By Tashmina Taha, Sheema Yousuf, Duriya Rehmani
AFFILIATIONS:
- Patel Hospital Karachi, Gulshan-e-Iqbal, Karachi, Pakistan.
ABSTRACT
Background: Cervical cancer is a major public health problem in developing countries due to ineffective screening programs. This study aimed to determine the accuracy of visual inspection with acetic acid (VIA) for cervical cancer screening in low-income population.
Methods: This cross-sectional study was conducted in an outdoor clinic of Dow University Hospital from July 2016 to July 2017. A total of 108 women with vaginal discharge, post coital bleeding, inter menstrual bleeding and dyspareunia were enrolled in the study. A solution of 5% acetic acid was applied to the cervix and examined under adequate light for 1 min. VIA was reported as positive or negative according to acetowhite changes. Positive results were confirmed by biopsy. SPSS was used for statistical analysis. Sensitivity and specificity were calculated. Chi Squared test was applied and p-value ≤0.05 was considered statistically significant.
Results: The average age of the patients was (mean± SD) 45.67±9.67 years. Out of forty-two patients who were VIA positive, n=38 had biopsy confirmed malignancy compared to seventeen women from the screened negative population (n=66) showing a sensitivity of 69.1% and specificity of 92.5%. We found 100% sensitivity and specificity in primipara. The positive predictive value (90.5%), negative predictive value (74.5%) and diagnostic accuracy of VIA positive were 80.6% respectively.
Conclusion: VIA is a simple, cost effective and reliable screening test in low socioeconomic areas allowing instant diagnosis and treatment (p=0.0005). Thus, it decreases the chance of loss to follow-up and the number of visits to a healthcare provider.
Keywords: Cervical Cancer; Visual Inspection with Acetic Acid; Screening.
Cervical cancer is the fourth commonest cancer in the world and approximately ninety percent of cases are found in developing countries with a disease burden of 493,000 cases and 273,000 deaths1,2. Globally it is the second commonest gynaecological malignancy3. However, it can be prevented by treating at premalignant stage using proper screening tools4. Invasive cervical disease is heralded by premalignant cervical intra epithelial neoplasia (CIN) so the goal of screening is detection and treatment of pre-cancer stage before it progresses to advanced stage5. Cancer of the cervix is the only malignancy, which can be prevented by structured screening program6.
The cervix is the lower fibro muscular portion of the uterus and appears reddish in colour on visual inspection. The ectocervix is composed of squamous epithelium whereas the endo-cervix is covered with columnar epithelium and the junction between the two is called squamocolumnar junction (SCJ). The location of SCJ changes progressively throughout the reproductive age. The region of the cervix where squamous metaplasia (physiological replacement of everted columnar epithelium on the ectocervix by a newly formed squamous epithelium) occurs is called the transformation zone, which is the site for greater than ninety percent of precancerous lesions7.
Cervical cancer affects women in the fifth to sixth decade of life9. The risk factors include human papilloma virus infection (HPV), early age at first intercourse, multiple sexual partners, smoking and low socioeconomic status. Approximately 99% of cases are linked to high-risk HPV infection. Primary prevention is possible by HPV vaccination and secondary prevention by screening and treating early disease. Different cervical cancer screening methods include cytology-based screening (Pap smear), visual inspection of the cervix with acetic acid (VIA) or Lugol’s iodine solution, colposcopy, and HPV test. The rationale behind VIA is that precancerous lesions appear white after staining with 3%-5% acetic acid7. It dehydrates cells so that abnormal squamous cells reflect light and appear white. Although the Pap smear is the most common type of screening used in the developed countries and is highly effective there is a dire need for a simpler method that can be interpreted rapidly allowing treatment at the same visit.
Numerous studies have been conducted in this regard so far showing variable sensitivity and specificity. Therefore, this study was performed to determine the accuracy of visual inspection with acetic acid (VIA) as a potential screening tool to rapidly detect any underlying cervical disease before it progresses to invasive cancer thus limiting the number of hospital visits.
A cross sectional study was carried out in the Gynaecology outpatient unit of Dow University Hospital from July 2016 to July 2017. Samples were collected by using the non-probability consecutive sampling technique. The study was started after permission from the ethical review board (IRB-545/DUHS/14). Written informed consent was obtained from all participants. A total of 108 sexually active women age 30 to 70 years attending OPD with vaginal discharge from 1 year, dyspareunia, post coital and intermenstrual bleeding from 6 months were enrolled in the study. Patients with active vaginal bleeding (confirm upon history), previous abnormal cervical cytology, pregnancy and those diagnosed with cervical cancer were excluded from the study. Patients with severe cervicitis were also excluded from the study.
