By Zainul Cholid1, Yuliana Mahdiyah Da’at Arina2
- Department of Oral and Maxillofacial Surgery, University of Jember, Indonesia
- Department of Periodontics, Faculty of Dentistry, University of Jember, Indonesia
DOI: https://doi.org/10.36283/PJMD12-3/011
How to cite: Cholid Z, Arina YMD. Mediastinitis due to Odontogenic Infection. Pak J Med Dent. 2023;12(3): 62-66. doi: 10.36283/PJMD12-3/011
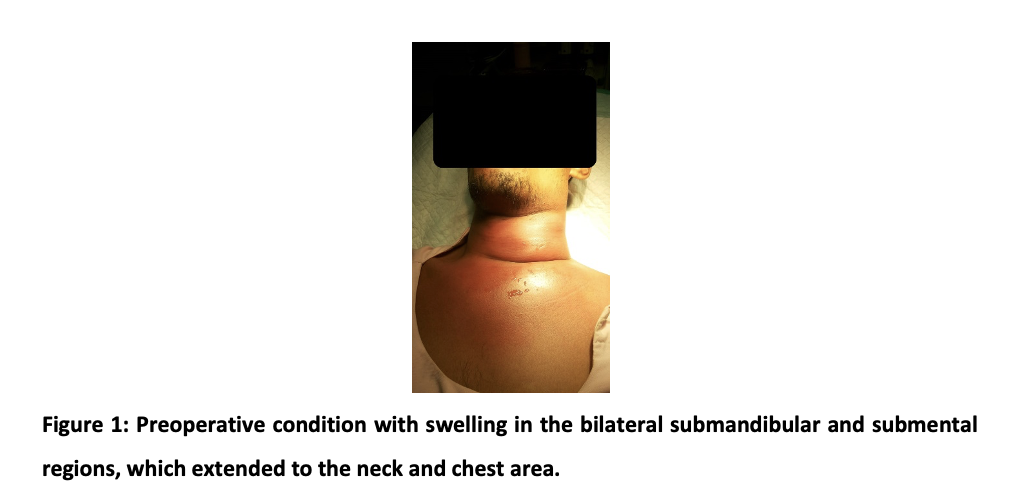
Mediastinitis due to the spreading of odontogenic infection is rare, but the mortality rate is high. This report presents the case of mediastinitis caused by the spreading of odontogenic infection in healthy males. The patient complained of dyspnoea and trismus. The diffuse and fluctuating swelling was observed in the submandibular and submental area, which spreads to the neck and chest. It was diagnosed mediastinitis as a submandibular and submental abscess complication due to the impacted teeth’ pericoronitis. Two drainage incisions were made following the administration of oxygen and antibiotics injection. The success of mediastinitis treatment due to the spread of odontogenic infection is determined by proper diagnosis and appropriate initial management. Antibiotic administration and pus drainage are the very decisive stage of treatment to reduce the risk of death. It is necessary to eliminate the causative of odontogenic infection.
Keywords: Impacted teeth, Mediastinitis, Odontogenic infection, Pericoronitis
Odontogenic infections can spread and cause complications such as mediastinitis1. Mediastinitis is severe inflammation in the chest cavity and potentially causes death2. Mediastinitis can occur due to the spread of infection from the head or neck, pharyngeal,3 and as complications of odontogenic infection 4,5. Mediastinitis due to the spread of infection from pericoronitis of impacted teeth needs attention because impacted teeth are often ignored. Comprehensive treatment is needed when mediastinitis occurs due to odontogenic infection. A delay in diagnosis and inadequate initial treatment can be a factor in the high mortality rate due to mediastinitis6.
This study was conducted at a medical university in Rawalpindi, Pakistan. It is a Cross-sectional study. The sample size was calculated using the WHO sample size calculator which came out to be n=210 from a population of 460 medical students with a 95% confidence level and 5% margin of error. The survey was filled by 211 participants from different years of M.B.B.S after taking informed consent. The Institutional Review Board (IRB) of Rawalpindi Medical University approved the study (Reference number is PSY-69-46-22).
