By Hamza Ashraf, Sherjeel Saulat, Syed Saeed Uddin Qadri, Duramin, Awais Ayub, Nauman Sadiq Kiani, Mansoor Ejaz
AFFLIATIONS:
Tabba Kidney Institute, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-2/007
How to cite: Ashraf H, Saulat S, Qadri SSU, Duramin, Ayub A, Kiani NS, et al. All That Glitter is not Gold: Computed Tomography-Kidney Ureter Bladder (CT-KUB) is not necessary for a Safe Percutaneous Nephrolithotomy. Pak J Med Dent. 2022;11(2): 36-43. doi: 10.36283/PJMD11-2/007
Background: Diagnosis of renal stones is tricky and appropriate diagnosis requires exact location and size identification of renal stones along with the degree of obstruction and hydronephrosis. This study aimed to compare the difference between Ultrasound and Computed tomography Kidney ureter Bladder (CT KUB) groups for stone clearance, diagnostic accuracy, laboratory parameters, and complications.
Methods: This is a cross-sectional, comparative effectiveness trial; patients (n=100) with suspected renal stones were randomly assigned with a 1:1 ratio in two different imaging groups, Group A (n=50) participants had ultrasonography and group B (n=50) patients had Computed tomography as a diagnostic imaging modality. The complications and operative differences were compared with the help of student t-test and chi-square tests, a p-value of 0.05 was considered statistically significant.
Results: The mean age of the patients was 37.3 ± 17 years and 45.8 ± 14.7 years in group A and group B, respectively. The study found no difference (0.3 and 0.1) between pre-operative stone size measurements of the renal unit by ultrasound and CT [(2.4±0.9 cm and 2.7±1.8cm (right) 1.8±1.0 cm and 1.9±0.7 cm (left)]. The sensitivity and specificity of USG for renal stone diagnosis was 84.8%, while CT indicated 86% accuracy, X-Ray KUB was used for radiopaque stones only and showed 78.6% sensitivity and specificity.
Conclusion: The pre-operative stone sizes indicated in ultrasonography and CT were similar in intra-operative, retrograde pyelogram (RPG) measurements, referred to the accuracy of stone size prediction. Simple x-ray and ultrasonography are cost-effective, easily available in hospitals, with minimal radiation exposure.
Keywords: Percutaneous Nephrolithotomy; Ultrasonography; Kidney Stones.
Renal stones are one of the most attributed medical problems in underdeveloped countries with higher incident rates, geographically, Pakistan is placed on a stone belt increasing the chances of its population of getting renal stones, enhancing the chances of obstructive uropathy, and in extreme cases loss of renal function1. Treatment of renal stones has been evaluated enormously in the last decades, upgrading of minimally invasive procedures to remove stones got the most deserving hype. Percutaneous nephrolithotomy (PCNL) is known as the gold standard to remove renal stones with minimal invasion2. Usual indications of PCNL are stone sizes (> 1.5 cms), stone location (lower calyceal stones), number of stones (Staghorn stones, multiple stones and hard stones) where Extracorporeal shock wave lithotripsy (extracorporeal shockwave lithotripsy (ESWL), retrograde intrarenal surgery RIRS), Ureteroscopy (URS) flop to attain stone clearance. PCNL has decreased the risk factors associated with open surgeries, including excessive financial burden and longer hospital stay3.
Diagnosis of renal stones is tricky and needs expensive imaging technologies to identify the size, location, and site of stones. The appropriate diagnosis requires exact location and size identification of renal stone along with the degree of obstruction and hydronephrosis, Urologists recommend Computed tomography KUB and/or Ultrasonography KUB to evaluate associated factors of renal stone and endorse surgery. Ultrasonography is known as the first imaging modality of choice for patients presenting with flank pain and clinical identification of renal stones for being economical, easily available and time-saving. The efficacy of ultrasonography for the diagnosis of renal stones relies upon secondary findings of renal stones such as hydronephrosis. Ultrasonography can distinguish dilatation of pelvicalyceal system, hydronephrosis, and location of stone giving health care providers a complete glimpse of renal stone characteristics4. Sampaio et al. has categorized the collecting system of the renal area within four different forms, the classification was based upon the difference of opening of major calyces. This classification had AI, AII, BI and BII categories5.
