By Farhan Mir1, Nazia Mushtaq1, Ihsanullah2, Ruby Qureshi1, Zara Noor1, Arzina Zaheer abbas1
- Leishmaniasis Clinic Institute of Skin Diseases, Karachi, Pakistan
- Zoology Department, Karachi University, Karachi, Pakistan
DOI: https://doi.org/10.36283/PJMD12-4/014
How to cite: Mir F, Mushtaq N, Ihsanullah, Qureshi R, Noor Z, Abbas AZ. Body Locations of Leishmaniasis in the Targeted Population of Pakistan. Pak J Med Dent. 2023;12(4): 75-79. Doi: 10.36283/PJMD12-4/014
Background: Cutaneous leishmaniasis (CL), a skin infection caused by a sand fly bite, is most prevalent clinically in Pakistan. The initially caused nodules (bumps) may become ulcerated, have a long healing time, and may re-occur multiple times. This study identified the body areas most affected by Leishmaniasis in our target population.
Methods: This prospective study was conducted at the leishmaniasis clinic Institute of Skin Diseases Sindh Karachi (ISDSK), from July 2022 to June 2023. A standard questionnaire recorded demographics and site, location, and number of lesions. The diagnosis was confirmed by a Slit Skin smear showing Leishmania. The ANOVA was used to determine the mean difference between the variables and p < 0.05 was considered significant.
Results: Out of 138 patients, 87 (63%) were females and 51 (37%) males. The most common site of involvement was lower limb and feet at 44(32%) followed by face and neck at 37(27%), upper limb at 37(27%), and multiple sites at 20(14%). Majority of patients had single lesions 72(52%) followed by, two 34(25%), three 9(6%) and four or more in 23(14%). A comparison of lesions in gender, revealed, that males had 17(33%) on upper limbs, while females had 31(35%) on lower limbs. Comparing body locations province-wise, in Sindh predominant was lower limb 41(34%) whereas face in Balochistan 6(35%).
Conclusion: CL’s most infected locations were face & neck and lower limbs of the body. Comparing gender, females were more affected. This is an increasing public health problem and requires attention of authorities, to fumigate the pandemic areas.
Keywords: Leishmaniasis, Cutaneous, Endemic
Cutaneous leishmaniasis (CL) is an infection of the skin caused by the biting of sand fly. It is a vector-borne zoonosis, with dogs, rodents, wolves, and foxes as common reservoir hosts and humans as incidental hosts1,2. There are different types of Leishmanias caused by Phlebotomus or Lutzomyia species of the genus Leishmania, affecting different areas of the body, but in Pakistan CL is clinically the most prevalent manifestation. Leishmaniasis is endemic in several parts of the world, particularly in tropical countries. Asian populations commonly consist of persons of poor localities having sub-standard living styles. Such individuals are more susceptible to vector-borne infections. Initially caused nodules (bumps) may become ulcerated and take a long time to heal and may re-occur multiple times. These may be single or multiple and may be associated with systemic complications3.
CL is endemic in Pakistan and most affected are children both males and females, who get infected by playing with their peers. Exposed body parts such as the face, hands, and legs are targeted by vector 4. Patients report in skin hospitals with a wide range of clinical manifestations and most frequently extensive skin ulceration5. The three clinical manifestations cutaneous leishmaniasis (CL), mucocutaneous leishmaniasis (ML), and visceral leishmaniasis (VL), are all caused by more than 20 well-known Leishmania species6. Over the past three decades, CL endemic areas in Afghanistan have moved to Pakistan, and outbreaks of CL have happened in refugee camps and among native Pakistani people close to related areas 7, 8.
This is an increasing public health problem in our population and the cause and most vulnerable area of the body for the infection is required to be investigated. This study aimed to find out which areas of the body are most affected by Leishmaniasis in our target population.
This prospective study was conducted at the leishmaniasis clinic Institute of Skin Diseases Sindh Karachi (ISDSK) which caters to patients from all provinces, mainly from Karachi, Balochistan, Sindh (interior), KPK, and Punjab. The patients were inducted from July 2022 to June 2023, after obtaining informed consent from each participant. After receiving approval from the Ethics Review Committee, the samples were collected. A convenient sampling method was used. Demographic and baseline characteristics including name, gender, site of involvement, location of disease, and number of lesions were recorded on a prepared questionnaire. The diagnosis was confirmed by a Slit Skin smear showing Leishmania.