The sampling was done by using Convenient sampling and data collection was completed from September 2022 to December 2022. All the medical students of all the years were included in this study. Whereas, medical students who were foreigners (belonged to other nations than Pakistan) were excluded from this study. Informed consent was taken from all participants before participating in this study. A pre-made questionnaire was adapted through literature review 20 and after applying a few changes was used to assess the knowledge and perceptions of medical students regarding AI was employed. All responses were recorded on google forms. IBM SPSS version 26 and Microsoft Excel were used for data analysis for designing graphs and tables. The Name of the repository was Zenodo with a Persistent identifier / DOI: https://doi.org/10.5281/zenodo.7589254 under the Data license of Creative Commons Attribution 4.0 International.
A 38-year-old man complained of swelling in the neck and chest and shortness of breath. From the anamnesis, it is known that the swelling has been suffered from 10 days ago. Initially, the patient complained of pain in the left of a lower molar tooth. Three days after the toothache, the swelling appeared under the left lower jaw, extended to the right lower jaw, and spread to the neck and chest.
Extra oral examination showed swelling in the bilateral submandibular and submental regions which extended to the neck and chest. The swelling was red and diffuse. On palpation, it was warm, painful, and fluctuated. The mouth opening was limited, and the interincisal distance was 1,5 cm. The intra-oral examination showed that the left mandibular molar third gingiva was red. A slight diffuse and painful swelling appeared under the tongue, but the tongue did not lift. The results of blood tests showed an increase in the number of total leukocytes indicating a severe infection, while the function of liver, renal, and glucose values was still normal. The panoramic radiography showed that the left mandibular third molar partially erupted. The thorax radiography showed fog in the left lung, so he was referred to a pulmonologist. The patient was consulted by an internist for an HIV examination with non-reactive results. The patient was diagnosed with mediastinitis from submandibular and submental abscesses due to the pericoronitis of impacted teeth (Figure 1).
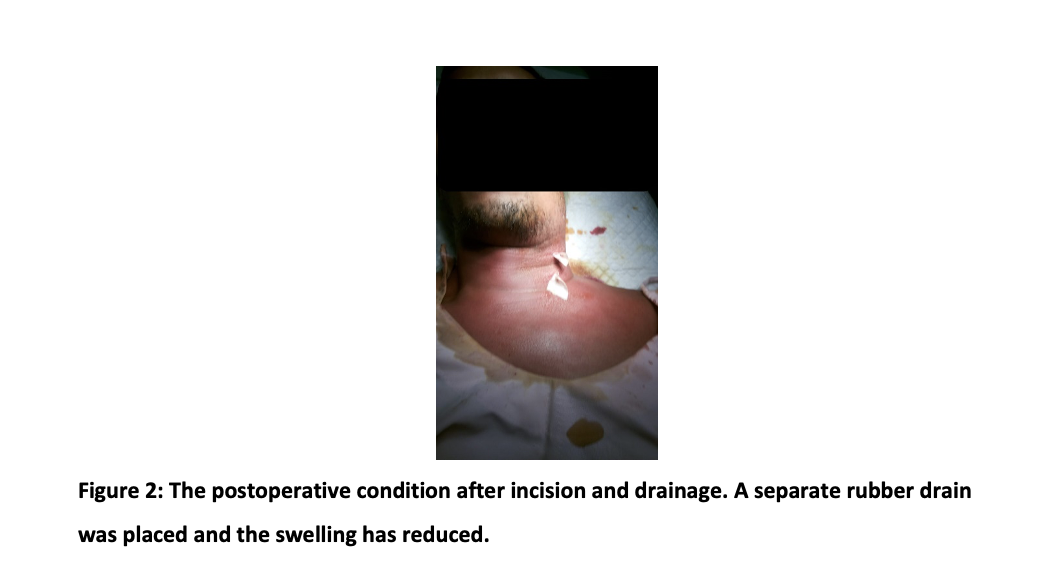
The patient was hospitalized, and the administration of antibiotics, incision drainage, and extraction of impacted teeth were planned. The intravenous administration of antibiotic Ceftriaxone 2x2g, Metronidazole infusion 3×500 mg, and Ketorolac 3 x 30 mg were given for five days. The oxygen 2l/min was suggested because the patient still has shortness of breath. On day three, the incisions using blade no. 11 in the left neck in the two most volatile places were made after obtaining permission from a pulmonologist. Then a blunt dissection to explore the abscess area was performed with an arterial clamp and finally installed a separate rubber drain (Figure 2). The drain is replaced daily, and the neck area is massaged to remove the pus.
