By Imrana Saeed 1, Maryam Sadiq 2, Faizan Fazal2, Alishba Shezal Ali 2, Fatimah Shahid 2, Muniba Zafar 2, Noor Mahal Azam2, Qurat Ul Ain2, Manahil Nazir2, Ayesha Noor2
- Department of Community Medicine, Rawalpindi Medical University, Rawalpindi, Pakistan.
- Final year MBBS, Department of Medicine, Rawalpindi Medical University, Rawalpindi, Pakistan.
DOI: https://doi.org/10.36283/PJMD12-3/007
How to cite: Saeed I, Sadiq M, Fazal F, Ali AS, Shahid F, Zafar M, Azam NM, Ain QU, Nazir M, Noor A. Ahmed NU. Effect of a Health Education Intervention on Practices of Hospital Laboratory Staff; A Quasi-Experimental Study. Pak J Med Dent. 2023;12(3): 36-41. doi: 10.36283/PJMD12-3/007
Background: The incidence of Laboratory acquired infections is on the rise despite the existence and continuous upgradation of infection prevention protocols. The objective of this study was to determine the practice of lab staff before and after carrying out an intervention in the form of health education intervention based on WHO protocols for infection prevention.
Methods: This is a Quasi-experimental study carried out in three hospitals in Rawalpindi. A total of n=38 technical and non-technical lab staff participated in the study. Laboratory practices were observed by the researchers themselves for a week. Then an education session was conducted for the staff regarding the World Health Organization (WHO) standard protocols for infection control. The post-intervention data were collected after about two weeks of health education sessions. Data were analyzed using SPSS version 22. Paired t-test was applied to compare the mean scores of pre- and post-interventional data.
Results: The laboratory staff participated in the study mostly 19(50%) belonging to the age(years) range of 20-27. The percentage of respondents having good practice of infection prevention protocols before intervention was 7.5%, after the intervention this increased to 57.9%. Paired t-test showed that the difference in practice mean score of pre- and post-interventional data was statistically significant (CI=21.55-15.33 p-value=0.001).
Conclusion: Pre-intervention data showed that the practice of the staff was not completely in accordance with WHO infection prevention. After delivering the education session on WHO infection prevention protocols, there was a significant improvement in the practices of laboratory staff.
Keywords: Laboratory Infections, Biosafety, Prevention, and Control
Laboratory technical staff have to handle various samples and specimens and any kind of negligence could result in the transmission of infection caused by these pathogenic organisms1. As laboratory staff faced frequent exposure to infectious agents, the risk for occupational hazards increases. The transmission of laboratory infections can occur through a number of different routes. Some of these include: inhalation of contagious aerosols, contact with mucous membranes, or infection via the percutaneous route such as through cuts, accidental self-inoculation, etc2.
In developing countries like Pakistan where resources are already minimal the number of laboratory infections is alarmingly higher3. Standard precautions (devised in 1996 and revised in 2007 by the CDC, with recent changes in light of the COVID pandemic) make up the basic protocols that hamper the spread of infectious diseases4. Standard precautions such as hand hygiene, use of gloves, gowns, eye protection, use of cough etiquette, and safe disposal of sharp instruments can significantly reduce the incidence of LAIs. Specific infections can be prevented by measures such as prophylaxis after exposure and immunization of laboratory employees5. Compliance with the standard precautions is highly necessary to avoid these infections which is unfortunately low among healthcare workers6. A survey carried out in 2017 in Karachi proved that the carelessness of many laboratory technicians can lead to the spread of diseases. The statistics were astonishing because 65% of laboratorians did not use PPE. Only 65% properly followed the procedure regarding the disposal of syringes and even though the use of mouth pipetting is now considered obsolete, 45% continued to do so7.
Even the improper use of PPE poses a serious threat. The technician could contaminate the skin or their clothes during removal, thus acting as a potential transmitter of the contagious organism to co-workers, fomites, and even patients8. Thus, lack of knowledge among healthcare workers accounted for the non-compliance and carelessness leading to the spread of infections creating biohazard9. Multiple research has shown that interventional sessions can be quite pivotal in helping spread awareness regarding the harms of laboratory infections10. Discarding hospital waste requires a proper hospital waste management plan. Not just that, it is necessary to abide by the procedures of waste disposal to ensure the complete prevention of environmental and occupational risks11. A remarkable decrease in laboratory infections could be noted if all proper preventive strategies were put into place. These mainly included hand hygiene, the use of personal protective equipment, and the correct disposal of hospital waste12. Studies had suggested that adequate educational sessions, training sessions, and refresher courses significantly improved the practices of HCWs toward infection prevention and control13,14.