Collecting system combined with upper and lower calyx was categorized in AI, when upper, lower or both calyxes open in middle calyx it is categorized in AII, when the mid pole opens to the renal pelvis categorized as BI, and when small calyces of mid pole enter the renal pelvis categorized as BII. Another inexpensive and time-saving technique is X-Ray KUB with a sensitivity of 40-50% only. Non-contrast CT KUB and intravenous pyelogram are comparatively expensive and time-consuming modalities for renal stone diagnosis. Although, the sensitivity is very high, and diagnostic accuracy is 100% with this imaging technique6. Renal stones have a high recurrence ratio, patients may need multiple scans, therefore making them more prone to the risks associated with excessive radiation dosage7. In countries like Pakistan, India, Nepal, and Bangladesh, where geographical factors contribute to the prevalence and recurrence of renal stones, the economic burden of diagnostic modalities and stone removal procedures is unaffordable for more than 60% of the population7-9. American Urological Association (AUA) has indicated to avoid multiple CT scans and excessive radiation exposure, however, the usage of CT KUB is still in priority6,10,11.
A landmark randomized multi-center research was conducted in four different geographically located emergency departments, to assess the efficacy of ultrasound versus CT tomography for early diagnosis of renal stones, indicating that ultrasonography is quick, economical, and easy to perform the procedure with 85% accuracy of results. While CT has 99% accuracy for renal stone size and location, at the same, the CT is comparatively slower, expensive, and less available and has increased radiation exposure12. Therefore, this study aimed to evaluate the efficacy of ultrasonography for the diagnosis of renal stones for PCNL and to compare the difference between Ultrasound and CT KUB groups for stone clearance, Diagnostic accuracy, laboratory parameters, and complications.
This was a cross-sectional, comparative effectiveness trial, study participants (n=100) were recruited from the urology department, Tabba Kidney Institute Karachi. Patients were enrolled from November 2020 until June 2021, after identification of presenting symptoms and relevant history, age range 18-60 years, reported in the Emergency department or outpatient department with a complaint of flank pain or with other lower urinary tract symptoms, and attending urologist decided to get the radiological image for renal stone diagnosis. The patients with suspected renal stones were randomly assigned with a 1:1 ratio in two different imaging groups, Group A participants had ultrasonography and group B patients had Computed tomography as a diagnostic imaging modality. Randomization was performed via computerized randomization software; every patient was allotted a unique ID number. The ethics approval of the study was obtained from the institutional ethical review committee (ERC Approval number: TKI-HEC-012).
Patients with impaired renal function, solitary kidney, and radiolucent stones were excluded from the study along with pregnant patients and previously reported for the stones under question, on the diagnosis of sepsis and End-stage renal disease. After identification, an informed consent form in the language of understanding was explained to patients by attending health care providers; patients were asked to sign the consent form to enroll them in the research.
The radiologist performed the imaging including ultrasound KUB and X-ray KUB for group A and CT pyelogram for group B participants. For group A the diagnostic criteria were stone should be visible in at least one of the modalities between ultrasound and X-ray. Ultrasound reports were prepared after 1 hour while CT pyelogram reports were available after 6 hours. Pre-operative laboratory investigations were ordered including hemoglobin, hematocrit, platelets, total leucocytes, serum creatinine, and urea. Urine culture was ordered to rule out urinary tract infections, every patient was asked to consult an anesthesiologist to get approval for general anesthesia. After identification of stone, patients were aligned for percutaneous nephrolithotomy to remove the stone, after considering all aspects RPG (retrograde pyelogram) was performed to measure the size of the stone and compare the accuracy of stone size, location, and numbers from pre-operative diagnostic imaging modality results. The main endpoints of this study were to identify the efficacy of Ultrasound and CT scans for renal stone diagnosis, renal stone size accuracy, and associated symptoms such as hydronephrosis and hydroureter.
