ Hospital DGK provided the data for this investigation. Data from 190 patients were gathered and divided into two groups. Before surgery (Group A) took antibiotic prophylaxis while Group B did not. Standard surgical protocols were followed during the surgical operation. Patients were checked for postoperative fever, surgical site infection, and discharge at the incision site. On the third, seventh, and twelfth postoperative days, the wound was checked. The chi-square test was used for analysis and P<0.05 was considered significant.
Results: Surgical site infections (SSI) occurred in 18 patients out of 190 patients, with 6 (6.3%) patients from group A and 12 (12.6%) from group B. Two (2.1%) of the patients in Group A who developed SSI were female, whereas no female patients in Group B experienced it. Contaminated wounds, diabetes, and improper surgical site cleaning were the three main risk factors for SSI in minor trauma cases.
Conclusion: The study found that the use of prophylactic antibiotics in minor trauma cases performed in adult patients significantly decreases the incidence of SSI.
Keywords: Antibiotic prophylaxis, Surgical site infection, Trauma.
Surgical site infections (SSI) are considered to be a major public health threat to the accomplishment of global surgical procedures, especially in developing countries. Although there is no complete global data, the SSI prevalence in low- and middle-income countries is greater than that in high-income countries (HICs)1. After surgery, the area of the body where the operation was performed becomes infected. SSI frequently manifests 30 days following the operation. Infection at the surgical site is a serious adverse effect of surgical trauma treatment 2. The outcomes are higher mortality, lengthier hospital stays, more revision surgeries, more antibiotic use, and more follow-up and rehabilitation. Redness, slow healing, temperature, pain, tenderness, warmth, and swelling are all signs of an SSI 3.
Accidents and traumatic injuries are among the leading causes of death globally. The tripodal pattern of mortality has typically been used to describe traumatic deaths. Pre-hospital triage, proper patient dispositional reasoning, injury avoidance, and other management strategies are necessary to increase survival rates in the first phase of the pattern, death on the scene Pre-hospital triage, proper patient dispositional reasoning, injury avoidance, and other management strategies are necessary to increase survival rates in the first phase of the pattern, death on scene 4.
Intensive care units (ICUs), emergency rooms, a thorough and accurate primary survey, cardiopulmonary resuscitation (CPR), a follow-up survey, and specialized treatment are all used in the second period of management, death during acute therapy. diseases made worse by one or more Multiple organ failures during the third phase, which arrives later, is frequently a serious concern while getting ICU care or subsequent ward treatment5.
Trauma is viewed as a clean-contaminated medical procedure that carries a risk of surgical site infection in healthy patients without any known risk factors 6. Adult patients presenting for minor trauma surgery are typically in good health, except elderly patients whose surgical problem has minimal systemic consequences. Surgery site infections are more likely to occur in patients who have one or more risk factors, such as diabetes mellitus, immunosuppression, glucocorticoid use, extended hospital stays, etc 7. Trauma patients are believed to have a high risk of infection due to a variety of factors. First of all, trauma events are frequently unpredictable and typically take place in open spaces or on surfaces with a high concentration of contagious microorganisms, such as roads. Second, the soft tissues and skin surfaces that act as a natural defense against infection can sustain serious damage from the mechanical energy that affects the human body during trauma events8. Third, shock and resuscitation may make subsequent inflammatory infections more likely to trigger an immunological reaction. Preventive antibiotic therapy for trauma patients was therefore recommended and has been practiced since 1982, however, the results have been conflicting9. In this study, it was aimed to determine the frequency and risk factors of SSIs with and without antibiotic prophylaxis in adults undergoing minor trauma surgery in a secondary care hospital.
This Cross-sectional descriptive study was conducted under the Department of Health Professional Technology, The University of Lahore from 1st March to 30th July 2022. Data was collected from Jinnah Hospital Lahore and DHQ Hospital Dera Ghazi Khan. Before beginning the study, permission was obtained from the institute’s Ethical Review Board. The sample size was assessed to be 190 and was determined with a 95% confidence level using the WHO sample size calculator. The patients for this study were chosen using a technique called purposive sampling.
