By Humera Akhlaq1, Kefi Iqbal2, Nosheen Mahmood3, Mohammad Owais Ismail4, Muhammad Nasir5, Hifza Sheikh5
AFFLIATIONS:
- Department of Oral Pathology, Sindh Institute of Oral Health Sciences, Jinnah Sindh Medical University, Karachi, Pakistan.
- Department of Dental Materials, Sindh Institute of Oral Health Sciences, Jinnah Sindh Medical University, Karachi, Pakistan.
- Department of Pathology, College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Saudi Arabia.
- Department of Pharmacology, Ziauddin University, Karachi, Pakistan.
- Department of Dentistry, Sindh Institute of Oral Health Sciences, Jinnah Sindh Medical University, Karachi, Pakistan.
Background: The recent global crisis afflicted by Coronavirus has led to psychological consequences like anxiety, fear and insecurity among health care workers. Fear of contracting infection and transmitting to close contacts has emerged as a serious concern. Through this study, we aimed to evaluate different psychological sequel experienced by medical and dental students and frontline health workers during COVID-19 pandemic.
Methods: A cross sectional online survey was opted using a link platform targeting frontline health care workers and medical students. Data was collected from September until November 2020. Descriptive statistics was used to address demographic characteristics of participants. Associations among selected qualitative variables were determined using Chi square test. All analysis was done by using SPSS and a p value of <0.05 was considered statistically significant.
Results: A collection of 391 responses was received. There were 266(68%) female and 125(32%) male participants. Vulnerability of family members to COVID-19 was the major concern as reported by 264(67.5%) which was significantly higher among nurses 38(84.4%) and paramedical staff 25(100%) with a p-value <0.001. Around 43(95.6%) nurses and 24 (96%) paramedical staff members were experiencing sleep disturbances p<0.001. Majority 65(90%) physicians had a concern of missing important scientific events. Only 144(36.8%) participants believed vaccination would be effective against COVID-19.
Conclusion: The fear of contracting infection and transmitting to family members has created an overall negative impact on mental health of health care workers. This generates the need to conduct high quality research focusing on addressing measures to promote psychological resilience among health care workers.
Keywords: COVID-19; Anxiety; Mental Health; Pandemics.
In December 2019, there was a cluster of pneumonia cases in the city of Wuhan, China. Investigations performed by the local authorities discovered that a previously unknown virus, named Coronavirus disease 2019, caused it (COVID-19)1. According to Centre for Disease Control and Prevention (CDC) Coronaviruses are groups of microorganisms that are named based upon the presence of crown-liked spikes on its surfaces. This virus can affect both humans and animals. Four different types have been isolated that infect people namely, alpha, beta, gamma and delta2.
On March 11, 2020, World Health Organization declared COVID-19 as pandemic, up until now (August 24, 2021) 213,345,924 confirmed cases and 4,454,131 deaths have been reported worldwide3. Worldwide spread of infectious diseases like COVID-19 has triggered other symptoms like mental illness and psychological distress4. Stress, anxiety, depression, anger, insomnia, frustration, fear of acquiring infection, confusion, irritability, and boredom associated with quarantine are the major psychological sequel of COVID-19 5. In the current pandemic, health care workers (HCWs) are particularly more vulnerable to emotional distress6. A recent study conducted among 1563 HCWs in China found that stress related symptoms are 73.4% while the statistics of depression, anxiety and insomnia are 50.7%, 44.7% and 36.1% respectively7. In the early 2000s, DiGiovanni and collaborators conducted a study in the affected individuals by severe acute respiratory syndrome (SARS) the results showed that emotional distress tempted some of the individuals to violate the orders of being quarantine8. Social isolation and feelings of loneliness in quarantine may accelerate the risk of mental disorders and thus are associated with the high risk of suicide9.
In Pakistan, 1,131,659 confirmed cases of COVID-19 have been reported as of August 23, 2021 and this tally is rising exponentially10. Balkhi and colleagues recently conducted a study among 400 residents of Karachi, which indicated that majority of the residents (88.8%) are afraid of going out of their homes. They further reported that 87% of participants were washing hands and maintaining self-hygiene more frequently than normal (87%) 11. Major research focus is on pathophysiology, diagnosis, clinical presentation and treatment therapies of the disease, whereas psychological aspects of this pandemic is often marginalized, limited data is available on the mental health and psychological sequel among health care workers12,13.