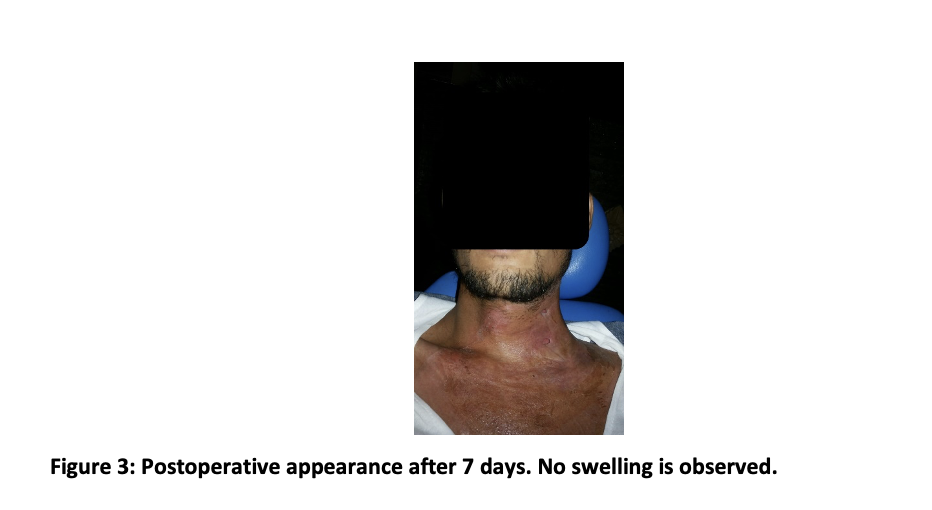
Seven days after the incision, the recovery was satisfactory. The swelling in the neck and chest is not found, nor the shortness of breath; however, the skin in the neck and chest area still showed redness (Figure 3). The incision hole is also still visible. Pus production has also started to stop, so it was decided to remove the drain. The following treatment plan was to remove the partially impacted left mandibular molar third, which was the focus of the infection. We have educated that the impacted tooth causes the mediastinitis and that recurrences may occur, so the impacted tooth should be removed. However, the patient still refused it.
Mediastinitis is a life-threatening infection7 and occurs acutely and in a very short time3. There are three types of mediastinitis; postoperative, descending necrotizing, and fibrotic. 70% of mediastinitis cases are descending necrotizing mediastinitis, due to the spread of infection from the head or neck3. In this case, the diagnosis is descending necrotizing mediastinitis due to the expansion of bilateral submandibular and submental abscesses due to partially impacted mandibular third molars.
Descending necrotizing mediastinitis involves spreading infection from a pathological process in the head and neck, such as a neck abscess, Ludwig’s angina, or other dental infection3. 60–70% of descending necrotizing mediastinitis originates from odontogenic infections8. Odontogenic infections can originate from the dentoalveolar, peri coronal, and periodontal tissues6. This case is mediastinitis originating from a disseminated odontogenic infection that from pericoronitis of a partially impacted third molar which developed into a submandibular and submental abscess. In partially impacted teeth, there is a potential space between the peri coronal gingiva and the tooth, which can promote the growth of anaerobic bacteria, causing pericoronitis. The pericoronitis infection continued periapical to the medulla, penetrated the cortical bone, spread to the Oro maxillofacial space, and became a submandibular and a submental abscess. According to Ogle9, the most common types of odontogenic infections are buccal space abscesses and sub-mandibular abscesses (60%), and fossa canine abscesses (16%).