Patients were placed into two equal groups of 95 patients each, A and B. The patient’s age, weight, and comorbidities were all documented. Patients in this study ranged in age from 18 to 75 and were scheduled for minor trauma surgery.
The inclusion criteria of the study were patients who contributed to elective surgeries and were 18 years or older. Patients who had not given consent or had bone surgeries or amputations and patients with infected wounds not classified under SSI by classification (local puncture wounds, suture abscesses patients, episiotomy, trauma-related wounds, or infected burn wounds) were excluded from the study. Cephalosporins and a prophylactic dosage of ceftriaxone were administered to group A. Induction of local anesthesia was administered to all subjects. The procedure was carried out using accepted medical procedures and techniques. On the proforma, each patient’s surgical type and duration were recorded. All patients underwent postoperative observation. Patients were checked for postoperative temperature, surgery site infection, and discharge at the incision site. On the third, seventh, and twelfth postoperative days, the wound was inspected. The Centers for Disease Control (CDC) standards were used for SSI labeling. Statistical Package for Social Sciences was used to analyze the data. (IBM-SPSS version 23). The frequency and percentage of demographic data and clinical characteristics of participants were computed while the chi-square test was used to determine significance. P<0.05 was considered significant.
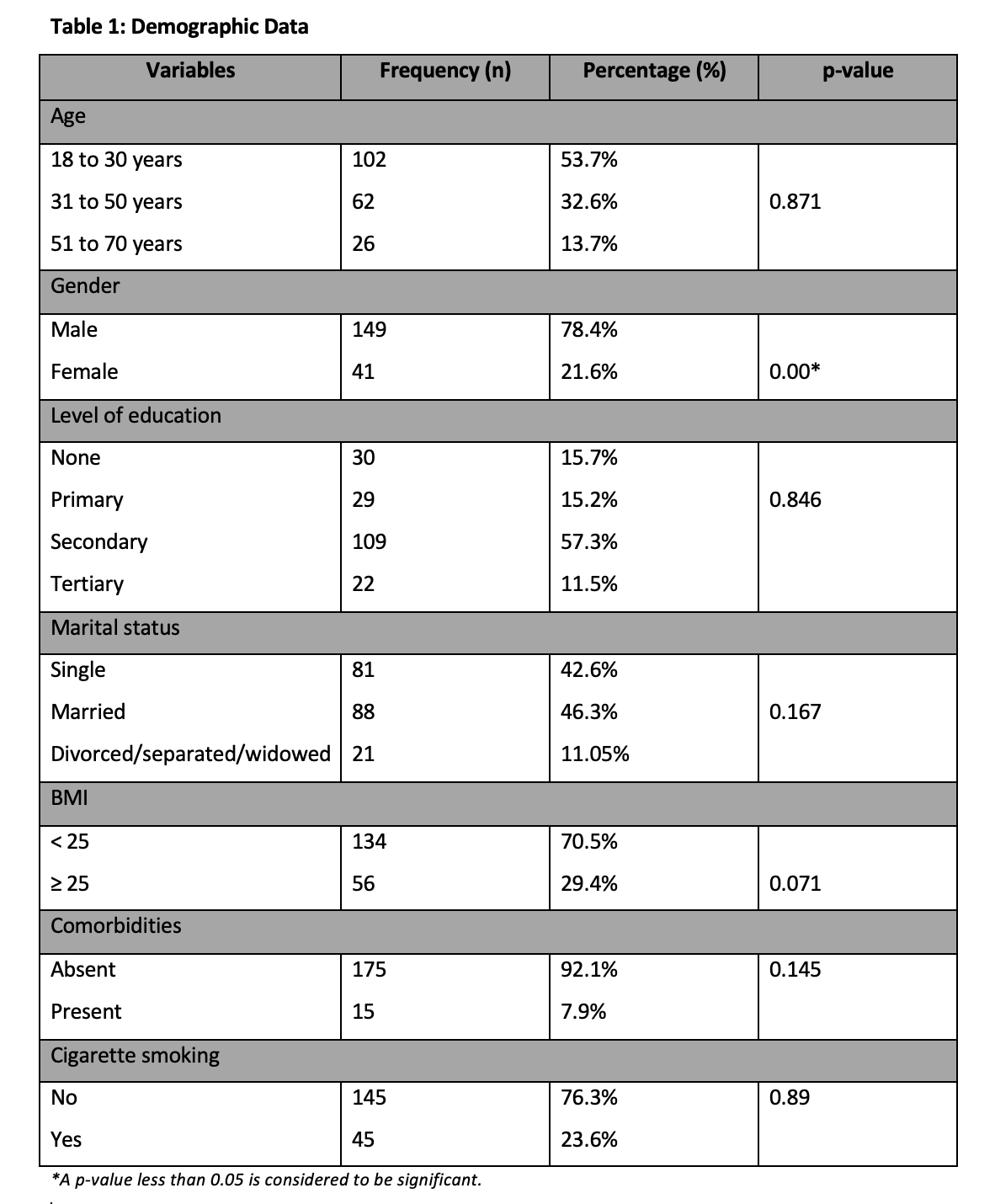