Patients were properly counselled and explained the procedure and given a free choice of withdrawing from the study at any time. All the participants were ensured about confidentiality. Detailed clinical data were obtained and noted on structured proforma. After taking relevant history and physical examination, a pelvic examination was done taking care of dignity and privacy. The cervix was visualized using Cusco speculum and squamocolumnar junction was identified. A cotton swab was used to apply 5% acetic acid solution and the cervix was examined under adequate light for 1 min with 100-watt illumination with the naked eye. Visual inspection with acetic acid (VIA) was reported as positive or negative according to acetowhite changes. A positive test was characterized by opaque, dense, well defined acetowhite areas at or near squamocolumnar junction. The absence of colour change was considered a negative test. Those with positive VIA were subjected to biopsy taken at the same visit for confirmation. The biopsy sample was fixed with formalin solution and sent for histopathological examination.
Statistical analysis was performed by using SPSS. Mean and the standard deviation was calculated for age and parity. The proportion was calculated for discharge per vaginal, post coital bleeding, intermenstrual bleeding, and dyspareunia. Sensitivity and specificity were calculated two into two contingency tables. Stratification of diagnostic accuracy of VIA in the detection of cervical cancer by age, parity, diabetes, hypertension and smoking status was done. Chi-squared test was applied and p-value ≤0.05 was considered as statistically significant.
A total of 108 married women attending OPD majority of the participants were greater than 40 years old and multiparous. Sixty-three patients were housewives while there were forty-five working women. The distribution of patients according to age, parity, diabetes, hypertension and smoking status is shown in Table 1. Vaginal Discharge and post coital bleeding were the commonest presenting complaints (Figure 1).
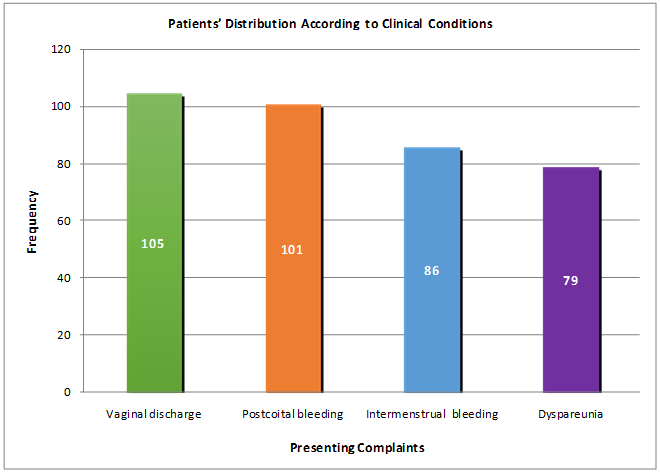
Figure 1: Distribution of patients according to clinical presentation.
Out of 42 patients who screened positive with VIA, thirty-eight were diagnosed with cervical cancer on biopsy while 17 women from the screened negative population (n=66) had biopsy (Figure 2) confirmed cervical cancer thus making a sensitivity of 69.1% and specificity of 92.5% (Table1).
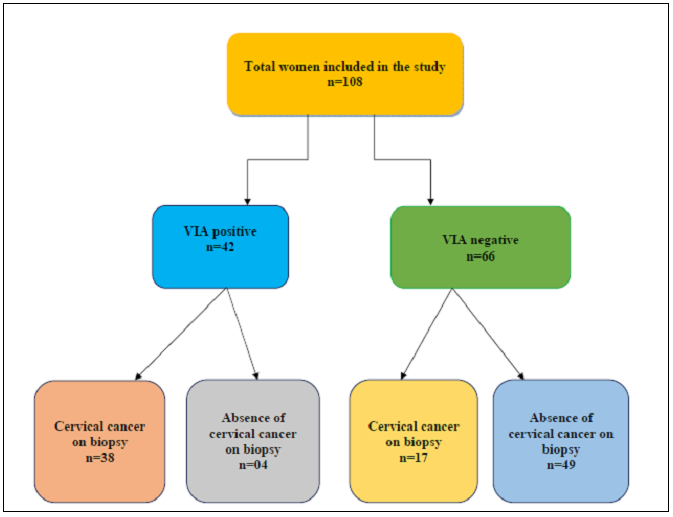
Figure 2: Flow chart showing output of visual inspection with acetic acid (VIA) for cervical cancer screening.
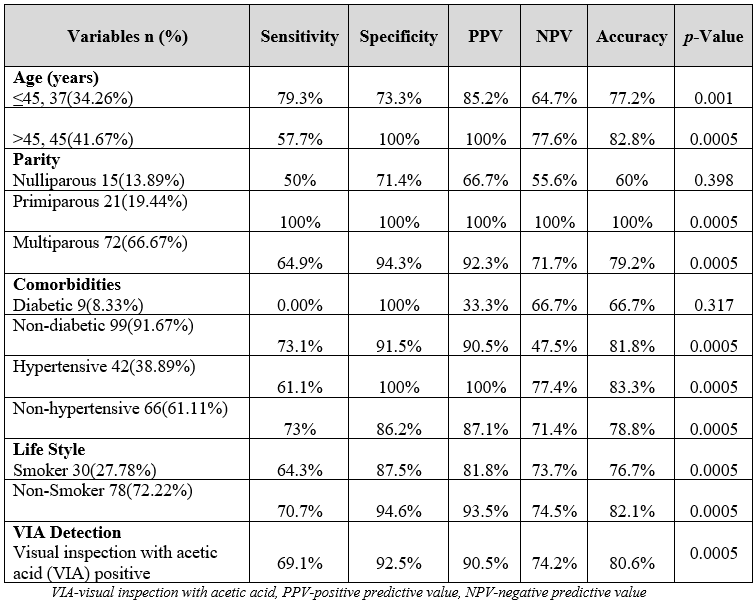
The positive predictive value (PPV) and negative predictive value (NPV) and diagnostic accuracy was 90.5%, 74.2% and 80.6% respectively. Stratification analysis was performed for accuracy of VIA in detection of cervical cancer by age, parity, diabetic, hypertension and smoking status of the women (Table 1). In primiparous women the diagnostic accuracy of VIA was found to be 100 percent with a p-value of 0.0005 which is statistically significant as shown in Table 1.
