By Syeda Surayya Jabeen1, Mehak Raoof2, Faria Mumtaz3, Beenish Khan4, Zubaida Shaheen5
- Head of Department, Gynae Obstetrics, CMH Kohat, Pakistan.
- Department of Gynae Obstetrics, Liaquat University of Medical & Health Sciences, Jamshoro, Pakistan.
- Classified Gynaecologist, CMH Kohat, Pakistan.
- Classified Gynaecologist, CMH Quetta, Pakistan.
- Senior Registrar, Department of Gynae Obstetrics, CMH Chunian, Pakistan.
DOI: https://doi.org/10.36283/PJMD12-3/006
How to cite: Jabeen SS, Raoof M, Mumtaz F, Khan B, Shaheen Z. Intrauterine Growth Restriction Among Pregnant Hypertensive Women of Urban and Rural Areas. Pak J Med Dent. 2023;12(3): 29-35. Doi: 10.36283/PJMD12-3/006
Background: Intrauterine growth restriction (IUGR) seems to have long-term health consequences in a newborn’s life. Hypertensive disorders of pregnancy are associated with placental blood flow and may lead to IUGR. This study aimed to determine the frequency and outcome of IUGR in hypertensive pregnant females of urban and rural areas.
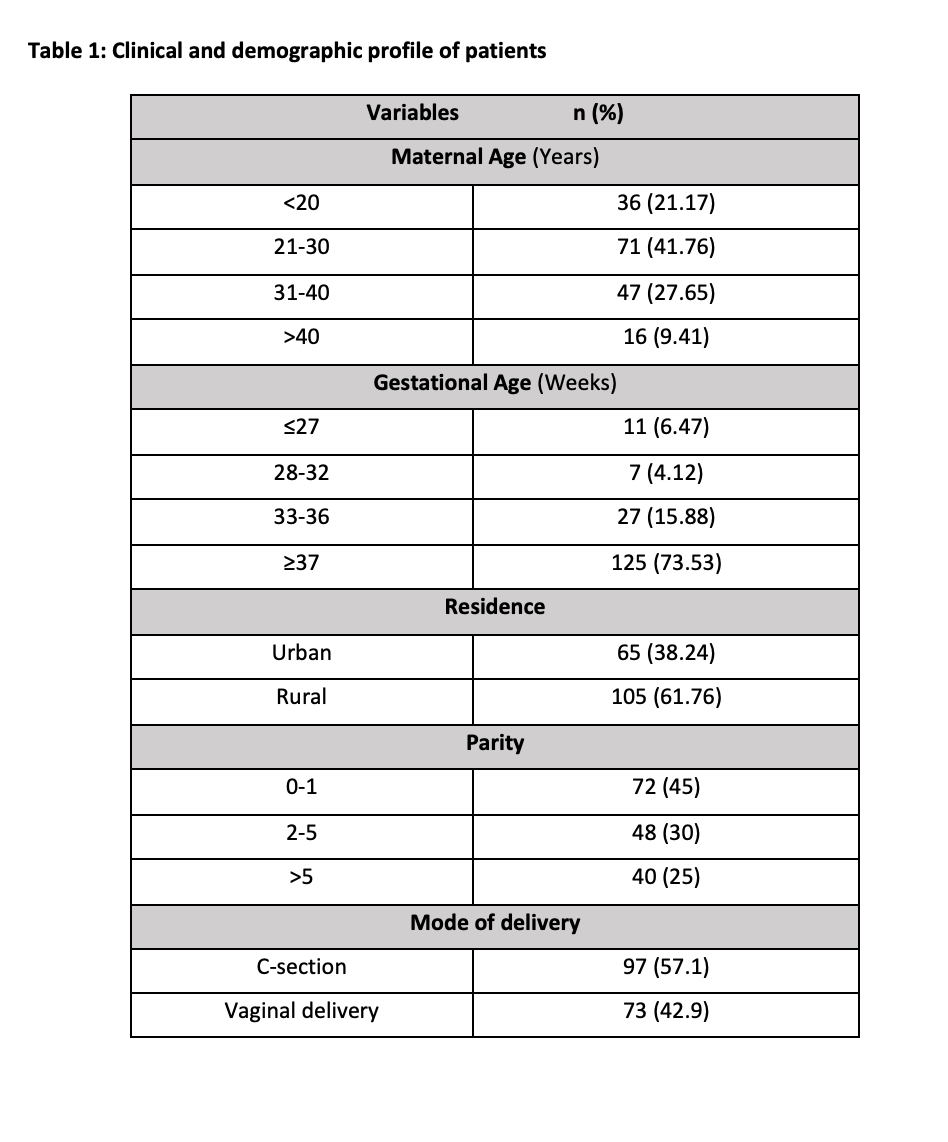
Method: This cross-sectional observational study was conducted from July 2021 to June 2022 in the Department of Gynecology & Obstetrics, CMH Kohat. All pregnant patients(n=170) of age between 18 to 45 years, either nulliparous or multiparous diagnosed with hypertensive disorders were observed for IUGR and its outcomes including appearance, pulse, grimace, activity, and respiration (APGAR) score, and stillbirth in urban and rural females. The collected data was analyzed using SPSS version 23. The stratification was performed for different variables and the Chi-square test was applied post-stratification with a confidence interval of 95% and a p-value of ≤0.05 was considered significant.
