By Peni Pujiastuti1, Yuliana Mahdiyah Daat Arina1, Depi Praharani1, Melok Aris Wahyukundari1, Neira Najatus Sakinah1, Desi Sandra Sari1
- Periodontology Department, Faculty of Dentistry, Jember University, Jember, Indonesia.
DOI: https://doi.org/10.36283/PJMD12-3/002
How to cite: Pujiastuti P, Arina YMD, Praharani D, Wahyukundari MA, Sakinah NN, Sari DS. Health Profile of Periodontal Tissue of Pregnant Women in The Agromedical Dental Community in Jember District. Pak J Med Dent. 2023;12(3): 3-8. Doi: 10.36283/PJMD12-3/002
Background: Periodontal disease is a disease found worldwide and the prevalence of periodontal disease is around 75% in Jember Regency in pregnant women. Periodontal disease during pregnancy is a risk factor for low birth weight. Therefore, it is crucial to study the ways of maintaining oral hygiene in pregnant women to prevent periodontal disease in pregnant women. The aim of this study was to determine the health profile of the periodontal tissue of pregnant women in the dental agromedical community in the Jember Regency.
Methods: This research is a descriptive observational survey-based study. The study population was pregnant women(n=50) in the 1st-3rd trimester, aged 20-30 years, and were having a pregnancy checkup at the MCH polyclinic of the Integrated Service Post in the Coastal area (Puger area) and the Plantation area (Renteng area). Gingival status was examined using the Gingival Index (GI), periodontal health status using the Community Periodontal Index of Treatment Need (CPITN), and oral hygiene status using the Oral Hygiene Index-Simplified (OHI-S).
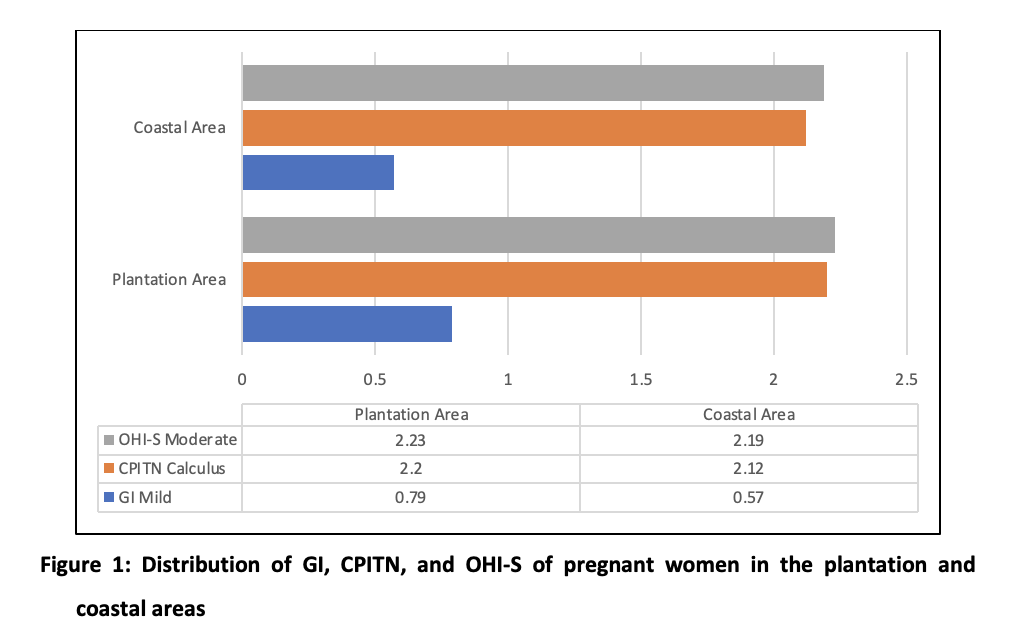
Results: The research results showed that the average CPITN was 2.20 in the plantation area and 2.12 in the coastal area which showed the presence of calculus and no presence of pockets. A score of 3 indicates that the gingiva has a sulcus depth of 4-5 mm and in this case, there was no presence of a pocket but edema in the gingiva was found.