The analysis of data was performed using SPSS v. 28. All the quantitative variables of the study were calculated as mean and standard deviation (SD), and frequency and percentages were used for qualitative variables. The ANOVA was used to determine the mean difference between the variables. The p < 0.05 was considered statistically significant for all the values of the study data.
A total of 138 patients were included in the study. There was a slight preponderance of female gender 87 (63%) and male 51 (37%). Regional distribution showed that there were 120(87%) patients from the Province of Sindh, Followed by 17(12%) from Balochistan and 1(0.7%) from Punjab. The most common site of involvement was the lower limb along with feet 44(32%) followed by the face and neck 37(27%), upper limb 37(27%), and multiple sites of involvement was seen in 20(14%). The Most common patients had single lesions in 72 (52%) followed by, two lesions in 34(25%), three lesions in 9(6%), and four or more lesions were found in 23(14%). (Table 1)
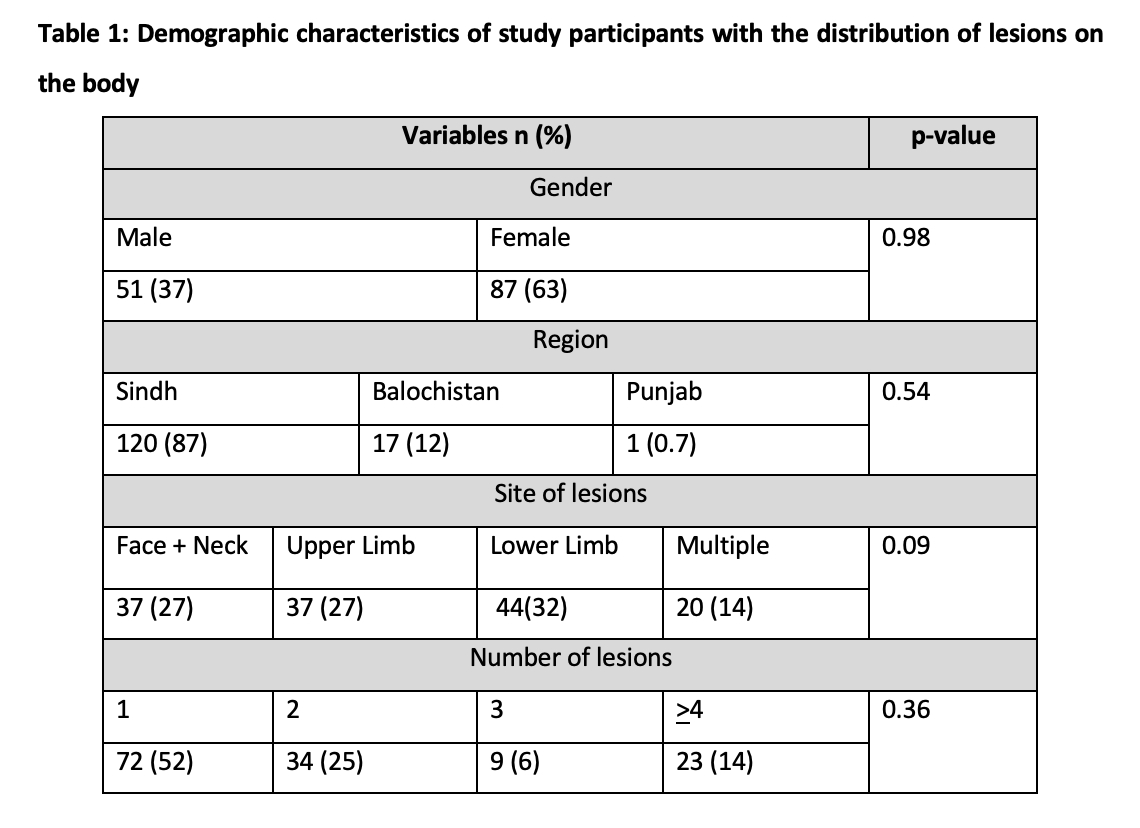
In comparison between males and females, upper limbs were commonly involved in males 17(33%), while lower limb was commonly involved in females 31(35%) with a p-value of 0.484.
While comparing the patients from different provinces we found that patients from Sindh had predominantly lower limb involvement 41(34%), from Balochistan face was the commonest site of involvement 6(35%), And from Punjab, only one patient showed involvement of the Lower limb. Though region-wise values looked remarkable the results were statistically not significant (P =0.412).