Some of the primary determinants of poor implementation of healthcare protocols in the laboratory included, according to WHO, poor knowledge and attitude regarding the spread of infections through staff members15. The reasons include limited infrastructure and resources along with poor management and organization; all of these factors manifest in a lack of professional competency 16. The aim of this study was to determine the practice of lab staff before and after carrying out an intervention in the form of health education intervention based on WHO protocols for infection prevention.
This study was carried out on the laboratory staff working in three different hospitals in Rawalpindi. The Study Duration was from May to November 2022. The study got its ethical approval from the institutional review board of Rawalpindi medical university (Reference number: PSY-73-46-22). The Study Design was Quasi-Experimental. The sample size came out to be 38 calculated by WHO Sample Size Calculator. Lab staff working in three Allied hospitals of Rawalpindi were included in the study. Trainees and student-lab technicians and those who had attended recent refresher training were excluded from the study.
A questionnaire was designed after reviewing different scientific literature using a combination of dichotomous and Likert response scales. The questionnaire was divided into three sections which include informed consent, demographic data, and lastly assessment of practices of the lab technical staff regarding infection control procedures. The overall level of practice was classified as poor (< 20 points, <70% score), moderate (21-25 points, 70–85% right answer), and good (26-30 points, 86–100% score) Intervention was done in the form of Health Awareness Session in accordance with WHO standard protocols for infection prevention by infection control officer for the lab staff in Hospitals. Data were retrieved in Excel and analyzed using SPSS version 22. Frequency, percentage, mean, pie charts, and tables for representation of data were used. Paired t-test was used for the comparison of pre-and post-intervention data, and a p-value of <0.05 was taken as statistically significant.
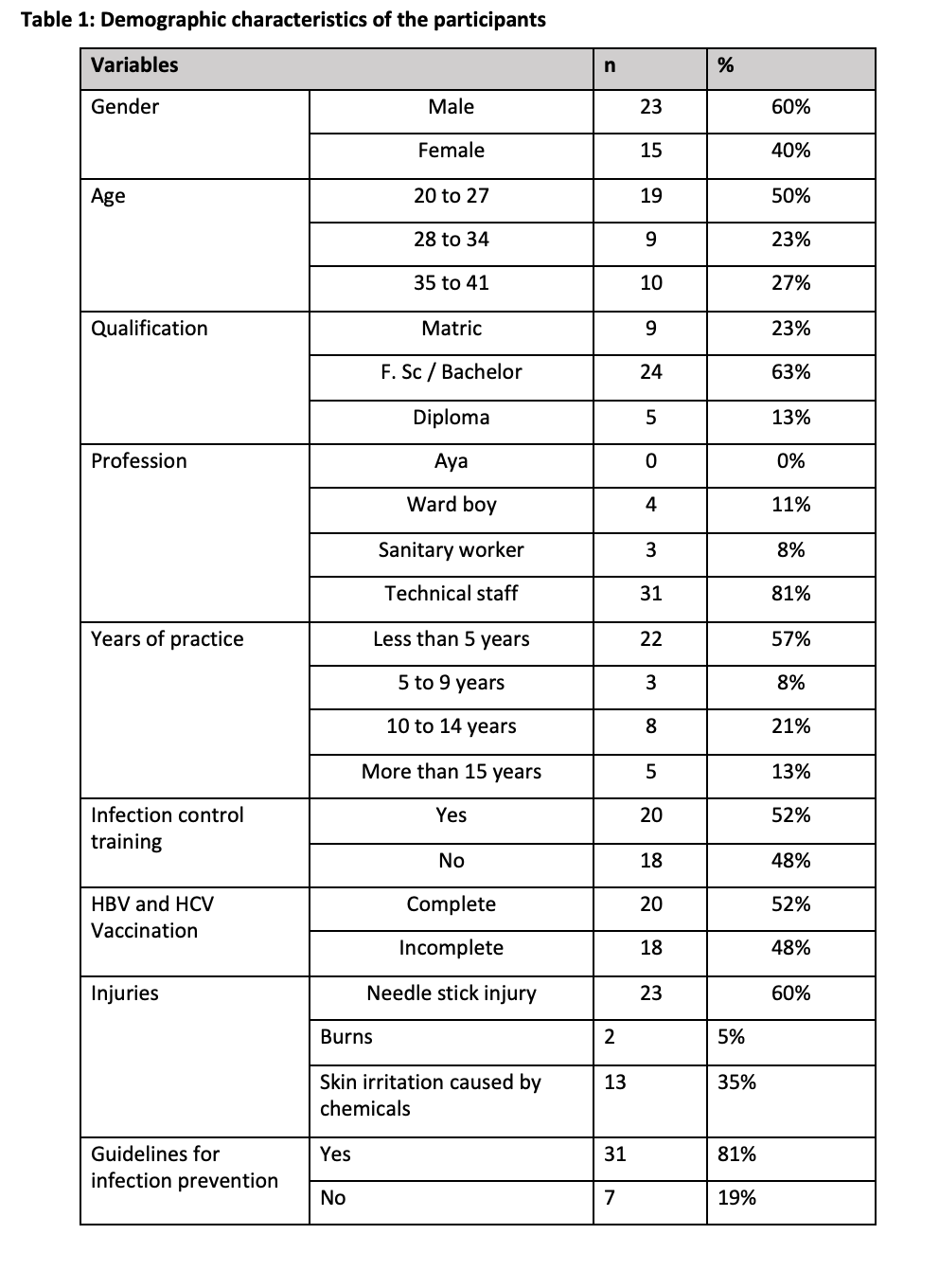
A total of 38 technical and non-technical lab staff participated in the study. The majority of them were technical staff, mostly 19 (50%) belonging to the age group 20 to 27. Most of them were males. The demographic details are given in the following Table 1:
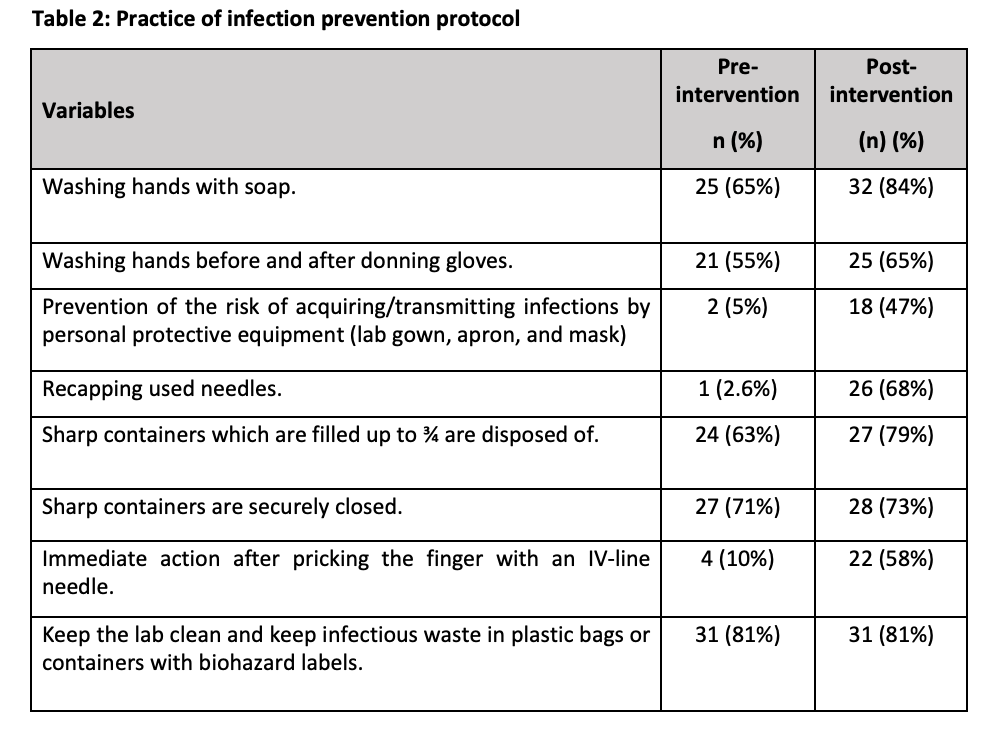
65% of the participants knew that hands must be washed with soap before lab work. This percentage increased to 84% after our intervention. Only 10% knew that immediate action after pricking the finger with an IV-line needle should be taken. This percentage increased to 58% after our intervention. Table 2 shows the different aspects of lab practices observed before and after carrying out the intervention.