In total 190 patients were chosen for this research study which were further categorized into groups A and B. The individuals who were chosen have an age range from 16 to 70. The majority were males 149 (78.4%), less than 30 years 102 (53.7%), and married 88 (46.3%). The highest educational attainment of the patients was secondary level 109 (57.3%). Most of the patients 134 (70.5%) had a BMI of less than 25 kg/m2 and comorbidities were present in 15 (7.9%). 45(23.6%) patients were smoker and 145(76.3%) were non-smoker. Details are shown in Table 1.
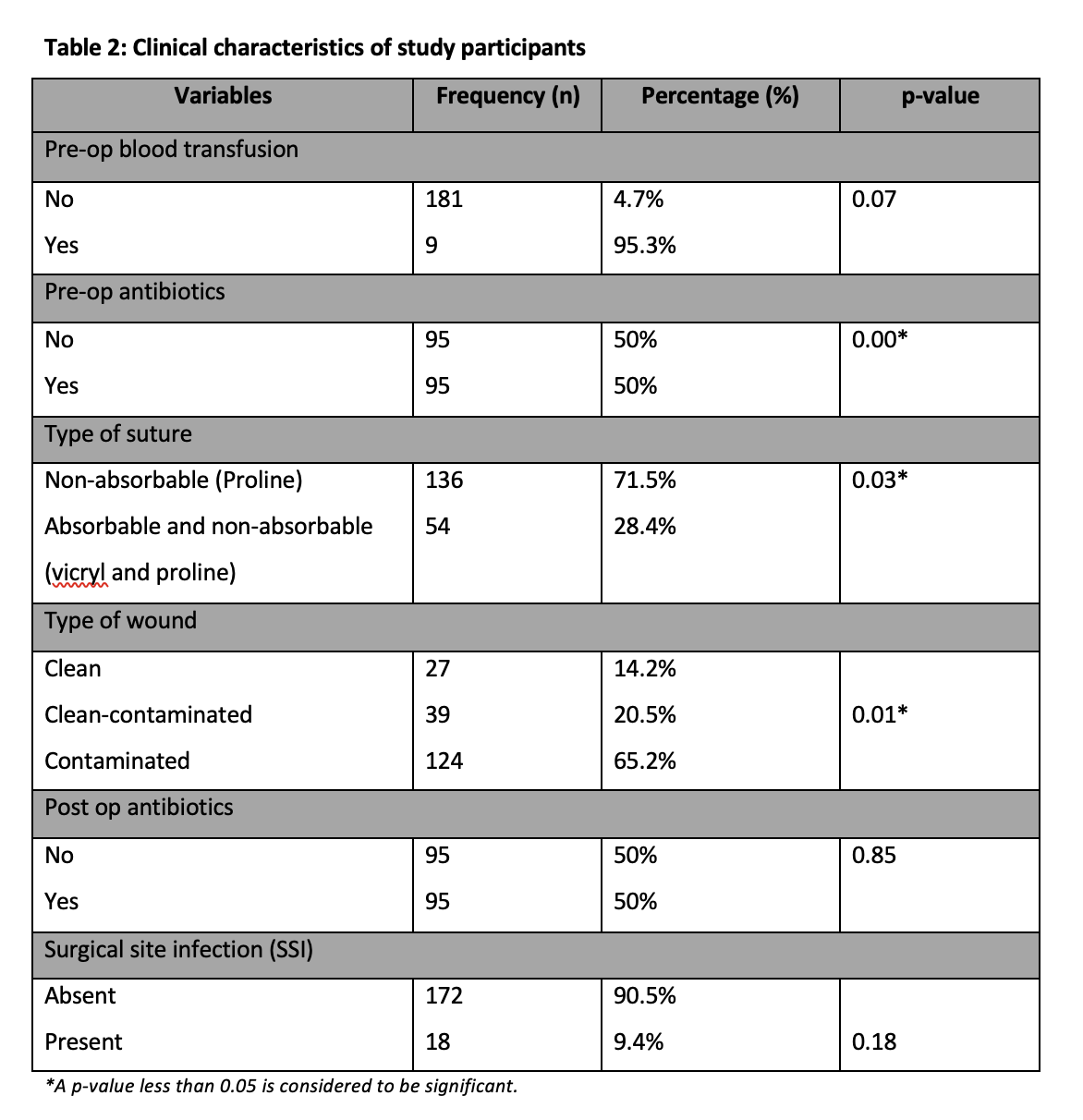
Pre-op blood transfusion was done in 9(95.3%) patients with a p-value 0.07 whereas the pre-op antibiotic was given in 95(50%) patients and half of the patients were given post-op antibiotics with a p-value 0.00. Surgery duration was less than 1 hour in all patients with a p-value 0.03 and local anesthesia was used in every surgery. Non-absorbable suture (proline) was used in 136(71.5%) patients while absorbable and non-absorbable (vicryl and proline) was used in 54(28.4%) patients. Out of the total, 27(14.2%) patients had clean wounds, 39(20.5%) patients had clean-contaminated wounds, and 124(65.2%) patients had contaminated wounds with p-value 0.01. Details are shown in Table 2.
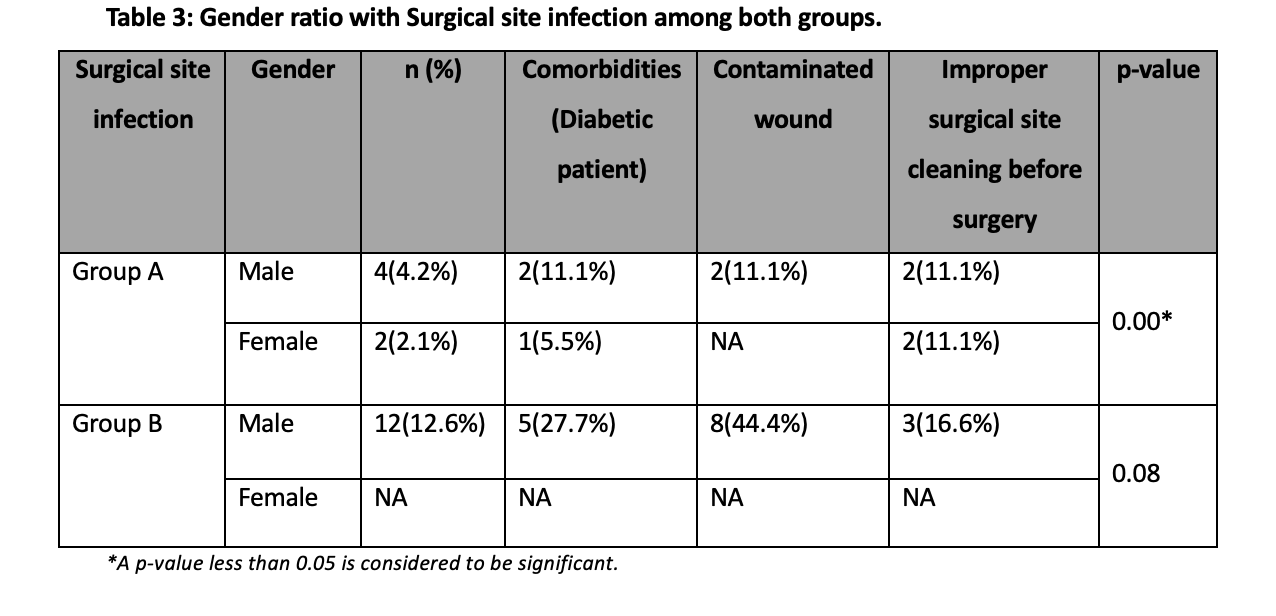
Surgical site infections occurred in 18 out of 190 patients, with 6 (6.3%) patients from group A and 12 (12.6%) from group B. In Group A, two (2.1%) of the patients who acquired SSI were female with one woman having trauma at the leg and one got at hand, whereas in Group B, the patients with SSI were male and no female patients had SSI. In