The spread of infection to the Oro maxillofacial space is influenced by root length, the root position relative to muscle attachment, bone thickness, porosity, and gravitational forces. Furthermore, this infection develops into the space in the neck area to become an infection of the inner neck. If an infection occurs in the deep cervical space, negative pressure during breathing and gravity can encourage the spread of infection into the mediastinum7. About 8% of mediastinitis originate from deep neck infections that spread through the pretracheal space. More than 70% of the spread occurs through the retro visceral space, while the remaining cases occur through the perivascular space6. Generally, odontogenic infections cause inflammation through the fascia affecting the posterior mediastinum3.
Bacterial virulence factors, systemic conditions, and un-proper treatment of odontogenic infections are essential factors causing mediastinitis7. In this case, the patient did not have a history of systemic disease that could facilitate the spread of infection; in this case, the causative factors of mediastinitis could be bacterial virulence factors and late treatment of odontogenic infections. The partially impacted left mandibular molar is a possible space that promotes bacterial growth and caution infection. According to Zawislak and Nowak10, the mandibular molar was the most common odontogenic source of infection in the head and neck region. As is known, the prevalence of impacted third molars is still high11 potentially causing pericoronitis. Late treatment of pericoronitis can develop into an Oro maxillofacial abscess. Bacterial virulence plays an important role in the occurrence of mediastinitis. Most cases of mediastinitis (60-70%) are caused by Gram-positive Staphylococcus aureus and Staphylococcus epidermidis, about 40% of cases are caused by a mixture of Gram-positive and Gram-negative bacteria2. The most common aerobic bacteria that cause mediastinitis are Streptococcus pyogenes (41%) and Staphylococcus aureus (32%), while the anaerobic bacteria are Pepto streptococcus (28%), followed by Prevotella (8%)4.
Although descending necrotizing mediastinitis is rare, it has a high mortality rate of 37-60%1. Mediastinitis due to odontogenic infection was a serious complication5. Therefore, prompt diagnosis and adequate treatment can reduce the risk of death. Stabilizing the airway and controlling the source of infection is essential in treating mediastinitis. Administering broad-spectrum antibiotics and adequate drainage is the right step for treating mediatinitis12. In this case, the initial treatment for mediastinitis is administering oxygen to stabilize the patient’s airway, administration of antibiotics, and surgical incision and drainage.
Antibiotic therapy is the primary treatment of mediatinitis13. Intravenous antibiotics are effective in controlling the source of infection. Ideally, the antibiotic should match the culture and resistance test results. However, microbiological diagnostics also has weaknesses because it cannot always identify the causative pathogens with culture-based methods alone13 and requires a long time. The selection of antibiotics for this case was based on empirical evidence. In this case, the combination of Ceftriaxone and Metronidazole was administered, which is sensitive to aerobic and anaerobic bacteria. Three days after antibiotic administration, the drainage incision was made following the pus was localized. The administration of those antibiotics has responded well, so the microbiological test is unnecessary.
Effective surgical incision and drainage is the main principle of treatment of mediastinitis12. Incision and drainage management must be carried out aggressively and promptly14. In this case, the incisions were carried out in the two most volatile places of the left neck. The incision and drainage are based on the principle elimination of the infectious focus and dissection of the space along with maximum drainage. Some surgeon limit drainage and debridement to the cervical region15. The incision and drainage were successful in reducing the swelling. The result was that the patient had no complaints of shortness of breath and could open the mouth. Prompt airway management, antimicrobial therapy, surgical incision, and drainage are all important to improve the patient’s outcomes. Management of the odontogenic infection that caused mediastinitis is also important.
Mediastinitis due to odontogenic infection must be treated seriously. Prompt diagnosis and adequate treatment can reduce the risk of death. Stabilizing the airway, administering antibiotics, incision, and drainage determine the success of the treatment. Eliminating all the contributing factors of odontogenic infection is also important.
The authors would like to acknowledge the hospital staff for their immense contribution.
The authors declared no conflict of interest.
Consent was taken from the patient before writing the case report.
ZC, the consultant, supervised the whole study and helped in the final review of the case report article. YMDA is a contributor to the writing of the case report.