Table 2: Association of the site of lesions with gender and region
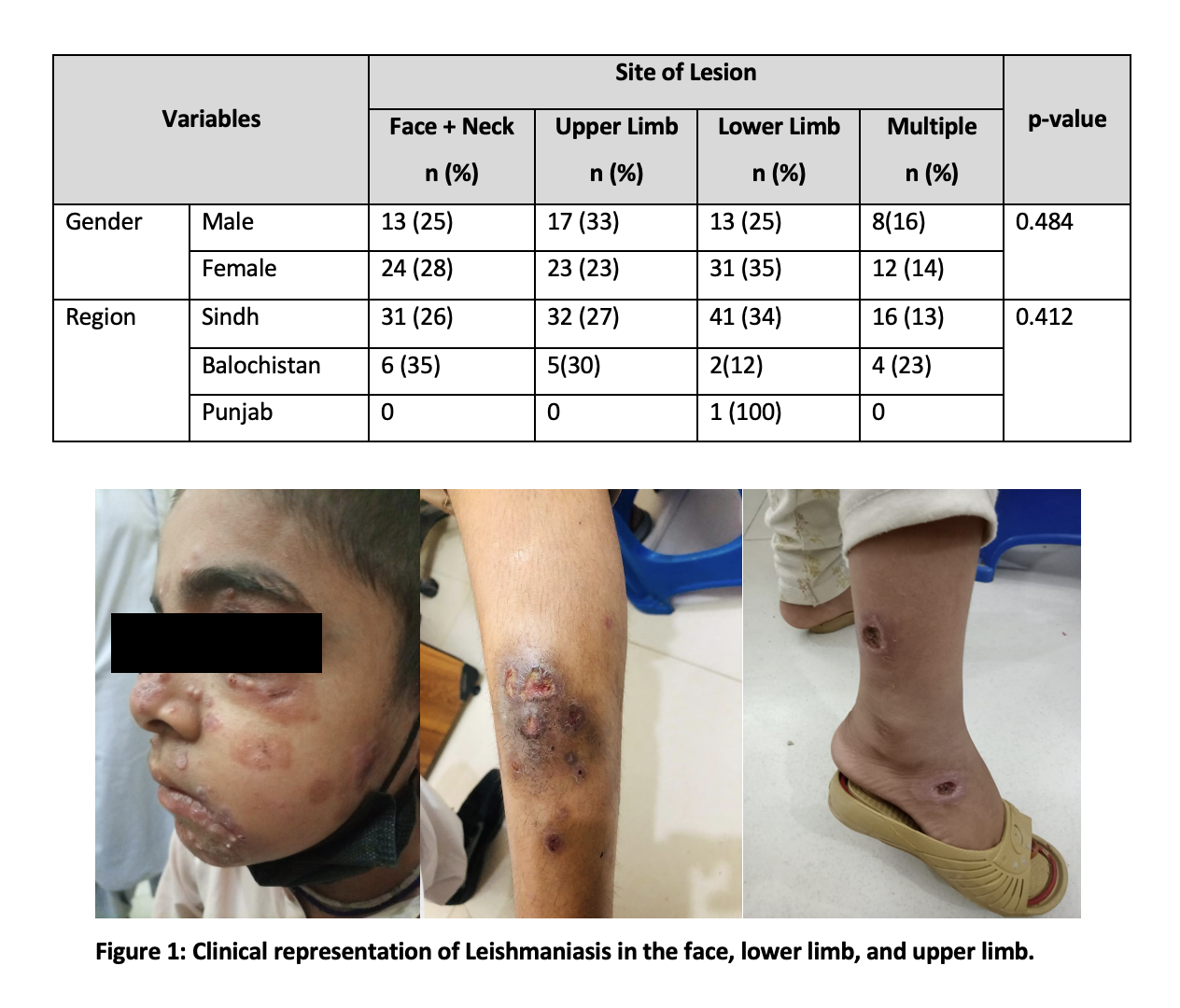
The main finding of the site of involvement was the lower limb along with feet 44 (32%). The lesions in the lower limb have been reported to cause more problems compared to other areas because of pain and discomfort in mobility as well as difficulty in self-care and daily activities6.
The second most common site was the face and neck 37(27%), followed by the upper limb 37(27%), multiple sites of involvement were seen in 20(14%). The lesions on the other sites of the body, such as on the head or face, do not look as if they contribute toward negative or inhibited behavior among the social surroundings, however, people with multiple lesions avoid socializing6.