Data was entered and analyzed in a statistical package of social science version 22. Descriptive variables were analyzed as means and standard deviations. Results from complications and operative differences were compared with the help of student t-test and chi-square tests (for gender, age distribution, adverse events, hospital stay, etc.); a p-value of 0.05 was considered statistically significant.
Total 100 cases were enrolled in the study, 50 participants in both groups (Group A -ultrasonography and X-ray KUB and group B- CT KUB). Mean age was measured as 37.3 ± 17 years and 45.8 ± 14.7 years in group A and group B respectively, the significance of the age difference was insignificant with a p-value of 0.08. Gender distribution of both groups indicted 33 (66%) males and 17 (34%) females in group A, while 25 (50%) males and 25 (50%) females were recruited in group B. Marital status was interpreted as 36 (72%) and 44 (88%) married participants in group A and group B respectively (Table 1).
Table 1: Demographic details of participants from group A [(ultrasonography and X-ray kidney, ureter, and bladder (KUB)] and group B [(CT kidney, ureter, and bladder (KUB)].
| Variables | Group A
(n=50) |
Group B
(n=50) |
p-Value | |
| Age (Mean ± SD) | 37.3 ± 17.0 years | 45.8 ± 14.7 years | 0.08 | |
| Weight (Mean ± SD) | 60.3 ± 23 kg | 71.1 ± 17.4 kg | 0.03 | |
| Gender | Male | 33 (66%) | 25 (50%) | 0.07 |
| Female | 17(34%) | 25(50%) | ||
| Marital status | Married | 36(72%) | 44(88%) | 0.03 |
| Unmarried | 14(28%) | 6(12%) | ||
The comparison of stone characteristics of participants within both groups A and B showed that both groups had almost similar stone sizes with a mean value of 2.4 ± 0.9 cm and 2.7 ± 1.8 cm on the right renal unit of group A and group B respectively. Similarly, the left renal unit’s stone sizes were measured as 1.8 ± 1.0 cm and 1.9± 0.7 cm in group A and Group B. The p-value of both renal units was 0.3 and 0.1 respectively. Single stones were present in 42 and 29 participants of group A and Group B respectively, Multiple stones were defined as more than 2 stones present in the same location were identified in 8 and 21 participants within groups A and B respectively with a p-value of 0.51.
Location of stone was differentiated within pelvis area, upper, mid, lower calyx, and multiple calyces, results indicated 20, 4, 10, 11, and 5 participants of group A within previously mentioned locations respectively. In group B, 22 patients had pelvic stone, 3 had upper calyx, 12 had mid calyx, a lower calyx, and 4 had multiple calyx stones, p-value of stone location between group A and B was 0.42. A maximum number of participants had left side stones with 26 and 28 in group A and group B respectively. Bilateral stones were present in 6 and 5 participants of groups A and B respectively, with an insignificant p-value of 0.15 (Figure 1).
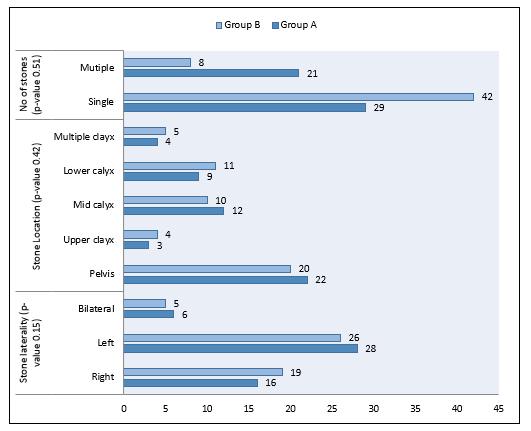
Figure 1: Stone characteristics of study cases: Group A and Group B.