group B men got trauma at the head, legs, and arm. In group A out of 18 SSI 2(11.1%) male and 1(5.55%) female patients are diabetic and 2 have contaminated wounds while in group B 5(27.7%) patients are diabetic and 8(44.4%) have contaminated wounds with a p-value of 0.00 that is significant. The most important risk factors for SSI in minor trauma cases were contaminated wounds, diabetes, and improper surgical site cleaning before surgery. Details are shown in Table 3.
SSIs are known to be one of the most common causes of nosocomial infections worldwide. They still form a large health problem and result in increased antibiotic usage, increased associated costs, and prolonged hospitalization, and contribute to increased patient morbidity and mortality 10,11. The rate of SSI varies greatly, from 2.5% to 41.9% as per different studies, worldwide and from hospital to hospital 12.
The rate of surgical site infections found in this study was 18 (9.4%). Moreover, wound class was also found to be an important risk factor in the development of SSI13. Hence, the contaminated wound had the highest odds of becoming infected followed by the clean-contaminated 14.
Surgical site infections occurred in 18 out of 190 patients, with 6 (6.3%) patients from group A and 12 (12.6%) from group B. In Group A, two (2.1%) of the patients who acquired SSI were female with one woman having trauma at the leg and one at hand, whereas in Group B, the patients with SSI were male and no female patients had SSI. In group B men got trauma at the head, legs, and arm. In group A out of 18 SSI 2(11.1%) male and 1(5.55%) female patient are diabetic and 