Results: Mean maternal and gestational age (mean ± SD) was 28.05±7.07 years and 36.16±3.64 weeks respectively. IUGR was detected in 110 (64.7%) babies. The outcomes observed were a low APGAR score of 42 (24.7%) and stillbirth was seen in 28 (16.46%) females. While IUGR in the urban population was 63.1% and higher in rural females at 65.71% (p = 0.80), the results were not statistically significant.
Conclusion: It was found that rural females had a high percentage of IUGR in babies which is associated with low APGAR scores and stillbirth. Therefore, timely intervention can prevent hostile consequences and growth disorders.
Keywords: Intrauterine Growth Restriction, Pregnancy Induced Hypertension, Gestational Hypertension.
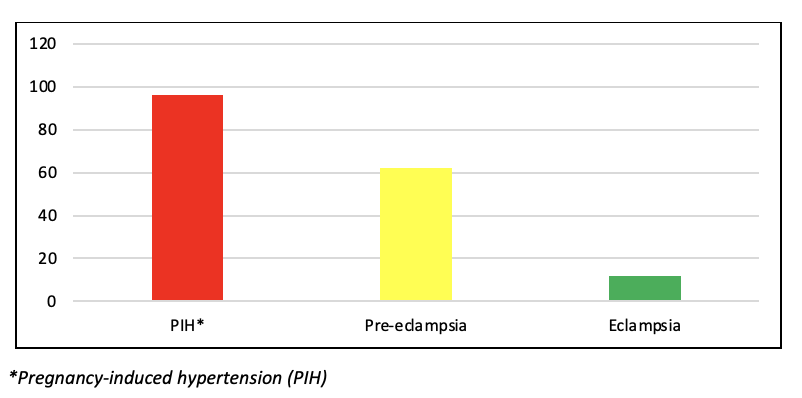
Hypertensive disorders of pregnancy are among the commonest medical disorders encountered in pregnancy and contribute greatly to fetal and maternal morbidity and mortality1. These include pregnancy-induced hypertension (PIH), pre-eclampsia, and eclampsia. The prevalence of these disorders is higher in developing countries as compared to developed countries2. A local study was conducted at a hospital in Karachi to find out the frequency of hypertensive disorders of pregnancy and was reported as high as 15%3. Hypertensive disorders of pregnancy may also adversely affect the fetus. It is associated with low birth weight, risk of admission to the intensive care unit, and even intrauterine demise. Another local study conducted in a hospital in Karachi observed that hypertensive disorders of pregnancy are one of the leading causes of stillbirths4.