This shows the social and psychological impact of Cutaneous Leishmania can be damaging and can hamper the quality of life of patients due to disfiguring scar formation and mutilation leading to social stigmatization4,7-10. A higher frequency of facial CL lesions has been reported from the Middle East, which may be due to the local dressing of the population with only the uncovered parts, face, hands, and feet affected while most of the body including the limbs remain covered, and thus are protected from the vector of CL, the sand flies and hazardous chemicals 11-14.
There are more than 20 well-known Leishmania species that can infect humans and cause the three clinical forms of the disease, cutaneous leishmaniasis (CL), mucocutaneous leishmaniasis (ML), and visceral leishmaniasis (VL)6. CL endemic areas in Afghanistan have migrated to Pakistan over the past three decades, and outbreaks of CL have occurred in refugee camps and indigenous Pakistan populations near associated areas 7,8. Persons with active lesions suffer from severe stigma in Pakistan due to the lack of information about the disease and its transmission 9,10. Cutaneous leishmaniasis is spread through bloodsucking sand flies (Phlebotomus), consisting of 37 species reported from Pakistan 10, 15,16. Algeria, Brazil, Iran, Syria, Afghanistan, Pakistan, Tunisia, and Peru are the countries with the most affected by this disease and the highest number of cases reported 17-21. Prevalent data described its prevalence in sixteen developed and 72 developing countries (WHO, 2015), causing 0.1 million deaths every year 17-18. In our study, there was a predominance of female patients which has also been reported by another study from Pakistan4. However, studies from Europe more men getting infected by CL, because of the association of CL with frequent visits to the interior (rain forest) for work or leisure-related reasons, with results showing 92,0% of male patients10.
In Pakistan11, the reported prevalence rate is 60.5% in males and 39.5% in females from the North West Frontier Province (NWFP) which shows the disease is more prevalent in males than females. They also reported young individuals 1-15 years of age are more affected by this disease than older age group. In the present study, we observed 63% female and 37% male which shows the steadiness of vector-borne diseases in Pakistan. According to Ali et al,11 16 out of 207 cases 64% of males were found positive and significantly high prevalent than 36% of females. Furthermore, they reported most infected body parts, legs are found highly infected 45%, Face 26%, arms 20%, and 9% mixed body parts. In the present study, we found dominantly affected 32% of feet (Legs), Face and neck 27%, upper limbs 27%, and multiple site lesions 14%. The study suggests that CL diagnosed in endemic settings reduces the quality of life of patients 22. Therefore, further work including different factors is required to examine and monitor the long-term impact of CL on patient life and to study the most effective therapies for better survival of patients.
Cutaneous Leishmania in our targeted area mostly infected the face neck and lower limbs of the body. Comparing the gender, females were found more affected. This is an increasing public health problem and requires the attention of authorities, to fumigate the pandemic areas.
We would like to acknowledge the institute for its support.
The authors declared no conflict of interest.
Informed consent was taken from the patients.
All authors contributed equally to the study.
- Ayatollahi J, Bafghi AF, Shahcheraghi SH. Chronic zoster-form: a rare variant of cutaneous leishmaniasis. Reviews and Research in Medical Microbiology. 2015;26(3):114-115 DOI:10.1097/MRM.0000000000000031
- da Silva GA, Sugui D, Nunes RF, de Azevedo K, de Azevedo M, Marques A, Martins C, Ferry FR. Mucocutaneous leishmaniasis/HIV coinfection presented as a diffuse desquamative rash. Case Reports in Infectious Diseases. 2014;2014. doi: 10.1155/2014/293761
- Saurabh S. Leishmaniasis. Lancet (London, England). 2019;393(10174): 871. https://doi.org/10.1016/S0140-6736(18)33046-0