2 have contaminated wounds while in group B 5(27.7%) patients are diabetic and 8(44.4%) have contaminated wounds with a p-value of 0.00 that is significant. Some studies revealed that in clean surgical procedures, there is no need for a prophylactic antibiotic because it causes bacterial resistance but it also depends and varies from surgery to surgery 15. Syed MH et al. did a study at King Fahad Hospital in Saudi Arabia. In their investigation, they concluded that the incidence of SSI is extremely minimal in clean surgical operations and that needless antibiotic prophylaxis may promote antimicrobial resistance. In another study, Anand T et al. concluded that routine use of prophylactic antibiotics in elective hernia surgery in children provides little benefit and should be avoided 16.
A local study conducted by Kayani, Z, et al. concluded that the administration of prophylactic antibiotics in a clean surgical procedure does not significantly lower the risk of SSI. Considering the foregoing data, it is proposed that the routine use of prophylactic antibiotics be discouraged. The majority of clean surgical operations do not necessitate prophylactic antibiotic coverage. Antimicrobial resistance and treatment costs will be reduced if antibiotics are used wisely17.
The use of antibiotics in surgical patients for prophylaxis is a justifiable practice; however, the appropriate route of administration, timing, and duration of prophylactic antibiotics should be chosen to achieve high plasma and tissue levels of antibiotics during and shortly after the surgical procedure when bacterial contamination is maximal 18-20.