Comparison of pre-operative and post-operative laboratory investigations was documented, results indicating that both group participants had similar laboratory investigation results. However, hemoglobin decline was slightly high postoperatively in group B as compared to group A. Intra-operative details including the need for pre-op stenting to support renal system, pre-op transfusion to treat anemia were documented in both groups, stenting was needed in 14(7%) participants of group A while 3(1.5%) participants of group B needed stenting. Although the need of transfusion post-operatively was required in only 1 (0.5%) patient of group A 2(1%) patients needed Transfusion in group B. Upon analyzing the difference between a finding of RGU of both groups, we found staghorn calculi in 4(2%) and 2(1%) patients in group A and B respectively, any stone present in more than two calyces and measuring more than 2.5cms was defined as Staghorn calculi. Most found stones were in the pelvis, 13(6.5%) and 17 (8.5%) of participants from groups A and B were identified with pelvic stones on RGU. The second most commonly occurring stone location is lower calyx with 7(3.5%) and 3(1.5%) of a participant in groups A and B respectively.
Sampaio classification was identified as A1, A2, B1, and B2 in 15(7.5%), 6(3%), 9(4.5%), and 7(3.5%) participants of group A while 20(10%), 2(1%) and 8(4%) in group B. Group B participants do not indicate B2 class of Sampaio. Stone seizes were categorized within 4 groups intra-operatively within > 10mm, >20mm, >30mm and >40mm of sizes, 18(9%), 17(8.5%), 10(5%) and 5(2.5%) patients were identifying in these categories from group A respectively, similarly group B participants showed 15(7.5%), 25 (12.5%), 1(0.5%) and 9(4.5%) of categorization according to stone sizes. After percutaneous nephrolithotomy, clearance was noted in 45(22.5%) and 44(22%) of participants from group A and group B respectively, there was no significant difference between clearance rates of both groups (p-value 0.3).
Post-operative, iatrogenic complications were documented as pelvic tear, presented in 1(0.5%) patient of group A, a mucosal tear in 7(3.5%) and 2(1%) of patients of group A and B within categories. While under dilatation was reported in only 1 (0.5%) patient of group B. Operative time was measured as total operative time and lithotripsy activation time, results were 99.9 ± 37.6 mins and 31.4 ± 26.9 mins respectively in group A, while group B indicated 96.7 ± 43.5 mins and 36.0 ± 29.2 mins with the insignificant p-value. Hemoglobin drop was measured as 1.0 ± 1.0 and 0.9 ± 0.9 in group A and group B with the slightly elevated drop-in group A. Sensitivity and specificity of USG for renal stone diagnosis was 84.8%, while CT indicated 86% accuracy, X-Ray KUB was used for radiopaque stones only and showed 78.6% sensitivity and specificity of results (Table 2).
Table 2: Intraoperative details of the study participants.
| Variables | Group A Frequency
(n) (%) |
Group B Frequency
(n) (%) |
p-Value | |
| Pre stenting | Yes | 14(7%) | 3(1.5) | 0.004 |
| Pre-OP Tx | Yes | 1(0.5%) | 2(1%) | 0.4 |
| Finding on RGU | Staghorn | 4(2%) | 2(1%) | 0.2 |
| Pelvis stone | 13(6.5%) | 17(8.5%) | ||
| Upper calyx | 2(1%) | 0 | ||
| Mid calyx | 3(1.5%) | 1(0.5%) | ||
| Lower calyx | 7(3.5%) | 3(1.5%) | ||
| Sampaio Classification | A1 | 15(7.5%) | 20(10%) | 0.02 |
| A2 | 6(3%) | 2(1%) | ||
| B1 | 9(4.5%) | 8(4%) | ||
| B2 | 7(3.5%) | 0 | ||
| No of stones | Single | 22(11%) | 28(14%) | 0.46 |
| Multiple | 20(10%) | 30(15%) | ||
| Stone size | > 10mm | 18(9%) | 15(7.5%) | 0.02 |
| >20mm | 17(8.5%) | 25(12.5%) | ||
| >30mm | 10(5%) | 1(0.5%) | ||
| >40mm | 5(2.5%) | 9(4.5%) | ||
| Clearance | Complete | 45(22.5%) | 44(22%) | 0.3 |
| Partial | 5(2.5%) | 6(3%) | ||
| Iatrogenic complications | Pelvic Tear | 1(0.5%) | 0 | 0.2 |
| Mucosal tear | 7(3.5%) | 2(1%) | ||
| Under dilatation | 0 | 1(0.5%) | ||
| Operative time | 99.9 ± 37.6 | 96.7 ± 43.5 | 0.17 | |
| Lithotripsy activation time | 31.4 ± 26.9 | 36.0 ± 29.2 | 0.1 | |
| Hemoglobin drop | 1.0 ± 1.0 | 0.9 ± 0.9 | 0.13 | |
The endpoint of the study was to evaluate the difference between pre-operative stone size measurement with ultrasound, X-ray, and CT KUB with intra-operative stone measurements, results indicated no difference between pre-operative stone size measurements of ultrasound and CT. Although, CT with higher accuracy rates and radiation dosage had increased accurate results ultrasound showed similar results with a comparatively lower financial burden (Figure 2).