This cross-sectional study addressed the psychological sequel of COVID-19 among front line health care workers and medical students. Objective of the study was to evaluate the consequences of COVID-19 on the mental and behavioral health of front line health care workers and medical and dental students.
An online cross-sectional survey was employed to collect information. Snowball sampling technique was considered for incorporating participants. Sample size of 384 was calculated using Raosoft sample size calculator keeping margin of error at 5% 14. Data was collected using a structured questionnaire developed through the Google forms. Upon providing consent participants were included if they were medical and dental students or health care workers frontline and non-frontline. Forms with incomplete information were excluded from the study. The cross-sectional survey was initiated after approval from Institutional Review Board (IRB) of Jinnah Sindh Medical University, Karachi, Pakistan (JSMU/IRB/2020/346). Data was collected from participants fulfilling the inclusion and exclusion criteria. The link for the questionnaire was shared using emails and social media apps such as WhatsApp, Instagram, and Facebook after briefing the purpose of study and their right to participate or withdraw without any consequences. Each participant was encouraged to forward the link among their social circle to enrol more and more participants. All findings were recorded in the Questionnaire. Questionnaire was reviewed and pretested on students, doctors and nurses in a group of 10 each to ensure clarity of questions. First part of questionnaire comprised of information about demographics of the study participant’s such as age, gender, occupation. Information to evaluate knowledge, attitude and practices related to COVID-19 pandemic were collected in second part of questionnaire. In the third part psychological impact left by COVID-19 including, anxiety and stress were recorded using a set of questions. Data was entered and analyzed by using SPSS version 24 (IBM SPSS Statistics, USA). Descriptive statistics were used to calculate frequency and percentages. Mean scores were calculated for anxiety and depression symptoms. Chi square test was used to calculate association among qualitative variables. p<0.05 was set to be statistically significant.
A total of 391 responses were received. Table 1 shows base line demographic characteristics of study subjects. Mean age of the participants was 24.5 ± 6.15 years with female to male ratio being 2:1. There were 249(63.7%) students and 142(31.9%) front line health care workers including physicians, nurses, and paramedics.
Of 391 participants 31(7.9%) were either currently positive or had recently recovered from COVID-19 infection. In addition, 88(22.5%) gave a history of COVID-19 infection among family members. It was observed that majority of the participants 375(95.9%) were familiar with the signs and symptoms related to the corona virus. Furthermore, 355(90.8%) knew the transmission of the COVID-19 virus can be avoided by simply hand washing or using hand sanitizers. About 362(92%) either were following necessary precautions when interacting with others in terms of transmission of the corona virus via droplet, contact and airborne routes and around 313(80.1%) of the participants were aware of the effects of cleaning environmental surfaces with bleaching solution. One hundred and 65(63.9%) participants were afraid of going out and meeting people. Approximately 362(92%) individuals comprehended the fact that corona virus is more detrimental in individuals belonging to older age group. Imposition of travel bans was considered as an effective move towards curbing the spread of infection by 326(83.3%) where 139(35%) agreed and 187(47.8%) strongly agreed to have cancelled their travel plans in an attempt to decreased spread of virus. When enquired about effectiveness of COVID-19 vaccine 144(36.8%) believed it would be effective whereas 86(22%) assumed it to be in effective and 161(41%) responded as did not know. In sufficient evidence about vaccine, safety was the major concern for not willing to take vaccine.
Table 1: Demographic characteristics of the study participants.