Conclusion: This study concluded that pregnant women in the coastal area had mild gingivitis and calculus with no presence of pockets in the plantation area.
Keywords: Oral Health, Gingival Index, Pregnant Women, Periodontal Index
Periodontal disease is the most common oral health disease that is being experienced all around the world. It was estimated in a recent study on the Global Burden of Diseases, that around 3.5 billion people are affected by oral diseases, and nearly 10% population was estimated to be affected by severe periodontitis1. For the prevention of oral diseases, regular dental care and timely corrective actions are necessary2.
During pregnancy, the physiological functions of women experience various changes that let their body to adjust to the new pregnancy environment. The changes in hormones during pregnancy, specifically elevation in Progesterone and Estrogen levels, as well as in dietary and hygiene habits make them more susceptible to oral diseases3. Similarly, periodontal disease is also a risk factor for premature birth and low birth weight (LBW). Huck et al proposed that periodontal disease can be linked to increased preterm birth risk, however, there is uncertain evidence to support the association and this debate can still be found in the published literature4. It has been suggested in previous research that infections of periodontium can act as a reservoir for inflammatory mediators, and therefore, might be a hazard to the fetal placental component and thus are related to adverse outcomes of pregnancy such as Low birth weight babies and preterm birth 5. The periodontitis possible impact as a risk factor for LBW necessitates additional studies and recommends a potential need for preventive measures to be taken for pregnant women along with better collaboration between dental professionals and obstetrical 6.
This can be done by examining their oral health using the Oral Hygiene Index-Simplified (OHI-S) and the Community Periodontal Index of Treatment Need (CPITN)7. The purpose of using CPITN is to obtain data on the periodontal status of the community, to plan outreach programs, to determine treatment needs which include the type of action, the amount of workload, and energy requirements, and to monitor the progress of individual periodontal conditions. GI is an index to determine the degree of gingival inflammation or gingivitis8.
Therefore, care management of oral health in pregnant women is required to be implemented as soon as possible to decrease the common oral disease incidences in pregnant women and also pregnancy adverse outcomes risk9,10. However, limited pregnant women actively seek examinations of their oral health after the start of pregnancy, and also there is inadequate awareness regarding oral health during pregnancy even among healthcare experts11,12,13. It was shown in a study that oral health education during pregnancy helps in improving their knowledge and attitude14. Hence, epidemiological data are needed to see the distribution and pattern of periodontal disease in pregnant women so that planned preventive, curative, and rehabilitative efforts can be equally integrated into the community. The purpose of this study was to determine the periodontal tissue health profile of pregnant women in the dental agromedicine community in Jember Regency.
This research is a descriptive observational study with a cross-sectional approach. The sampling technique used was purposive sampling with a total of 50 research subjects in the coastal area of Puger and 50 in the plantation area of Renteng in the Jember Regency. The population of this study was pregnant women in the 1st – 3rd trimester aged 20-30 years, who were having a pregnancy check-up at the MCH polyclinic of the Integrated Service Post in the coastal and plantation areas. The ethical clearance for this study was approved by the Dentistry Research Ethics Commission of Jember University No. 1625/UN25.8/KEPK/DL/2022.
Before being examined, informed consent was obtained from the pregnant women along with the questionnaire. Furthermore, the gingival health status was examined using the Gingival Index (GI), periodontal health status using the Community Periodontal Index of Treatment Need (CPITN), and oral hygiene status using the Oral Hygiene Index-Simplified (OHI-S). The results were tabulated and described by calculating the percentage of each variable of periodontal tissue status in the coastal and plantation.