A study in 2021 was conducted by Nabi Bux Napar and other contributors on SSI in children undergoing Elective inguinal with and without Prophylactic antibiotics. The study’s objective was to establish the frequency of SSI in children having elective inguinal hernia who received antibiotic prophylaxis and those who did not by creating two groups of A and P. A total of 160 patients were chosen for the research. Before the induction of anesthesia, Group A got the antibiotic ceftriaxone 1g/kg, while Group P received a placebo. The patient’s details and the length of the procedure were recorded. Following surgery, all patients were checked for temperature, inflammation, and site discharge. On the first, third, seventh, and thirty-first days after surgery, the surgical site was inspected post-operatively. There was a total of 116 individuals, but 12 of them experienced SSI. which included five cases from group P and seven patients from group A (13) 21,22. In our study, 190 patients in total were chosen for the research. The individuals who were chosen ranged in age from 16 to 70. Surgical site infections occurred in 18 out of 190 patients, with 6 (6.3%) patients from group A and 12 (12.6%) from group B. In Group A, two (2.1%) of the patients who acquired SSI were female, whereas in Group B, twelve (12.6%) of the patients with SSI were male and no female patients had SSI with a p-value of 0.186 which is insignificant Also, antibiotic prophylaxis with proper timing has paramount importance in decreasing the incidence of SSI. In addition, considering the type of wound, duration of surgery and comorbid condition would also have a vital role in minimizing SSI rate.
It is concluded in our study that the use of prophylactic antibiotics in minor trauma cases performed in adult patients does significantly decrease the incidence of surgical site infection. The major risk factors for developing SSI in trauma surgery were contaminated wounds, diabetes, and improper surgical site cleaning before surgery.
We would like to acknowledge Dr. Usra Naeem for her immense contribution to data management.
The authors declared no conflict of interest.
Informed consent was taken from the patients.
SM collected the data and wrote the manuscript. GM analyzed and interpreted the patients’ data. The US helped in writing the first draft.
- Lakoh S, Yi L, Sevalie S, Guo X, Adekanmbi O, Smalle IO et al. Incidence and risk factors of surgical site infections and related antibiotic resistance in Freetown, Sierra Leone: a prospective cohort study. Antimicrob Resist Infect Control. 2022;11(1):39. doi: 10.1186/s13756-022-01078-y.
- Vander Poorten V, Uyttebroek S, Robbins KT, Rodrigo JP, de Bree R, Laenen A et al. Perioperative Antibiotics in Clean-Contaminated Head and Neck Surgery: A Systematic Review and Meta-Analysis. Adv Ther. 2020;37(4):1360-1380. doi: 10.1007/s12325-020-01269-2.
- Syed MK, Al Faqeeh AA, Othman A, Hussein AA, Rajab H, Hussain S, Zaidi SMJ et al. Antimicrobial Prophylaxis in Clean Pediatric Surgical Procedures: A Necessity or Redundancy? Cureus. 2020;12(9):e10701. doi: 10.7759/cureus.10701.
- Kreß JS, Rüppel M, Haake H, Vom Dahl J, Bergrath S. Short-term outcome and characteristics of critical care for non-trauma patients in the emergency department. Anaesthesist. 2022;71(1):30-37. English. doi: 10.1007/s00101-021-00953-4.
- Orelio CC, van Hessen C, Sanchez-Manuel FJ, Aufenacker TJ, Scholten RJ. Antibiotic prophylaxis for prevention of postoperative wound infection in adults undergoing open elective inguinal or femoral hernia repair. Cochrane Database Syst Rev. 2020;4(4):CD003769.doi:10.1002/1465185
- Nichols RL, Smith JW, Klein DB, Trunkey DD, Cooper RH, Adinolfi MF, Mills J. Risk of infection after penetrating abdominal trauma. N Engl J Med. 1984;311(17):1065-1070. doi: 10.1056/NEJM198410253111701.