- Kassi M, Kassi M, Afghan AK, Rehman R, Kasi PM; Marring leishmaniasis: the stigmatization and the impact of cutaneous leishmaniasis in Pakistan and Afghanistan.PLoSNegl Trop Dis. 2008;2(10):e259.https://doi.org/10.1371/journal.pntd.0000259
- Van der Meide WF, Jensema AJ, Akrum RA, Sabajo LOA, Lai A Fat RFM, Lambregts L, et al. Epidemiology of Cutaneous Leishmaniasis in Suriname: A Study Performed in 2006. Am. J. Trop. Med. Hyg. 2008;79(2): 192–197. doi: 10.1371/journal.pntd.0008759
- Clem A. A current perspective on leishmaniasis. Journal of global infectious diseases. 2010 May;2(2):124. DOI: 4103/0974-777X.62863
- Brooker S, Mohammed N, Adil K, Agha S, Reithinger R, Rowland M. et alLeismaniasis in Refugee and Local Pakistani Populations.Emerg Infedt. Dis. 2004;10:1681-1686. https://doi.org/10.3201/eid1009.040179
- Hussain M, Munir S, Ayaz S, Khattak B. U., Khan T. A., Muhammad N. et al.. First report on molecular characterization of Leishmania species from cutaneous leishmaniasis patients in southern Khyber Pakhtunkhwa province of Pakistan. Asian Pacific Journal of Tropical Medicine. 2017; 10(7):718-721. doi: 10.1016/j.apjtm.2017.07.015
- Yanik M, Gurel MS, Simsek Z, Kati M. The psychological impact of cutaneous leishmaniasis. Clin Exp Dermatol. 2004:29:464–467. https://doi.org/10.1111/j.1365-2230.2004.01605.x
- Kassi M, Kassi M, Afghan A. K., Rehman R. & Kasi, P. M. Marring leishmaniasis: the stigmatization and the impact of cutaneous leishmaniasis in Pakistan and Afghanistan. PLoS neglected tropical diseases. 2008;2(10): e259.
- Ali A, Rehman TU, Qureshi NA, Rahman HU. The new endemic focus of cutaneous leishmaniasis in Pakistan and future epidemics threats. Asian Pacific Journal of Tropical Disease, 2016;6(2),155-159.
- Ali N, Ullah A, Wahid S, Khisroon M, Rasheed SB. Distribution, species composition and relative abundances of sandflies in North Waziristan Agency, Pakistan. Medical and Veterinary Entomology, 2016;30(1), 89-94.
- Khan K, Wahid S, Khan NH, Ali N. Potential resting and breeding sites of sand Flies (Diptera: Psychodidae) and their habitat characteristics in Leishmaniasis Foci of Dir Districts, Khyber Pakhtunkhwa, Pakistan. Journal of medical entomology, 2017;54(5):1390-1396.
- Ramdas S; Cruel disease, cruel medicine: Self-treatment of cutaneous leishmaniasis with harmful chemical substances in Suriname. Social Science and Medicine 2012; 75: 1097–1105. https://doi.org/ 10.1016/j.socscimed.2012.04.038.
- SamiUllah D, Jan AH, Wazir SM, Ali N. Prevalence of cutaneous leishmaniasis in Lower Dir District (N.W.F.P), Pakistan. J Pak Assoc Dermatol. 2016;19(4):212-215
- Ihsanullah M, Yousuf MJ, Ahmad N, Masood Z, Majeed S, Hassan HU, Shaikh F. Prevalence of cutaneous leishmaniasis in the largest populated city Karachi, Pakistan. Brazilian Journal of Biology. 2021;83:e247583. https://doi.org/10.1590/1519-6984.247583
- Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M; WHO Leishmaniasis Control Team. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7(5):e35671. doi: 10.1371/journal.pone.0035671.
- World Health Organization. Investing to overcome the global impact of neglected tropical diseases: third WHO report on neglected tropical diseases 2015;3.
- fghan AK, Kassi M, Kasi PM, Ayub A, Kakar N, Marri SM. Clinical manifestations and distribution of cutaneous leishmaniasis in pakistan. J Trop Med. 2011;2011:359145. doi: 10.1155/2011/359145.
- Ricardo VPFHu, Ramdas S, Nieuwkerk P, Reis R, Lai A Fat RFM, de Vries HJC, et al. Body location of “New World” cutaneous leishmaniasis lesions and its impact on the quality of life of patients in Suriname. PLoS Negl Trop Dis. 2020; 14(10): e0008759. https://doi.org/10.1371/journal. pntd.0008759
- Reithinger R, Aadil K, Kolaczinski J, Mohsen M, Hami S. Social impact of leishmaniasis, Afghanistan. Emerg Infect Dis. 2005;11:634–636. https://doi.org/10.3201/eid1104.040945
- Peleva E, & Walker S. L. Cutaneous leishmaniasis and health-related quality of life in returning travellers to the UK. Journal of travel medicine. 2020; 27(7): taaa188. https://doi.org/10.1093/jtm/taaa188
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