| Variables | Characteristics | n (%) |
| Gender | Male | 125(32%) |
| Female | 266(68%) | |
| Age in years
(Mean±SD) |
24.5±6.1 | 391 |
| Profession | Medical students | 249(62.6%) |
| Doctors | 72(18.4%) | |
| Nurses | 45(11.5%) | |
| Paramedical Staff | 25(6.4%) | |
| Marital Status | Single | 329(84%) |
| Married | 62(15.9%) | |
| Educational status | Undergraduate | 249(63.7%) |
| Graduate | 120(30%) | |
| Postgraduate | 22(5.6%) | |
| Monthly income in PKR | <20,000 | 239(6114%) |
| 20-60,000 | 130(33.2%) | |
| >60,000 | 22(5.6%) |
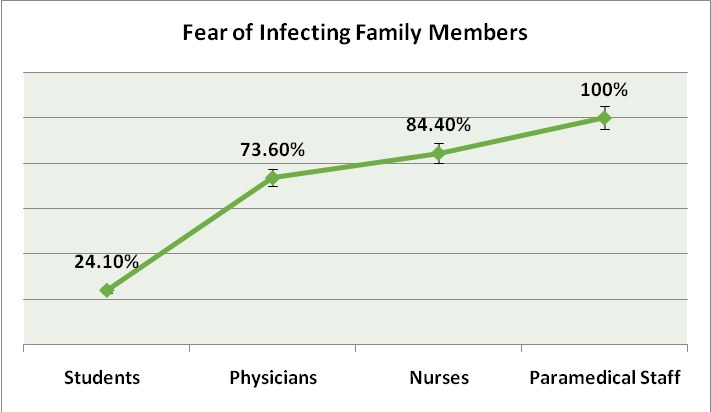
Figure 1: Fear of infecting family members experienced by study participants.
According to 264(67.5%) participants, one major concern was transmitting the disease to family members. It was further observed that frontline health workers had a significantly higher concern of acquiring infection and transmitting to close family members which was more prevalent among nurses p<0.05 as displayed in Figure 1. A significant 253(64.7%) were afraid of acquiring or transmitting infection despite using personal protective equipment (PPE). In order to break the chain of spread 370(94.6%) participants avoided social gatherings. Prevalence of various stressors among different groups of study participants is summarized in Table 2. Nurses and paramedical staff were experiencing significant Insomnia as displayed in Figure 2.
Table 2: Prevalence of various stressors amongst participants.
| Stressors | Students | Physicians | Nurses | Paramedical
Staff |
p-Value |
| Being infected with COVID-19 | 128(51.4%) | 36(50%) | 35(77.8%) | 13(52%) | 0.008* |
| Getting Serious with COVID-19 disease | 36(30%) | 34(28.3%) | 32(26%) |
18(15%) |
<0.001** |
| Nightmares | 20(8%) | 7(9%) | 4(8.9%) | 3(12%) | 0.9 |
| Fatigue | 168(67.5%) | 44(61.1%) | 26(57.8%) |
15 (60%) |
0.488 |
| Frequent need | 237(95%) | 66(91%) | 45(100%) | 18(72%) | <0.001** |
| Frequent use of sanitizers | 235(94%) | 68(94%) | 38(84%) | 16(64%) | <0.001** |
| Attending COVID-19 patients | 168(67.5%) | 40(50.5%) | 26(57.8%) | 14(56%) | 0.35 |
| Going out in crowded places | 168(67.5%) | 44(61.1%) | 26(57.8%) | 15 (60%) | 0.488 |
| Attending social gatherings | 163(65.5%) | 40(50.5%) | 26(57.8%) | 14(56%) | 0.353 |
| Missing important scientific events | 26(10%) | 65(90%) | 6(13%) | 0(0%) | <0.001** |
| Is it safe to be vaccinated? | 20(8%) | 7(9%) | 4(8.9%) | 3(12%) | 0.9 |
| Are you willing to receive vaccine? | 60(24%) | 13(18.1%) | 7(15.6%) |
6(24%) |
0.16 |
*; p<0.05, **; p<0.001
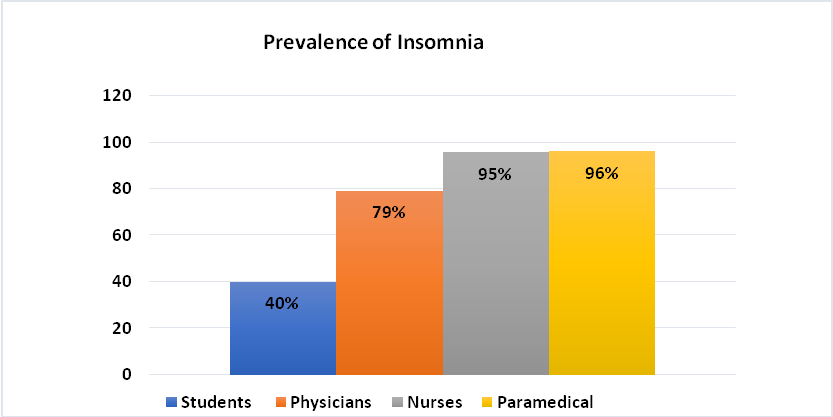
Figure 2: Prevalence of insomnia among study participants.