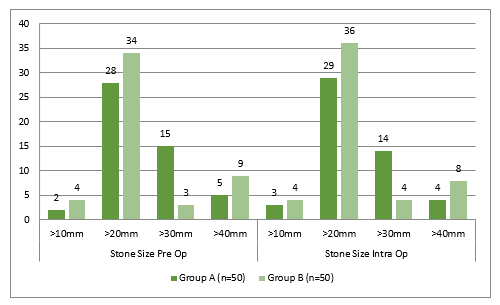
Figure 2: Difference of stone size within the pre-operative radiological measurement and intra-operative measurements.
This study showed equivalent results of stone clearance in ultrasonography and CT groups, the results are like the studies, which identified comparative results between both imaging modalities, contemplating the fact that urolithiasis tends to reoccur frequently at any age and need have repeated imaging tests may be necessary for patients13,14. Urologists avoid unnecessary radiation exposure to patients and work on low cost, easy to perform diagnostic tests. Ultrasonography has been known to be a good option to evaluate the renal stone diagnosis in adults and the pediatric population15.
Another remarkable identification of this research was a comparison of pre-operative stone sizes with ultrasonography and CT with intra-operative, RPG (retrograde pyelogram) base measurements of renal stones. These comparison results showed almost equal accuracy between pre-operative and intra-operative stone sizes, these results were like the studies conducted previously16. In this study, ultrasonography patients were exposed to relatively lower radiation as compared to CT group participants with equivalent results of stone clearance and stone size accuracy12. Urolithiasis patients usually present with a complaint of moderate to severe flank pain along with other lower urinary tract symptoms such as dysuria, anuria and in some cases hematuria. Emergency diagnosis of renal stone and deciding the need for emergency intervention is crucial in renal health care institutes6,17. Countries like Pakistan have a higher incidence rate of urolithiasis in adult and pediatric populations with lower economic stability for which the need for low-cost diagnostic tests should be considered when ruling out the diagnosis. To avoid unnecessary financial burden to patients along with improved weight time to get test results back, urologists should opt for an imaging modality fulfilling the above-mentioned criteria, which is ultrasound1,2,18. CT pyelogram has been evaluated for its accuracy in many studies and proved to be the best imaging modality for renal stone diagnosis but elevated radiations, complicated procedure, the prolonged waiting time to get results back and availability of equipment have been some major concerns for health care institutes in past decades19,20.
The study outcomes do not support the idea that patients should undertake only ultrasound imaging, but relatively that ultrasonography should be recommended as the early diagnostic imaging test, with further radiological tests completed at the decision of the urologist. However, in the current study patients in the ultrasonography groups did not undergo CT, and still, there was no upsurge in any sort of grave contrary measures among patients assigned to ultrasonography. However, the approach of preliminary evaluation with ultrasonography and obtaining additional imaging when needed based on the judgment of the attending urologist commanded to reduce radiation exposure. When the precision of imaging was examined according to the first imaging test a patient underwent, CT had greater sensitivity than ultrasonography, a finding that was consistent with prior research9,16. Patient results and diagnostic accuracy were similar in the two groups. Radiation exposure was slightly higher in the CT group. The strengths of this research include its randomized allocation of participants within groups, eliminating the confounding factors as well as biased results, diversity of demographics in patients, and thorough assessment of clinically relevant pre-operative, intra-operative and post-operative outcomes beyond diagnostic accuracy alone. The restraint of this study is that the researchers could not ensure complete double-blind randomization, as the investigator, patients, and doctors of the study knew the randomization.