The mortality from hypertensive disorders of pregnancy is very high in developing countries in comparison to developed countries and the etiology of these disorders remains elusive5. A thorough understanding of the pathogenesis of these disorders will help in managing these disorders and provide a more effective way of protecting women from the complications of these disorders, hence protecting the mother and the fetus6. Regarding the pathogenesis of the hypertensive disorders of pregnancy it is thought that it is dependent, at least to some extent, on the interaction between the surface endothelial cells in the uteroplacental circulation, maternal platelets, and the counteracting action of eicosanoids made by these tissues7. Conversely, hypertensive disorders of pregnancy and unexplained intrauterine growth restriction are a result of placental insufficiency due to placental dysfunction and result in restriction of fetal growth. The incidence of intrauterine growth restriction is around 5% in the general obstetric population whereas the prevalence of IUGR in patients of PIH is around 28% 8-9. Rationale of this study was to measure the IUGR and its outcomes in pregnant women with hypertensive disorders in the local population. With the help of this study, we’ll be able to gather local data and devise local guidelines and better preventive antenatal measures so that the patients may be managed in a more effective way. Therefore, the study aimed to find out the frequency and outcome of IUGR in hypertensive disorders of pregnancy in urban and rural females.
This was a cross-sectional observational study, conducted in the Department of Obstetrics & Gynecology, CMH Kohat, from July 2021 to June 2022 after approval from the Ethical Review Committee of this Hospital (ERC Ref No. E-2005/A/10). The sample size (n=170) was calculated with the help of an online sample size calculator10, with the prevalence of IUGR in hypertensive disorders of pregnancy at 19%, 11 margins of error of 5%, and a confidence level of 95%. The same size came out to be 168 and was rounded off to 170 patients. The technique used for sampling was non-probability consecutive sampling.
All pregnant patients with age between 18 to 45 years, either multiparous or nulliparous diagnosed with hypertensive disorders of pregnancy were included in this study. Hypertensive disorders of pregnancy were defined as new onset hypertension that occurred after 20 weeks of gestation. Patients with a history of transient or chronic hypertension with or without proteinuria and patients with a history of ischemic heart disease and chronic kidney disease were excluded from this study. Pregnant women fulfilling the inclusion criteria were enrolled for this study after signing the informed consent. All the patients diagnosed with hypertensive disorders of pregnancy were observed for IUGR and outcomes including stillbirth and low APGAR score (APGAR less than 7 at 5 minutes). A detailed history was taken along with carrying out the detailed clinical examination by researchers. Ultrasonography was done by a consultant sinologist. A pre-designed proforma was used to collect all the data.
SPSS version 23 was used to analyze the collected data. The frequencies and percentages were calculated for a place of residence, parity, maternal age, gestational age, mode of delivery, IUGR, and different outcomes in hypertensive disorders of pregnancy. Mean and standard deviations (SD) were computed for parity, gestational age, maternal age, and APGAR score. The stratification was performed for parity, gestational age, maternal age, mode of delivery (simple vaginal delivery or C-section), and residence (urban or rural) to observe the effects on the outcome. The chi-square test was applied post-stratification on categorical variables with a confidence interval of 95% and a p-value of ≤0.05 was considered statistically significant.
During one year period of this study, 170 patients diagnosed with hypertensive disorders of pregnancy were evaluated for IUGR. The frequency of types of hypertensive disorders is shown in Figure 1.
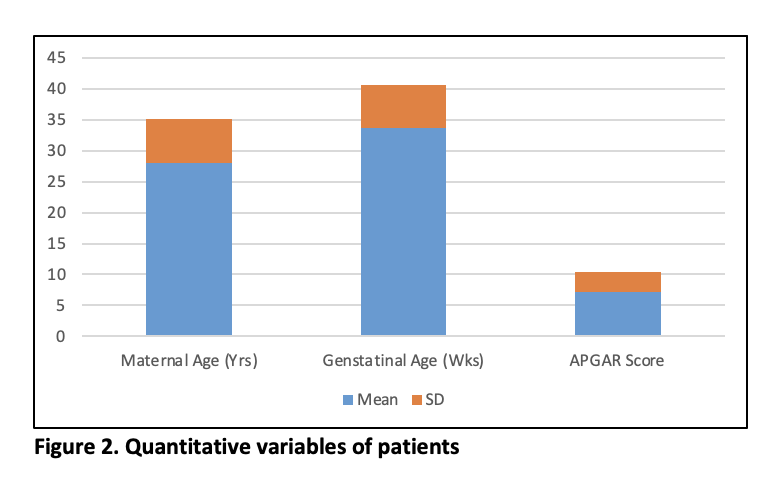
The maternal age ranged from 18-43 years with a mean ± SD of 28.05±7.07. Mean and SD for gestational age (weeks) and APGAR score and parity were 36.16±3.64, 7.11±3.47, and 2.63±2.4 respectively. The mean ± SD for the quantitative variables is shown in Figure 2. The demographical data and clinical profile of the patients are shown in Table 1. A comparison of urban and rural populations is shown in Table 2.