With the brewing cascade of events arising from the corona pandemic, many discerning feelings have led to the increased emotional and mental distress among health care workers. In this research, individuals were assessed on a series of questions to analyze psychological effects seen among health care workers during the current pandemic. It was seen that this pandemic led to significant anxiety and depression among health care workers. When compared to medical students’ subjects involved in direct patient care had significantly higher level of anxiety and depression. Zaki et al. reported similar findings. They reported fear of catching infection and feeling helpless a reason for observed depression and anxiety among their participants15, 6.
Arshad et al. reported 10% depression among health care workers in data collected from 3 metropolitan cities of Pakistan. They further reported 25% of the participants exhibited symptoms of anxiety. We observed a higher prevalence of anxiety and depression among nurses, which is like findings reported by Arshad et al. similar to our findings16. Parveen et al. also reported significantly higher rate of anxiety, stress and fear among a cohort of 100 health care workers. Direct patient contact is the most likely reason for escalating fear of catching infection and transmitting to the family members17.
Hayat et al. report a significantly mild level of depression and anxiety in a large cohort of 1094 health care workers of Pakistan. Symptoms of depression and anxiety were evaluated using patient Health questionnaire (PHQ-9) and Generalized Anxiety Disorders-7 (GAD-7). They found a higher level of anxiety among married female participants whereas depression was more prevalent among nurses18.
As one of the methods to break the chain for slowing/ending the transmission of the corona virus is quarantine and self-isolation, majority of subjects were of the opinion that decreased social activities elevated their level of anxiety causing further panic and stress. This was seen also in a study in India which focused on the impact of COVID-19 virus on the society and how community interactions and social connections were adversely affected leading to increased loneliness and depression19. Because of the increased fear of transmitting corona many individuals refrained from family gatherings especially elderly20. For the same reason majority of our subjects were avoiding visits to their relatives specially to avoid transmitting disease to elderly as they are more susceptible to severe disease.
Imposing travel bans was taken as an important move towards slowing spread of infection. The study showed that participants also had to cancel their travel plans, which they found was needed, but at the same time it led to symptoms of anxiety. Other studies also depicted similar findings on how thrusting such restriction during the pandemic had deteriorating consequences on a person’s mental health status21. However, an interesting outcome observed from this study was that due to common route of transmission people had become more aware and cautious in terms of self-hygiene disinfectants use. This indicates that even amid the current crisis, how self-awareness has made a huge impact on the daily living standards/ conditions of a person22,23.
Medical history has clearly shown role of vaccines in combating many infective diseases. To overcome this deadly pandemic scientists have rushed towards development of safe and effective vaccine. It is extremely important to know the perception of health care workers regarding COVID-19 vaccine. They are the most vulnerable group hence need to be vaccinated as a priority group. Moreover, their perception will have a direct effect on perception and willingness of society towards vaccination. Only about a third of our study participants were willing to take vaccine and to recommend it to the family members. Regarding effectiveness and safety of vaccine, majority of study participants were unsure due to insufficient data available. Our findings are in accordance with the findings of Paudel et al. They also reported only partial willingness of the health care workers for receiving vaccine24. Concerns regarding vaccine safety were the major reason for reported hesitancy. These observations can play critical role in designing educational programs for health care workers.
There are few limitations of the study. First, online collection of data limits involvement of health care workers having access to internet only. Secondly, there is a possibility of no response from those facing severe depression thus diluting the outcome. Thirdly, data were collected before introduction of COVID vaccination. It would be very helpful to analyze prevalence of psychological stress after COVID-19 Vaccination and to compare the changes in perception regarding effectiveness and safety of vaccine.
COVID-19 pandemic has led to significant anxiety and depression among health care workers, which is severe among front line health care workers involved in direct patient care. Development and execution of guidelines can help minimize the psychological and mental health issues.
We would like to acknowledge Jinnah Sind Medical University for allowing us to conduct this study. We are grateful to Ms Afsheen for her valuable input in designing the questionnaire and data collection.