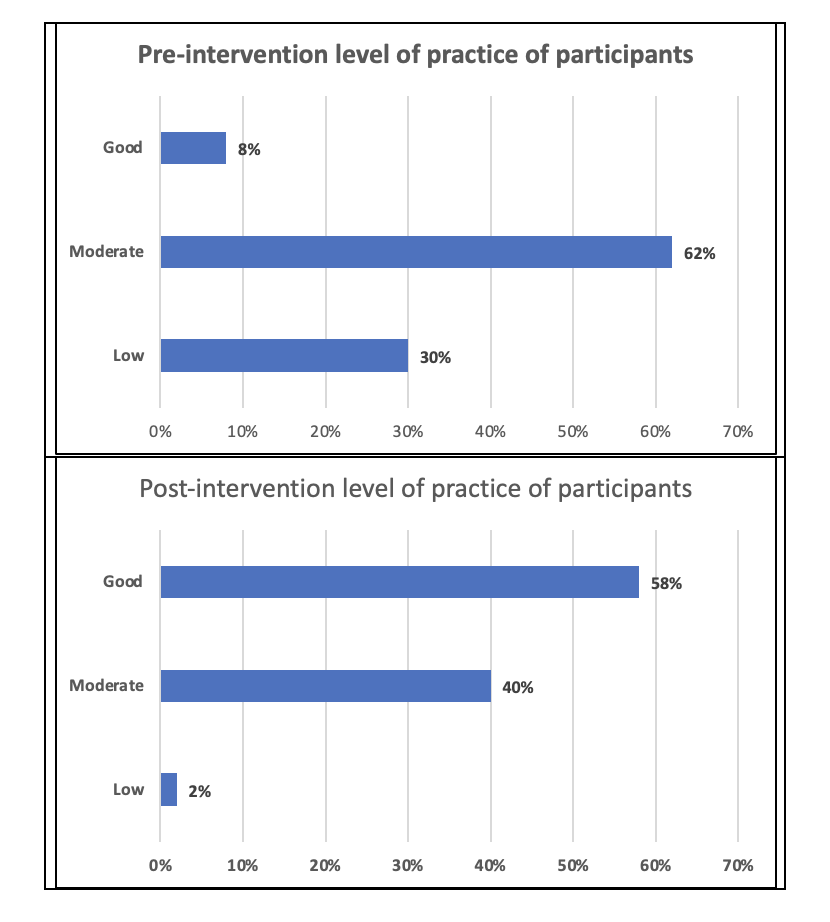
Only 8% of the lab staff had a good level of practice in accordance with infection prevention protocols before the intervention and 62% had a moderate level. On the contrary, 58% of the lab staff had a good level of practice in accordance with infection prevention protocols after the intervention (Figure 1).
Paired t-test showed that the difference in practice mean score of pre- and post-interventional data was 18±10.58(C. I=21.55-15.33) with a p-value of 0.001.
The significant p-value of 0.001 shows that the null hypothesis has been rejected and that the practice score of the population prior to intervention and after it is not the same. Hence our intervention has been proved fruitful and the mean practice scores of the infection prevention protocols improved after the intervention.
Hospital-acquired infections pose a threat to a million patients worldwide and are also a potential risk factor for healthcare workers as well. It is the responsibility of healthcare providers and managers to rude the risk of the spread of these hazardous infections as much as possible. When asked if participants had ever attended any training program on infection prevention, 58 % had previously attended one or two training programs on infection prevention, about one-two years ago. This number points to the fact that still, 42 % of our study population had never attended even a single workshop or program on infection prevention which is alarming. A study carried out in Nigeria showed that 67.2% of healthcare workers had previously had any form of infection prevention training17. In our study, we further wanted to assess the incidence of any injury that the lab staff would have faced during their work in hospital labs. 60 % of our study population had got needle stick injuries at least once during their work in the hospital lab. A study in Malaysia showed that the prevalence of needle stick injury in its medical laboratory technicians was 28.7%18. Yet another study conducted in Qatar, pointed out that of the total (1022) studied subjects, 214 studied subjects (20.9%) were victims of needle stick injuries4. 81% of our study population said that there is a proper display of infection prevention guidelines in their working department. It means that hospital administration is playing its part to educate the lab staff on infection prevention guidelines.