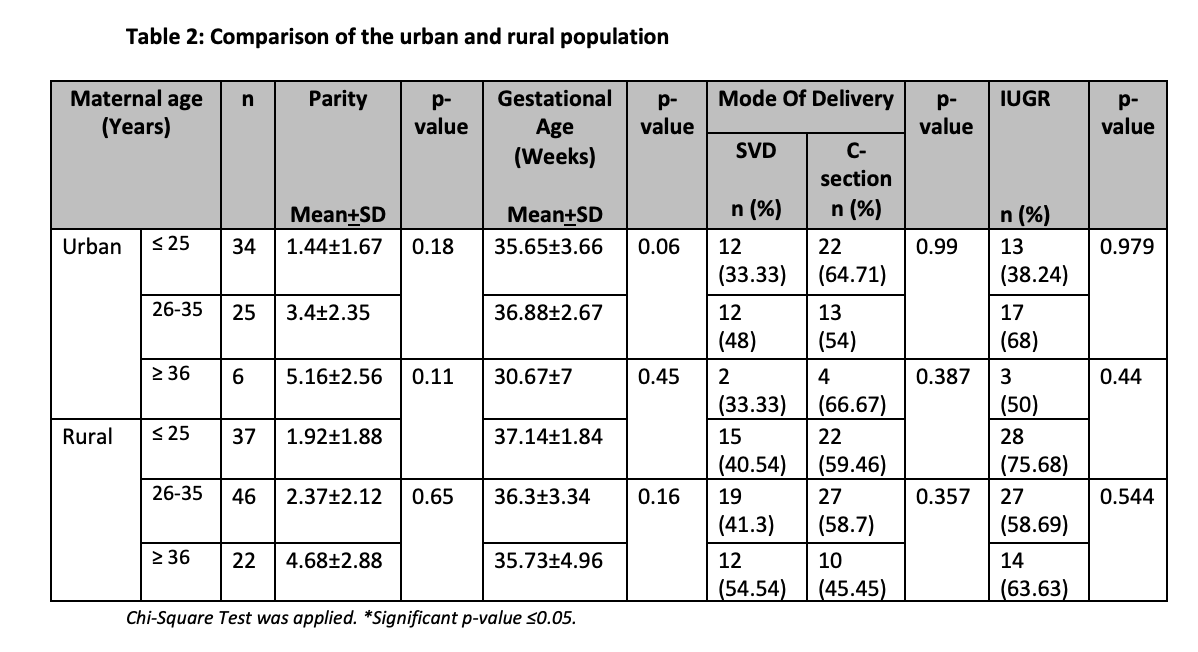
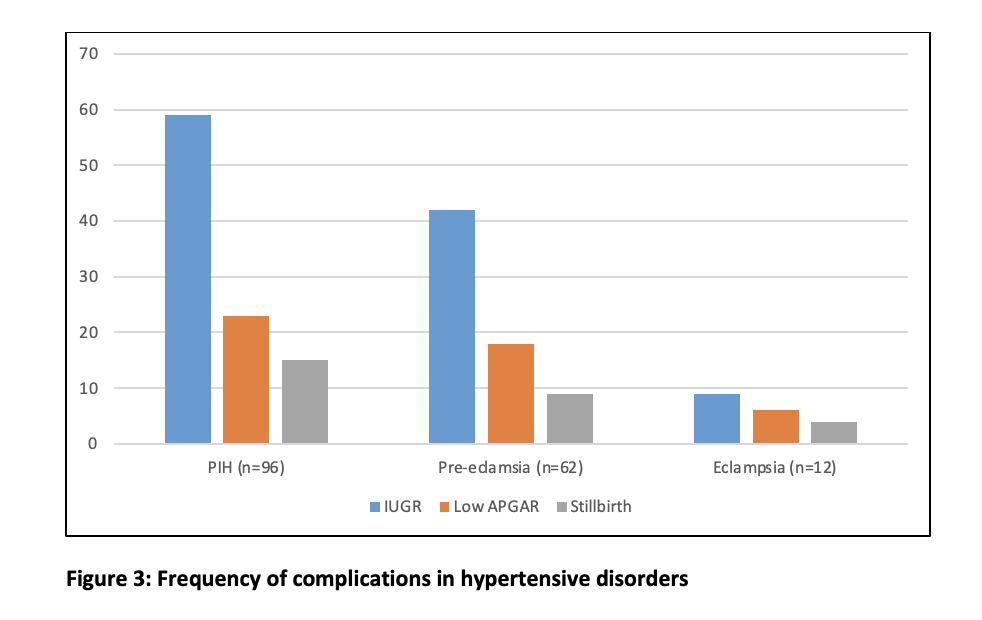
Regarding the IUGR in relation to maternal age, 66.66% (19-20 years), 66.19% (21-30 years), 63.63% (31-40 years), and 50% (over 40 years) (p= 0.91). The IUGR in relation to gestational age was 60% (30 weeks or less) and 65.2% (31 weeks or more) (p = 0.93) while the IUGR in context to urban residence was 63.1% and rural residence was 65.71% ([p= 0.80). The IUGR in context to parity was nulliparous 63.1% and multiparous 61.8% (p = 0.91) while the IUGR in context to the mode of delivery c section 60.82% and vaginal delivery 69.87% (p= 0.77). The IUGR was detected in 110 (64.7%) babies. The observed outcomes were low APGAR scores of 42 (24.7%) and stillbirth was 28 (16.46%). The frequency of various complications in different hypertensive disorders of pregnancy is shown in Figure 3.
Hypertensive disorders of pregnancy can lead to many complications which include but are not limited to premature delivery, IUGR, placental abruption, HELLP syndrome, stroke, and myocardial infarction 12-15. The risk of morbidity and mortality of the mother and the fetus due to these complications warrants timely diagnosis and management of these disorders. As compared to uneventful pregnancies, pregnancies with hypertensive disorders may lead to increased morbidity and mortality of the mother and the fetus. IUGR seems to be the prime complication of the fetus in pregnancies complicated with hypertensive disorders16. The exact cause is not fully understood but it is believed that it may be related to malfunction of the blood vessels in the placenta. Hypertensive disorders of pregnancy lead to vasoconstriction of the blood vessels present in the placenta and result