A strict reference standard of stone diagnosis to calculate diagnostic accuracy, which had the benefit of being unbiased for imaging method, as evidenced by the equal diagnosis of stones across the two groups. The use of CT for the diagnosis of suspected renal stones has been amplified by an influence of 10 times over the past 15 years in the United States, possibly because of its superior sensitivity and because it can be performed at will in most emergency departments in the United States. Although the difference between population measurements within US and Pakistan are overbearing, literature has evidence of advanced imaging technology used to assess patient outcomes beyond diagnostic precision, and the trial, confirms the viability of evaluating different results. It was found that although ultrasonography was not as sensitive as CT for the diagnosis of nephrolithiasis, using ultrasonography as the initial test in patients with suspected urolithiasis might reduce the chances of need for CT in most patients, resulting in reduced radiation contact.
Results of ultrasonography and X-ray plain abdomen (KUB) combined are equal to results of intravenous urography or CT KUB and sufficient to diagnose renal stone disease among patients presenting with renal stone symptoms. Simple x-ray and ultrasonography are cost-effective, easily available in hospitals, and noninvasive procedures that are much better than computed tomography or Intravenous urogram in terms of quick result, cost-effectiveness, and minimal radiation exposure.
The authors would like to acknowledge the Urology team and the Research Department of TKI for their support.
The authors declared no conflict of interest.
The ERC of Tabba Kidney Institute had approved the study with a protocol number (ERC Approval number: TKI-HEC-012).
Informed consent was taken before enrollment.
HA designed the objective collected the data and assisted in the surgery. SS was involved in surgeries and given final approval of the manuscript. SQ obtained the ethical considerations and did the randomization. DA wrote the manuscript, especially the introduction and methodology sections. AA performed the data analysis, interpreted the results while NK wrote the discussion and analyzed the results.
- Memon WA, El Khalid S, Sharif I, Saulat S, Haider, Asadullah, et al. The efficacy of JJ stent on stone free rate after extracorporeal shock wave lithotripsy: a retrospective study. Pak J Med Dent. 2021; 10(2): 22-27. doi: 10.36283/PJMD10-2/005
- Jahanzeb Shaikh SK, Siddiq A, Mithani S, Saulat S, Sharif I. Use of amplatz sheath in percutaneous nephrolithotomy and effect of its various sizes: randomized controlled trial. J Med Dent. 2020; 9(3): 37-41. doi: 10.36283/PJMD9-3/008
- Lu P, Song R, Yu Y, Yang J, Qi K, Tao R, et al. Clinical efficacy of percutaneous nephrolithotomy versus retrograde intrarenal surgery for pediatric kidney urolithiasis: A PRISMA-compliant article. Medicine (Baltimore). 2017; 96(43): 1-7. doi: 10.1097/MD.0000000000008346
- Sheikh R, ul Haq QT, Abdullah U. Diagnostic role of ultrasonography and X-RAY combined versus intravenous urography in evaluation of renal colic. Professional Med J. 2021;28(05):725-730. doi: 10.29309/TPMJ/2021.28.05.5784
- Sampaio FJ, Mandarim-de-Lacerda CA. Anatomic classification of the kidney collecting system for endourologic procedures. J Endourol. 1988;2(3):247-251. doi: 10.1089/end.1988.2.247