Another worth mentioning thing that we wanted to observe in our study was the level of practice of infection prevention protocols among our hospital lab staff. Only 7.5% of our study population had a good level of practice with the infection prevention protocols prior to our intervention. And after our intervention, we observed that 57% of participants showed to have a good level of practice of infection prevention protocols. Another study in Ghana showed that compliance of health care workers including the lab technicians with Infection Prevention and Control guidelines was 30.7%19. This points to the fact that interventions such as awareness and educational sessions and workshops for hospital lab staff can improve the level of their practice of infection prevention protocols. We also observed that certain practices of infection prevention protocols were especially neglected by the hospital lab staff before our intervention. Before our intervention only 1 participant out of 38 admitted that he does not recap the needles after use. All other 37 participants said that they had practice of recapping the needles after their use. This depicts the fact that knowledge and awareness of the practice of infection prevention protocols are much needed. Because recapping needles after their use can lead to re-usage of those needles by anyone who gets hold of them. But after our intervention, participants said that they then were doing the practice not recapping the needles after their use. This again shows the importance of interventions to increase the practice of infection prevention protocols17.
Furthermore, before our intervention only 2 participants of our study out of 38 said that they used personal protective equipment (lab gown, apron, mask) to prevent the risk of acquiring/transmitting infections. This shows that the use of PPE is not taken seriously by the hospital lab staff. Now this could be due to a lack of awareness or lack of motivation to use PPE during lab work. But after our intervention, we observed that 18 participants said that they then used PPE during their lab work. Thus, educating the lab staff regarding the proper use of PPE and its potential benefit can help in increasing the number of lab staff that adhere to the infection prevention protocols. In a study on the Effects of Infection Control Education for Nursing Students, it was concluded that significant increases in knowledge, awareness of standard precautions, and infection control performance were observed after the intervention 4. The guidelines and protocols for infection prevention are already available, it is now the need of the hour that these guidelines and protocols be followed by everyone dealing with infections and infectious waste and samples. This result that we have observed in our study stresses the need to introduce programs and workshops on infection prevention for lab staff working in various hospitals. Moreover, lab staff should be encouraged to attend these workshops on infection prevention. This will not only improve the performance of lab staff but will also ensure that no diseases are spread through the hospital staff itself.
The practice of the lab staff regarding the infection prevention protocol was at par there was a need for a proper education session. After delivering the education session, there was a significant improvement in practices. Therefore, the regular educational sessions and refresher courses will help control laboratory-acquired infections.
I would like to acknowledge the hospital staff for their immense contribution.
No conflict of interest exists.
The study got its ethical approval from the institutional review board of Rawalpindi medical university (Reference number: PSY-73-46-22).
Informed consent was taken from all participants.
All authors equally contributed to this research study.