The authors declare that there is no conflict of interest with respect to the research, authorship and/ or publication of this article.
The Jinnah Sind Medical University approved the study with the reference number (JSMU/IRB/2020/346).
The consents were taken prior to filling the forms.
HA generated concept, designed questionnaire, did literature search, and wrote manuscript. KI did literature search, data acquisition and statistical analysis. NM and OA did data acquisition and manuscript preparation. MN and HS did data acquisition, manuscript editing, and manuscript review.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579(7798):270-273.
- Asselah T, Durantel D, Pasmant E, Lau G, Schinazi RF. COVID-19: discovery, diagnostics and drug development. J Hepatol. 2021;74(1):168-184.
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. [Accessed 18 May 2021]. Available from: https://covid19.who.int.
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020; 22(395): e37-e38.
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395(10227):912-920.
- Zaki NFW, Sidiq M, Qasim M, Aranas B, Hakamy A, Ruwais NA, et al. Stress and psychological consequences of COVID-19 on health-care workers. J Nat Sci Med. 2020; 3:299-307.
- Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17-e18.
- DiGiovanni C, Conley J, Chiu D, Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004; 2(4):265-272.
- Calati R, Ferrari C, Brittner M, Oasi O, Olié E, Carvalho AF, et al. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J Affect Disord. 2019; 245:653-667.
- COVID-19 Situation! See the Realtime Pakistan and Worldwide 2021. [Internet]. Government of Pakistan, 2021 [cited 2021 Jun 16]. Available from: https://covid.gov.pk/
- Balkhi F, Nasir A, Zehra A, Riaz R. Psychological and behavioural response to the coronavirus (COVID-19) pandemic. Cureus. 2020;12(5):1-16.
- Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Mil Med Res. 2020; 7(1):1-10.
- Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020; 92(6):568-576.
- Sample size calculator. Retrieved from :http://www.raosoft.com/samplesize.html
- Ahmed HO. The impact of social distancing and self-isolation in the last corona COVID-19 outbreak on the body weight in Sulaimani governorate- Kurdistan/Iraq, a prospective case series study. Ann Med Surg (Lond). 2020; 59:110-117.
- Arshad MS, Hussain I, Nafees M, Majeed A, Imran I, Saeed H, et al. Assessing the impact of COVID-19 on the mental health of healthcare workers in three metropolitan cities of Pakistan. Psychol Res Behav Manag. 2020; 13:1047-1055.
- Parveen S, Awan S, Rabbani F, Pervaiz F, Khan A, Khan F, et al. Impact of covid-19 on mental health of healthcare workers during pandemic; an experience at a tertiary cardiac care set up. Pak Armed Forces Med J. 2020;70(4):S838-S842.
- Hayat K, Haq M, Wang W, Khan FU, Rehman AU, Rasool M, et al. Impact of the COVID-19 outbreak on mental health status and associated factors among general population: a cross-sectional study from Pakistan. Psychol Health Med. 2021:1-15.
- Singh J, Singh J. COVID-19 and its impact on society. Electronic Research Journal of Social Sciences and Humanities. 2020;2(1):168-172.
- Van Orden KA, Bower E, Lutz J, Silva C, Gallegos AM, Podgorski CA, et al. Strategies to promote social connections among older adults during ‘social distancing’ restrictions. Am J Geriatr Psychiatry. 2021;(8):816-827.
- Ranasinghe R. Karunarathna C, Pareedapamali J. After corona (COVID-19) impacts on global poverty and recovery of tourism-based service economies: An appraisal. Int J Tour Hosp. 2021;1(1):52-64.
- Assefa D, Melaku T, Bayisa B, Alemu S. Knowledge, attitude and self-reported performance and challenges of hand hygiene using alcohol-based hand sanitizers among healthcare workers during COVID-19 pandemic at a tertiary hospital: A cross-sectional study. Infect Drug Resist. 2021;14:303-313.
- Chatterjee K, Chauhan VS. Epidemics, quarantine, and mental health. Med J Armed Forces India. 2020; 76(2):125-127.
- Paudel S, Palaian S, Shankar PR, Subedi N. Risk perception and hesitancy toward COVID-19 vaccination among healthcare workers and staff at a medical college in Nepal. Risk Manag Healthc Policy. 2021;14:2253-2261.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