- Roberson NP, Dillman JR, O’Hara SM, DeFoor WR, Reddy PP, Giordano RM, et al. Comparison of ultrasound versus computed tomography for the detection of kidney stones in the pediatric population: a clinical effectiveness study. Pediatr Radiol. 2018;48(7):962-972. doi: 10.1007/s00247-018-4099-7
- Rodger F, Roditi G, Aboumarzouk OM. Diagnostic accuracy of low and ultra-low dose CT for identification of urinary tract stones: a systematic review. Urol Int. 2018;100(4):375-385. doi: 10.1159/000488062
- Jessani S, Bux R, Jafar TH. Prevalence, determinants, and management of chronic kidney disease in Karachi, Pakistan-a community based cross-sectional study. BMC Nephrol. 2014;15(1):1-9. doi: 10.1186/1471-2369-15-90
- Cassim R, Van Walraven C, Lavallée LT, McAlpine K, Highmore K, Leonard MP, et al. Systematic radiologic detection of kidney stones in Canadian children: a new era of asymptomatic stones? J Pediatr Urol. 2019;15(5): e1-467.e7. doi: 10.1016/j.jpurol.2019.05.012
- Nery DR, Costa YB, Mussi TC, Baroni RH. Epidemiological and imaging features that can affect the detection of ureterolithiasis on ultrasound. Radiol Bras. 2018;51:287-292. doi: 10.1590/0100-3984.2017.0113
- Leo MM, Langlois BK, Pare JR, Mitchell P, Linden J, Nelson KP, et al. Ultrasound vs. computed tomography for severity of hydronephrosis and its importance in renal colic. West J Emerg Med. 2017; 18(4): 559-568. doi: 10.5811/westjem.2017.04.33119
- Altaf N, Kamran A, Naseem B, Iqbal M, Asif R, Farooq S, et al. Diagnostic accuracy of ultrasonography versus computed tomography for ureteric calculi among the adult patients visiting Mayo Hospital Lahore. J Health Med Sci. 2019;2:68-74. doi: 10.31014/aior.1994.02.01.21
- Liu S, Nie P, Wang H, Guo J, Shang Q, Xu W, et al. Application of digital tomosynthesis in the diagnosis of urolithiasis: Comparison with MDCT. J Endourol. 2020;34(2):145-150. doi: 10.1089/end.2019.0327
- Barrick L, Cohen DM, Schober MS, Schwaderer A. National imaging trends of recurrent pediatric urolithiasis. Pediatr Emerg Care. 2020;36(4):e217-e221. doi: 10.1097/PEC.0000000000001320
- Morrison JC, Kawal T, Van Batavia JP, Srinivasan AK. Use of ultrasound in pediatric renal stone diagnosis and surgery. Curr Urol Rep. 2017;18(3):1-7. doi: 10.1007/s11934-017-0669-8
- Dai JC, Dunmire B, Sternberg KM, Liu Z, Larson T, Thiel J, et al. Retrospective comparison of measured stone size and posterior acoustic shadow width in clinical ultrasound images. World J Urol. 2018;36(5):727-732. doi: 10.1007/s00345-017-2156-8
- Suetterlin KJ, Vivekanandam V, James N, Sud R, Holmes S, Fialho D, et al. Annual renal ultrasound may prevent acute presentation with acetazolamide-associated urolithiasis. Neurol Clin Pract. 2019:1-3 doi:10.1212/CPJ.0000000000000761
- Hussain M. Evolution of Urology Services in Pakistan. J Coll Physicians Surg Pak. 2021;31(6):746-749.
- Salmaslıoğlu A, Bulakçı M, Bakır B, Yılmaz R, Akpınar YE, Tefik T, et al. The usefulness of agent emission imaging-high mechanical index ultrasound mode in the diagnosis of urolithiasis: a prospective preliminary study. Diagn Interv Radiol. 2018; 24(3): 169-174. doi: 10.5152/dir.2018.18005
- De Lima CS, Cintra CA, Meirelles AÉ, Crivellenti SB, Mariani OM, Honsho DK, et al. Sensitivity of urolithiasis detection using urinary, radiography and ultrasound parameters. Semina Agric Sci. 2017;38(6):3599-3604. doi: 10.5433/1679-0359.2017v38n6p3599
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