- Coelho, A. C., & Díez, J. G. (2015). Biological risks and laboratory-acquired infections: a reality that cannot be ignored in health biotechnology. Frontiers in Bioengineering and Biotechnology. doi: 10.3389/fbioe.2015.000562
- Peng, H., Bilal, M., & Iqbal, H. M. N. (2018). Improved Biosafety and Biosecurity Measures and/or Strategies to Tackle Laboratory-Acquired Infections and Related Risks. International journal of environmental research and public health. https://doi.org/10.3390/ijerph15122697
- Abalkhail A, Al Imam MH, Elmosaad YM, Jaber MF, Hosis KA, Alhumaydhi FA, Alslamah T, Alamer A, Mahmud I. Knowledge, Attitude and Practice of Standard Infection Control Precautions among Health-Care Workers in a University Hospital in Qassim, Saudi Arabia: A Cross-Sectional Survey. International Journal of Environmental Research and Public Health. 2021 Nov 11;18(22):11831. DOI: 3390/ijerph182211831
- .Kim E, Kim SS, Kim S. Effects of Infection Control Education for Nursing Students Using Standardized Patients vs. Peer Role-Play. Int J Environ Res Public Health. 2020;18(1):107. Published 2020 Dec 26. doi:10.3390/ijerph18010107
- Alhumaid, S., Al Mutair, A., Al Alawi, Z. et al. Knowledge of infection prevention and control among healthcare workers and factors influencing compliance: a systematic review. Antimicrob Resist Infect Control 10, 86 (2021). https://doi.org/10.1186/s13756-021-00957-0
- Tvedt C, Bukholm G. Healthcare workers’ self-reported effect of an interventional programme on knowledge and behaviour related to infection control. Quality and Safety in Health Care. 2010 Dec 1;19(6):e7-. DOI: 1136/qshc.2007.026252
- Ahmed, S. (2019, March). A Survey on Biosafety Practices in Lab Personnel in 12 Selected Areas of Karachi, Pakistan. Journal of Biosafety and Biosecurity, Volume 1(Issue 1), Pages 68-72. https://doi.org/10.1016/j.jobb.2018.12.001
- Casanova L, Alfano-Sobsey E, Rutala WA, Weber DJ, Sobsey M. Virus Transfer from Personal Protective Equipment to Healthcare Employees’ Skin and Clothing. Emerg Infect Dis. 2008;14(8):1291-1293. https://doi.org/10.3201/eid1408.080085
- Sax H, Perneger T, Hugonnet S, Herrault P, Chraïti MN, Pittet D. Knowledge of standard and isolation precautions in a large teaching hospital. Infection Control & Hospital Epidemiology. 2005 Mar;26(3):298-304. DOI: 1086/502543
- World Health Organization, India. Medical Waste. (2018). Available online at: http://www.searo.who.int/india/topics/medical_waste/en/ (accessed December 19, 2018)
- Kwikiriza S, Stewart AG, Mutahunga B, Dobson AE and Wilkinson E (2019) A Whole Systems Approach to Hospital Waste Management in Rural Uganda. Front. Public Health 7:136. doi: 10.3389/fpubh.2019.00136
- Khan N, Azam N, Mahmood H, Iftikhar A, Afzal A.Impact of Intensive Training Programme on the Knowledge and Practice of Infection Control Among Auxiliary Staff in A Tertiary Care Hospital. Pak Armed Forces Med J 2022; 72(1): 54-57.Doi: https://doi.org/10.51253/pafmj.v72i1.5637
- Hassan ZM. Improving knowledge and compliance with infection control standard precautions among undergraduate nursing students in Jordan. American journal of infection control. 2018 Mar 1;46(3):297-302. doi: 1016/j.ajic.2017.09.010
- Uchendu OC, Desmenu AP, Owoaje ET. Effect of training on knowledge and attitude to standard precaution among workers exposed to body fluids in a tertiary institution in south-west Nigeria. Annals of Ibadan Postgraduate Medicine. 2020;18(2):100-105
- Geberemariyam, B.S., Donka, G.M. & Wordofa, B. Assessment of knowledge and practices of healthcare workers towards infection prevention and associated factors in healthcare facilities of West Arsi District, Southeast Ethiopia: a facility-based cross-sectional study. Arch Public Health 76, 69 (2018). https://doi.org/10.1186/s13690-018-0314-0
- Khan, T., Tanveer, F., & Muhammad, J. (2021). Improving Biosecurity in Pakistan: Current Efforts, Challenges, and Recommendations on a Multidimensional Management Strategy. Health security, 19(3), 254–261. https://doi.org/10.1089/hs.2020.0050
- Enwere OO, Diwe KC. Knowledge, perception and practice of injection safety and healthcare waste management among teaching hospital staff in south east Nigeria: an intervention study. Pan African Medical Journal. 2014;17(1) DOI: 11604/pamj.2014.17.218.3084
- Rampal L, Zakaria R, Sook LW, Zain AM. Needle stick and sharps injuries and factors associated among health care workers in a Malaysian hospital. Eur J Soc Sci. 2010 Mar;13(3):354-362. doi: 18295/squmj.2020.20.01.008
- Kondor VD. Health Worker Compliance with Infection Prevention and Control Policy in Ghana: A Case Study of La General Hospital. UG Space. 2018:1-37.
DOI: 10.21522/TIJPH.2013.09.02.Art014
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