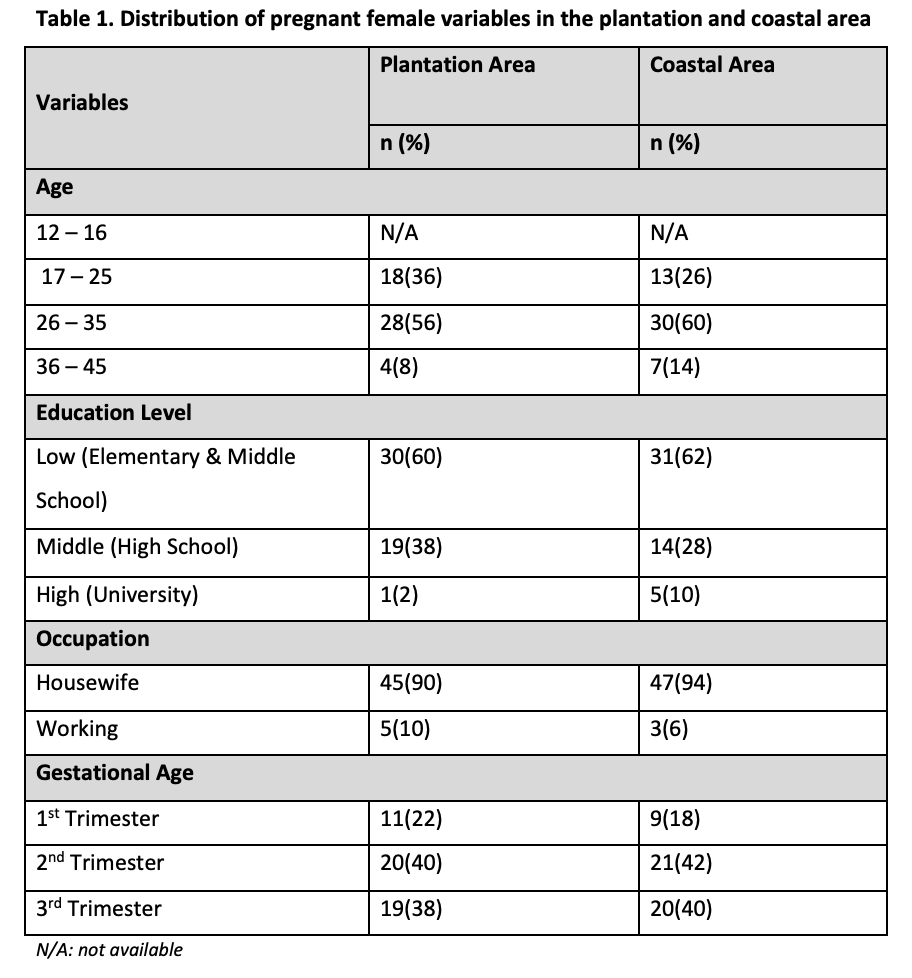
The examination results of 50 pregnant women in the plantation area and 50 in the coastal area showed the following characteristics: the pregnant women were mostly aged 26-35 years (Table 1), with a mostly low level of education, and based on the gestational age, the pregnant women in both areas were mostly in the 2nd trimester.
The results of this study showed that in the plantation and coastal areas, the average gingival status (GI) in pregnant women fell under the criteria of mild inflammation or mild gingivitis. The average periodontal health status (CPITN) in pregnant women fell under the criteria of calculus and no pockets (< 3mm). Meanwhile, the average level of oral hygiene (OHI-S) was under moderate criteria (Figure 1).