in reduced placental blood flow. This in turn results in a reduced supply of nutrients and oxygen to the fetus leading to growth restriction. Hypertensive disorders of pregnancy are more prevalent in primigravida and perhaps the main reason for the IUGR and reduced weight of the placenta17. In this study, the IUGR was seen in 110 (64.7%) patients, out of these 29 (26.36%) were nulliparous and the remaining 81 (73.63%) were multiparous, this is comparable with the study conducted by Arwan B et al 18. Contrary to this, in another study, IUGR was seen in 57.5% of primigravida and while it was 42.5% in multigravida 19.
In our study we found out the incidence of IUGR in urban and rural populations was statistically non-significant; which was 63.1% for urban and 65.71% for rural residents. Contrary to this finding, in a study conducted by Iranian researchers, it was concluded that pregnant ladies belonging to rural areas are at higher risk of IUGR, preterm birth, post-term pregnancy, need for neonatal resuscitation, and NICU admissions20. In the current study, we observed that the incidence of IUGR in the hypertensive disorder of pregnancy in relation to maternal age is evenly distributed in all age groups. However, various national and international studies have yielded a wide variety of results. A similar study conducted by Villar J et al. concluded that the incidence of IUGR is more common in extremes of maternal age21. In a local study conducted at Aga Khan Hospital Karachi by Pakistani researchers, found that complication of IUGR in hypertensive disorders of pregnancy is associated with young maternal age22. Rubinshtein AM et al concluded in their study that IUGR is commonly associated with advanced maternal age 23.