- Legesse Laloto, T., Hiko Gemeda, D. & Abdella, S.H. Incidence and predictors of surgical site infection in Ethiopia: prospective cohort. BMC Infect Dis 17, 119 (2017). https://doi.org/10.1186/s12879-016-2167-x
- Mujagic E, Zeindler J, Coslovsky M, Hoffmann H, Soysal SD, Mechera R et al. The association of surgical drains with surgical site infections – A prospective observational study. Am J Surg. 2019;217(1):17-23. doi: 10.1016/j.amjsurg.2018.06.015.
- Misganaw D, Linger B, Abesha A. Surgical Antibiotic Prophylaxis Use and Surgical Site Infection Pattern in Dessie Referral Hospital, Dessie, Northeast of Ethiopia. Biomed Res Int. 2020;2020:1695683. doi: 10.1155/2020/1695683.
- Singh M. P., Brahmchari S., Banerjee M. Surgical site infection among postoperative patients of the tertiary care center in Central India-a prospective study. Asian Journal of Biomedical and Pharmaceutical Sciences. 2013;3(17):p. 41.
- Gottrup F., Melling A., Hollander D. A. An overview of surgical site infections: aetiology, incidence and risk factors. EWMA Journal. 2005;5(2):11–15.
- Elbur AI, M A Y, El-Sayed AS, Abdel-Rahman ME. Prophylactic antibiotics and wound infection. J Clin Diagn Res. 2013;7(12):2747-2751. doi: 10.7860/JCDR/2013/6409.3751.
- Kayani Z, Awan S, Abbasi M, Gilani I, Akhtar N, Sabir F. Role of prophylactic antibiotics in clean surgery. PJP. 2019;15(2):38-40.
- Network SIG. Antibiotic Prophylaxis in Surgery.Edinburgh: A National Clinical Guideline, SIGN; 2000.
- Anand T, Gupta S, Gupta A. Routine use of antibiotics in hernia surgery in children: Is it really required? Journal of Medical Science And clinical Research. 2018;6(9). DOI:10.18535/jmscr/v6i9.187.
- Dellinger E. P., Gross P. A., Barrett T. L., et al. Quality standard for antimicrobial prophylaxis in surgical Procedures. Infection Control and Hospital Epidemiology. 1994;15(3):182–188. doi: 10.1086/646887.
- Zhiqing L, Yongyun C, Wenxiang C, Mengning Y, Yuanqing, M, Zhenan, Z et al. Surgical masks as source of bacterial contamination during operative procedures. Journal of Orthopaedic Translation. 2018;14(1)57-62. DOI: 10.1016/j.jot.2018.06.002.
- Chatterjee, A., Modarai, M., Naylor, N. R., Boyd, S. E., Atun, R., Barlow, J., … Robotham JV. Quantifying drivers of antibiotic resistance in humans: A systematic review. The Lancet Infectious Diseases. 2018;18(12),e368-e378. DOI: 10.1016/s1473- 3099(18)30296-2.
- Cheadle WG. Risk factors for surgical site infection. Surg Infect (Larchmt). 2006;7 Suppl 1:S7-11. doi: 10.1089/sur.2006.7.s1-7.
- Koullouros M, Khan N, Aly EH. The role of oral antibiotics prophylaxis in prevention of surgical site infection in colorectal surgery. International Journal of Colorectal Disease. 2016;32(1):1-18. DOI:10.1007/s00384-016-2662-y.
- Napar NB, Shaikh NA, Baloch I, Shah AA, Shaikh B, Mahtam I. Surgical Site Infection with and without Prophylactic Antibiotic in Children undergoing Elecltive Inguinal Herniotomy. Journal of Rawalpindi Medical College. 2021;25(4).https://doi.org/10.37939/jrmc.v25i4.1681
- Ma T, Lu K, Song L, Wang D, Ning S, Chen Z et al. Modifiable factors as current smoking, Hypoalbumin, and elevated fasting blood glucose level increased the SSI risk following elderly hip fracture surgery. Journal of Investigative Surgery. 2019; 33(8):750-758. DOI:10.1080/08941939.2018.1556364.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