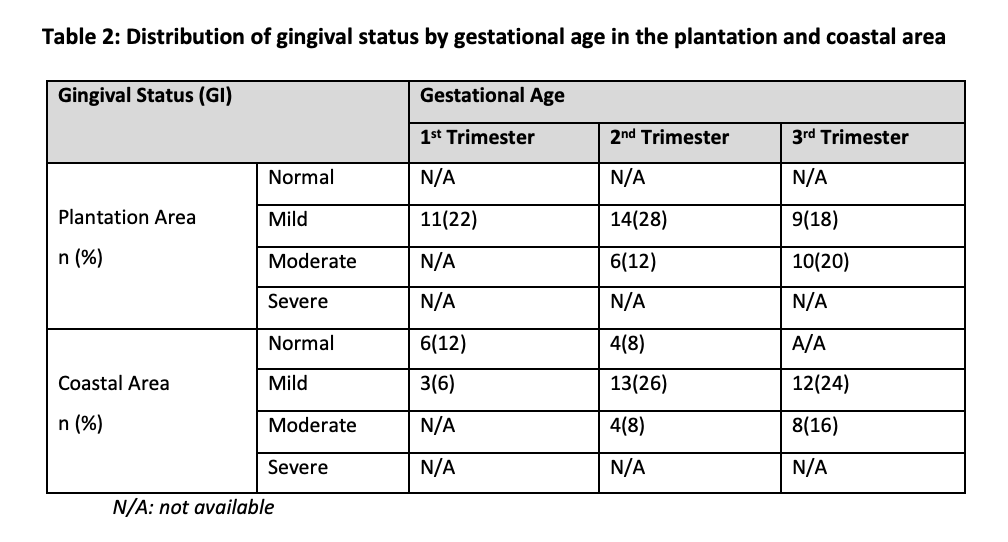
The gingival status in Plantation and Coastal areas showed mostly mild inflammation for all three trimesters. This means that on average, pregnant women in these areas experienced mild gingivitis (Table 2). In the plantation area, many pregnant women in the 1st and 2nd trimesters experienced mild inflammation, while in the 3rd trimester experienced moderate inflammation. In the coastal area, it was found that many pregnant women in 1st trimester showed normal conditions, while in the 2nd and 3rd trimesters showed mild inflammation.
The periodontal health status based on gestational age showed that in the plantation and coastal areas, the periodontal health status of pregnant women in the 1st, 2nd, and 3rd trimesters mostly had a score of 2, which means there was a presence of calculus and there was no presence of pockets (<3mm) (Table 3). A score of 3 indicates that the gingiva has a sulcus depth of 4-5 mm and in this case, there was no presence of a pocket but edema in the gingiva was found.

The pregnancy process can be influenced by periodontal health, and vice versa. In other words, periodontal diseases not only interfere with pregnancy but also gets worse during pregnancy because of certain alterations in physiology15. Gingival inflammation in pregnant women increases along with gestational age. This is caused by dental plaque as the main cause of gingival inflammation and is exacerbated by progesterone and estrogen hormones. Table 1 shows that the pregnant women were mostly aged 26-35 years, the productive ages for women. These results are in line with Arina et al. who found that most pregnant women were aged 26-35 years.16 Also, the gingival status of pregnant women in the Plantation and Coastal areas showed mild inflammation. This means that on average, pregnant women in these areas experienced mild gingivitis (Table 2). In the plantation area, based on gestational age, it was found that many pregnant women in the 1st and 2nd trimesters experienced mild inflammation, while many in the 3rd trimester experienced moderate inflammation. In the coastal area, based on gestational age, it was found that many pregnant women in the 1st trimester showed normal conditions, while in the 2nd and 3rd trimesters showed mild inflammation. This is also because the majority of pregnant women in the coastal area (83%) consume saltwater fish every day. Saltwater fish contain abundant omega 3 which has anti-inflammatory properties. Pregnant women who consumed morhaveea fish have a lower risk of having gingival inflammation. According to El-Sharkawy et.al, omega-3 fatty acids have therapeutic and anti-inflammatory agents and are used as a protective measure against various diseases including periodontitis17.
The periodontal health status of pregnant women in the Plantation and Coastal areas showed the presence of calculus and no pockets (< 3mm). This is due to the influence of the progesterone and estrogen hormones which cause pregnant women in early gestational age to experience nausea and vomiting that affect the oral cavity. These hormone levels wildly fluctuate during pregnancy and reach peak plasma levels by the third trimester, making the host more vulnerable to periodontal diseases18,19. This situation will increase plaque build-up, thereby worsening the dental and oral hygiene levels of pregnant women.
In addition, changes in the progesterone and estrogen hormones will affect the dilatation of the gingival blood vessels so that the gingiva is more prone to plaque bacteria. According to Maybodi et al, the severity of gingivitis increases due to an increase in prostaglandin E2 (PGE2) synthesis in the gingival sulcus fluid and vascular permeability, as well as a decrease in the chemotaxis and phagocytosis of polymorphonuclear which suppresses the immune response of the periodontal tissue to plaque as a reaction to high levels of the progesterone and estrogen along with the increasing gestational age20.