The hypertensive disorders of pregnancy also adversely affect the APGAR score as well. The present study results showed a low APGAR score of 24.7%. Our results are comparable to another similar study conducted by Aftab S et al. 24 In their study the low APGAR score was seen in 24.7%. Stillbirth is another sequela of hypertensive disorders. In our study stillbirth was seen in 16.46% of patients. A similar rate of stillbirth (15.5 %) was seen in a study conducted by Lugobe HM et al. 25 Hypertensive disorders in pregnancy are quite common and are associated with various outcomes which necessitate their timely diagnosis and proper management to reduce the adverse outcomes.
The strength of this study was that it covered the rural and urban population of the KPK province of Pakistan and had an ample sample size and covered an age group from eighteen to 43 years. A possible weakness of the study was patients recruited for this study belonged to only one region of Pakistan and results cannot be generalized for the Pakistani population, it is therefore suggested that a similar multicenter study on a larger scale with at least covering two to three provinces be conducted for more accurate results.
The study found that rural females had a high percentage of IUGR in babies. As IUGR is one of the most frequently encountered sequelae of hypertensive disorders. It is associated with low APGAR scores and stillbirth. Assessment of growth disorder can be easily done in modern-day obstetrics and timely intervention can prevent the hostile consequences.
The authors would like to acknowledge the hospital and staff for their support throughout the study.
All authors confirm that there is no conflict of interest.
The ethical committee of CMH Kohat approved to carry out of this study (ERC Ref No. E-2005/A/10).
Consent was signed by all participants willing to take part in this study.
SSJ did conception and design, acquisition of data, analysis, and interpretation of data, drafting the article, and overall supervision of the research project. MR did the conception and design, analysis, and interpretation of data, drafting of the article, and critical revision. FM also did conception and design, acquisition of data, analysis, and interpretation of data, and drafting of the article. BK designed and conception, analyzed, and interpretation of data, critical revision. ZS conception and design, analysis interpretation of data and critical revision
- Folk DM. Hypertensive disorders of pregnancy: Overview and current recommendations. Journal of Midwifery & Women’s Health. 2018; 63(3):289-300. doi:10.1111/jmwh.12725
- Malik A, Jee B, Gupta SK. Preeclampsia: Disease biology and burden, its management strategies with reference to India. Pregnancy Hypertension. 2019; 15(1):23-31. doi: 10.1016/j.preghy.2018.10.011
- Shah N, Hossain N, Shoaib R, Hussain A, Gillani R, Khan NH. Socio-demographic Characteristics and the Three Delays of Maternal Mortality. J Coll Physicians Surg Pak.2009; 19:95-8
- Korejo R, Bhutta S, Noorani KJ, Bhutta ZA. An audit and trends of perinatal mortality at the Jinnah Postgraduate Medical Centre, Karachi. J Pak Med Assoc.2007; 57:168-72.
- Utami SH, Handayani F, Mam. Ecological analysis of Preeclampsia/Eclampsia case in Sidoarjo Regency, Indonesia, 2015-2019. Indian Journal of Forensic Medicine & Toxicology. 2020; 14(4): 3474–3479. doi:10.37506/ijfmt. v14i4.12164
- Socha MW, Malinowski B, Puk O, Dubiel M, Wiciński M. The NLRP3 Inflammasome role in the pathogenesis of pregnancy induced hypertension and Preeclampsia. Cells. 2020; 9(7):1642. doi:10.3390/cells9071642
- Palei AC, Spradley FT, Warrington JP, George EM, Granger JP. Pathophysiology of hypertension in preeclampsia: a lesson in integrative physiology. Acta Physiol (Oxf).2013;208(3):224-33
- Seyom E, Abera M, Tesfaye M, Fentahun N. Maternal and fetal outcome of pregnancy related hypertension in Mettu Karl Referral Hospital, Ethiopia. J Ovarian Res.2015; 8:10-15
- Gortner L. Intrauterine growth restriction and risk for arterial hypertension: a causal relationship?. J Perinat Med.2007;35(5):361-5.