- Bali RK, Sharma P, Gaba S, Kaur A, Ghanghas P. A review of complications of odontogenic infections. Natl J Maxillofac Surg. 2015 Jul-Dec;6(2):136-43. Doi: 10.4103/0975-5950.183867. PMID: 27390486; PMCID: PMC4922222.
- Pastene B, Cassir N, Tankel J, Einav C, Fournier PE, Thomas P, Leone M. Mediastinitis in the intensive care unit patient: a narrative review. Clinical Microbiology and Infection 2020 26(1):26-34 doi: 10.1016/j.cmi.2019.07.005
- Kappus S, King O. Mediastinitis. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2022. PMID: 32644692.
- Kimura A, Miyamoto S, Yamashita T. Clinical predictors of descending necrotizing mediastinitis after deep neck infections. Laryngoscope. 2020 Nov;130(11): E567-E572. Doi: 10.1002/lary.28406. Epub 2019 Nov 20. PMID: 31747058.
- Escobedo, 2020 Escobedo, M. F., Junquera, L. M., Megias, J., García-San Narciso, L., Fernández, M. J., & Junquera, S. Mediastinitis of odontogenic origin. A serious complication with 80 years of history. British Journal of Oral and Maxillofacial Surgery. Volume 59, Issue 6, July 2021 683-689 doi: 10.1016/j.bjoms.2020.09.004
- Filiaci F, Riccardi E, Mitro V, Piombino P, Rinna C, Agrillo A. et al. Disseminated necrotic mediastinitis spread from odontogenic abscess: our experience Ann Stomatol (Roma) 2015 Apr-Jun; 6(2): 64-68. PMCID: PMC4525101
- Guan X, Liang X, Liang X, Wang F, Qian W, Zhang W. A new classification of descending necrotizing mediastinitis and surgical strategies. Ann Transl Med. 2021 Feb;9(4):356. Doi: 10.21037/atm-21-121. PMID: 33708983; PMCID: PMC7944333.
- Kozak-Rusinek A, Kozak K, Rusinek M, Kozakiewicz M, Kozak J. Odontogenic origin of descending necrotizing mediastinitis – controversies, multidisciplinary approach and personal experience. Arch Med Sci Civil Dis 2018; 3: e180–e183. doi: 10.5114/amscd.2018.81130
- Ogle OE. Odontogenic Infections. Dent Clin North Am. 2017 Apr;61(2):235-252. Doi: 10.1016/j.cden.2016.11.004. PMID: 28317564
- Zawislak E and Nowak R. Odontogenic Head and Neck Region Infections Requiring Hospitalization: An 18-Month Retrospective Analysis. BioMed Research International Vol 2021, Article ID 7086763, 8 pages https://doi.org/10.1155/2021/7086763
- Patil S. Impacted Mandibular Third Molars: Review of Literature and a Proposal of a Combined Clinical and Radiological Classification. Ann Med Health Sci Res. 2015; 5(4): 229–234. doi: 4103/2141-9248.160177
- Yhang JH, Jang IS, Kim SH, Park HH, Kang DH, Choi JY. A Novel Mediastinal Drainage Tube for Mediastinitis. Korean J Thorac Cardiovasc Surg. 2015;48(5):378-379. Doi:10.5090/kjtcs.2015.48.5.378
- Böttger S, Zechel-Gran S, Schmermund D, Streckbein P, Wilbrand J-F, Knitschke M, et al. Microbiome of Odontogenic Abscesses. Microorganisms. 2021; 9(6):1307. https://doi.org/10.3390/microorganisms9061307
- Skala M, Sebek J, Vodicka J,Safránek J, Geiger J, Zidkova A, et al. The Diagnostics and Treatment of Acute Mediastinitis – Single Institute Experiences. Clin Surg. 2021; 6: 3042.
- Wei D, Bi L, Zhu H, He J, Wang H. Less invasive management of deep neck infection and descending necrotizing mediastinitis: A single-center retrospective study. Medicine (Baltimore). 2017 Apr;96(15): e6590. doi: 10.1097/MD.0000000000006590.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