Oral hygiene can also be influenced by the level of education. Based on the educational background (Table 1), it was found that in the Plantation and Coastal area, 60-62% of the pregnant woman with periodontal disease attended Primary or Junior High school. These results are in accordance with Umniyati et al, who found that pregnant women with low levels of education have a greater chance of experiencing gingivitis and periodontitis because a lack of education can also mean a lack of knowledge about oral hygiene practices in pregnant women21. In addition, this can also be influenced by the type of occupation. The study showed that in the plantation and coastal areas, most pregnant women with periodontal disease were housewives (90-94%) (Table 1) and had never visited a dentist (90-92%). According to Uwambaye et al, in Rwanda, the socio-economic status and occupation of pregnant women are significantly related to periodontitis due to the inability to maintain dental hygiene through toothbrushes and toothpaste purchases. Consequently, they are susceptible to poor oral hygiene and the inability to pay for dental care22.
The gingival status in the plantation and coastal areas showed that pregnant women in the 1st trimester started to experience gingival inflammation/mild gingivitis. As for the periodontal health status, pregnant women in the 1st trimester began to form calculus and it was mostly experienced during the 2nd trimester. These data can be used as a basis for the implementation of preventive programs from the early age of pregnancy. Meanwhile, curative programs can be carried out in the 2nd trimester. The 2nd trimester is a safe time for dental and oral care because they will not interfere with fetal development. 23
This study disclosed that participating pregnant women in the plantation and coastal areas had mild gingivitis, and calculus, with no presence of pockets (< 3mm). The implementation of preventive programs can be started in the 1st trimester and curative programs can be carried out in the 2nd trimester.
The author would like to extend our uttermost gratitude to the Institute of Research and Community Services of the University of Jember.
All the authors hereby declare that there is no conflict of interest.
This study was approved by the Dentistry Research Ethics Commission of Jember University No. 1625/UN25.8/KEPK/DL/2022.
Verbal and written informed consent was obtained from all patients.
This research was funded by Research Grant No 4083/UN25.3.1/LT/2022 for Research Group (KeRis) at Jember University in 2022.
PP: Conceptualization; Data curation; Formal analysis. YMDA: Funding acquisition; Investigation; Methodology. DP: Project administration; Resources. MAW: Software; Supervision; Validation. NNS: Visualization; Roles/Writing – original draft. DSS: Roles/Writing – original draft; Writing – review & editing. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
- Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, Listl S, Celeste RK, Guarnizo-Herreño CC, Kearns C, Benzian H, Allison P, Watt RG. Oral diseases: a global public health challenge. Lancet. 2019 Jul 20;394(10194):249-260. doi: 10.1016/S0140-6736(19)31146-8.
- Kumar S. Evidence-Based Update on Diagnosis and Management of Gingivitis and Periodontitis. Dent Clin North Am. 2019 Jan;63(1):69-81. doi: 10.1016/j.cden.2018.08.005.
- Fakheran O, Keyvanara M, Saied-Moallemi Z, Khademi A. The impact of pregnancy on women’s oral health-related quality of life: a qualitative investigation. BMC Oral Health. 2020 Oct 27;20(1):294. doi: 10.1186/s12903-020-01290-5
- Huck O, Tenenbaum H, Davideau JL. Relationship between periodontal diseases and preterm birth: recent epidemiological and biological data. J Pregnancy. 2011; 2011:164654. doi: 10.1155/2011/164654.
- Haerian-Ardakani A, Eslami Z, Rashidi-Meibodi F, Haerian A, Dallalnejad P, Shekari M, Moein Taghavi A, Akbari S. Relationship between maternal periodontal disease and low birth weight babies. Iran J Reprod Med. 2013 Aug;11(8):625-630.
- Saini R, Saini S, Saini SR. Periodontitis: A risk for delivery of premature labor and low birth weight infants. J Nat Sci Biol Med. 2011 Jan;2(1):50-52. doi: 10.4103/0976-9668.82321.
- Soulissa, A. G. Hubungan kehamilan dan penyakit periodontal (Relationship between pregnancy and periodontal disease). Jurnal PDGI 2014, 63(3), 71–77.