- Sample size calculator. (n.d.). Retrieved from https://www.calculator.net/sample-size-calculator.html
- Elghoudi A, Alsharef A, Elghoudi A. A cross-sectional study on current practice of the management of pregnancy-induced hypertension and its maternal and foetal complications and outcome in the western part of the state of Libya. Open Journal of Obstetrics and Gynecology. 2022; 12(03):222-241. doi:10.4236/ojog.2022.123022
- Leeman L, Dresang LT, Fontaine P. Hypertensive Disorders of Pregnancy. American family physician. 2016; 93(2):121–127.
- Wu P, Jordan KP, Chew-Graham CA, Coutinho T, Lundberg GP, Park KE, et al. Temporal trends in pregnancy-associated stroke and its outcomes among women with hypertensive disorders of pregnancy. Journal of the American Heart Association. 2020; 9(15):e016182. https://doi.org/10.1161/JAHA.120.016182
- Ford ND, Cox S, Ko JY, Ouyang L, Romero L, Colarusso T, et al. Hypertensive disorders in pregnancy and mortality at delivery hospitalization – United States, 2017-2019. MMWR. Morbidity and Mortality Weekly Report. 2022; 71(17):585–591. https://doi.org/10.15585/mmwr.mm7117a1
- Mersha AG, Abegaz TM, Seid MA. Maternal and perinatal outcomes of hypertensive disorders of pregnancy in Ethiopia: systematic review and meta-analysis. BMC Pregnancy and Childbirth. 2019; 19(1):458. https://doi.org/10.1186/s12884-019-2617-8
- Wilkerson RG, Ogunbodede AC. Hypertensive disorders of pregnancy. Emergency Medicine Clinics of North America. 2019; 37(2):301-316. doi: 10.1016/j.emc.2019.01.008
- Patel H, Shah PT, Shah A, Patel SV, Deliwala dj. oligohydramnios: -a common problem with increasing incidence in term pregnancy and its fetomaternal outcome. bjkines-njbas. 2021; 13(1):68-73.
- Arwan B, Sriyanti R. Relationship between Gravida Status, Age, BMI (Body Mass Index) and Preeclampsia. Andalas Obstetrics and Gynecology Journal. 2020; 4(1):13-21. DOI: https://doi.org/10.25077/aoj.4.1.13-21.2020
- Gluhovschi G, Gluhovschi A, Petrica L, Anastasiu D, Gluhovschi C, Velciov S. Pregnancy-induced hypertension–a particular pathogenic model. Similarities with other forms of arterial hypertension. Rom J Intern Med.2012;50(1):71-81.
- Mehrnoush V, Ranjbar A, Banihashemi F, Darsareh F, Shekari M, Shirzadfardjahromi M. Urban-rural differences in the pregnancy-related adverse outcome. Gynecology and Obstetrics Clinical Medicine. 2023; 3(1):51-55. doi:10.21203/rs.3.rs-1827244/v1
- Villar J, Carroli G, Wojdyla D, Abalos E, Giordano D, Ba’aqeel H et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? American Journal of Obstetrics and Gynecology. 2006; 194(4):921-931. doi: 10.1016/j.ajog.2005.10.813
- Mohammad N, Sohaila A, Rabbani U, Ahmed S, Ahmed S, Ali SR. Maternal predictors of intrauterine growth retardation. J Coll Physicians Surg Pak. 2018; 28(9):681–685. https://doi.org/10.29271/jcpsp.2018.09.681.
- Rubinshtein AM, Golyanovskiy OV. Obstetric outcomes in women of advanced maternal age after assisted reproduction. Clin Exp Obstet Gynecol. 2021; 48(4),893-900.
- Aftab S, Ayaz S, Hussain SF, Hussain AS. Frequency and outcome of Intrauterine Growth Restriction (IUGR) in pregnancy induced hypertension. Pak J Surg 2022; 38(3):201-206.
- Lugobe HM, Muhindo R, Kayondo M, Wilkinson I, Agaba DC, McEniery C et al. Risks of adverse perinatal and maternal outcomes among women with hypertensive disorders of pregnancy in southwestern Uganda. PLOS ONE. 2020; 15(10):e0241207. doi: 10.1371/journal.pone.0241207
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