- Iheozor-Ejiofor Z, Middleton P, Esposito M, Glenny AM. Treating periodontal disease for preventing adverse birth outcomes in pregnant women. Cochrane Database Syst Rev. 2017 Jun 12;6(6):CD005297. doi: 10.1002/14651858.
- Yenen Z, Ataçağ T. Oral care in pregnancy. Journal of the Turkish German Gynecological Association. 2019 Dec;20(4):264.
- American College of Obstetricians and Gynecologists. Oral health care during pregnancy and through the lifespan. Committee Opinion No. 569. Obstet Gynecol. 2013 Aug;122(2):417-22.
- Sharif S, Saddki N, Yusoff A. Knowledge and attitude of medical nurses toward oral health and oral health care of pregnant women. The Malaysian journal of medical sciences: MJMS. 2016 Jan;23(1):63.
- Hoerler SB, Jenkins S, Assad D. Evaluating Oral Health in Pregnant Women: Knowledge, attitudes and practices of health professionals. American Dental Hygienists’ Association. 2019 Feb 1;93(1):16-22.
- Al Khamis S, Asimakopoulou K, Newton JT, Daly B. Oral health knowledge, attitudes, and perceptions of pregnant Kuwaiti women: a qualitative study. JDR Clinical & Translational Research. 2016 Oct;1(3):211-7.
- Chawla RM, Shetiya SH, Agarwal DR, Mitra P, Bomble NA, Narayana DS. Knowledge, Attitude, and Practice of Pregnant Women regarding Oral Health Status and Treatment Needs following Oral Health Education in Pune District of Maharashtra: A Longitudinal Hospital-based Study. The journal of contemporary dental practice. 2017 May 1;18(5):371-7.
- Kapila YL. Oral health’s inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 2000. 2021 Oct;87(1):11-16. doi: 10.1111/prd.12398
- Arina D. Saputri, dan C. F. Novita. Gambaran Status Gingiva Pada Ibu Hamil di Rumah Sakit Umum Merauxa Banda Aceh. Journal Caninus Dentistry 2017, 02: 4.
- El-Sharkawy H, Aboelsaad N, Eliwa M, Darweesh M, Alshahat M, Kantarci A, Hasturk H, Van Dyke TE. Adjunctive treatment of chronic periodontitis with daily dietary supplementation with omega-3 Fatty acids and low-dose aspirin. J Periodontol. 2010 Nov;81(11):1635-1643. doi: 10.1902/jop.2010.090628
- Bobetsis YA, Graziani F, Gürsoy M, Madianos PN. Periodontal disease and adverse pregnancy outcomes. Periodontol 2000. 2020 Jun;83(1):154-174. doi: 10.1111/prd.12294.
- Figuero E, Han YW, Furuichi Y. Periodontal diseases and adverse pregnancy outcomes: Mechanisms. Periodontol 2000. 2020 Jun;83(1):175-188. doi: 10.1111/prd.12295.
- Rashidi Maybodi F, Haerian-Ardakani A, Vaziri F, Khabbazian A, Mohammadi-Asl S. CPITN changes during pregnancy and maternal demographic factors ‘impact on periodontal health. Iran J Reprod Med. 2015 Feb;13(2):107-112.
- Umniyati H, Amanah SP, Maulani C. Hubungan gingivitis dengan faktorfaktor risiko pada ibu hamil. Padjadjaran J Dent Res Student 2020, 4(1):36-42. doi: 10.24198/pjdrs. v3i2. 26086
- Uwambaye P, Kerr M, Rulisa S, Harlan S, Munyanshongore C. Prevalence of periodontitis and associated factors among pregnant women: a cross-sectional survey in Southern Province, Rwanda. Rwanda J Med Heal Sci 2021, 4(1):131-150. Doi:10.4314/rjmhs. v4i1.10
- Newman, M. G., Takei, H. H., & Klokkevold, P. R.(. Newman and Carranza’s Clinical Periodontology thirteenth edition Philadelphia: Elsevier Inc. 2019.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