Table 1: Stratification of diagnostic accuracy of visual inspection with acetic acid (VIA) in detection of cervical cancer by age, parity, diabetes, hypertension and smoking status.
In the present study, the average age of the patients was 45.67±9.67 years and the majority were homemakers (58.13%). Our research showed that VIA had a low sensitivity (69.1%) but high specificity (92.5%) for cancer detection. The positive predictive value, negative predictive value and accuracy were 90.5%, 74.2%, 80.6% respectively. These results were comparable to other research studies such as shown by Mustafa et al. (sensitivity 77% and specificity 82%) and El Sokkary (sensitivity of 70.4%, specificity 77.6%, PPV 44% and NPV of 91.3%)8,9. In a meta-analysis by Sauvaget et al., data was collected from 26 studies conducted in high- and low-income countries showed a sensitivity of 80% and a specificity of 92% 10-12. In another study from Bangladesh, Rashid et al. found a sensitivity of 76.5% and specificity of 91.8% thus making it a useful screening tool to diagnose invasive and pre-invasive lesions of the cervix7.This contrasts with Vahedpoor et al., which showed a higher sensitivity but lower specificity13. In various studies, the average sensitivity and specificity ranged from 16.6-82.6% and 82.1-96.8% respectively14. A recent meta-analysis in sub-Saharan Africa showed pooled sensitivity and specificity of VIA to be 82.4% and 87.4% respectively15.
Although cervical cytology is the most used screening method and resulted in the dramatic decline of cervical cancer incidence in most developed countries. However, according to World Cancer Statistics, majority of the cases are found in underdeveloped countries due to a lack of awareness and hurdles in running Pap smear test because it requires high technology, well-experienced staff and high costs, which are not readily available in all developing countries and in all places16. Other factors contributing to the failure of the screening program include complexness of the process, inadequate government funding, poverty, socio-religious and cultural barriers, limited access to the hospital, inadequate follow-up, lack of knowledge and information and infrastructure10. In a world, health survey crude coverage of screening in resource-limited countries was found to be only 45%, for example, over 90 % of women in Malawi, Ethiopia and Bangladesh reported never had a pelvic exam17.
Additionally, only a small number of women at risk are screened because of the lack of trained technologists and laboratories and non-affordability. Due to some problems research studies have been conducted on alternative tests, including VIA which is simple to perform, no technology needed and the result is available within minutes. It can be performed by any healthcare worker with a low level of training making VIA a good alternative for low-resource settings. Some of the previous reports observed that it could reach similar or better results than the Pap smear in the detection of cervical intraepithelial neoplasia (CIN)18. VIA can be used as a primary screening test instead of cytology in developing countries where cervical cytological services are suboptimal as it has a sensitivity of 66% to 96% and specificity between 69% to 90% consistent with various studies2,19. Studies have shown that VIA has a true positive rate comparable to Pap smear and also permits treatment and referral at the same visit by detecting pre-invasive cervical lesions in both low-resource and well-equipped health facilities18,20. It is shown by Consul et al. in their study that VIA and VILI (visual inspection with Lugol’s iodine) had sensitivity comparable to Pap smear and can thus be a suitable alternative/adjunctive test not only in a resource-poor setting but in well-equipped centres also21. Another study by Nessa et al. in Bangladesh reported that VIA can be considered as a useful screening test with a good sensitivity of 88.9%.22
VIA can reliably be performed by both nurses and doctors in the presence of good training and sustained quality assurance23-25. However, a study from Congo by Raifu et al. showed limitation of the test as positivity rates of VIA performed by nurses and physicians differed significantly (36.3% versus 30.2%, respectively). Accordingly, there is need for thorough quality assurance by adequate training and re-training of service providers25-27. A study conducted in Bangladesh reaffirmed the sensitivity and specificity of 93.6% and 58.2% respectively of VIA in one hundred women by trained personnel thus suggesting it as a beneficial screening tool28.
It is shown in research that single visit approach leads to significant decrease in high-grade cervical lesions and is regarded as a safe and acceptable approach in various developing countries. It also helps in overcoming barriers of time, distance and loss to follow-up because recalling patient for additional tests or treatment can be critical to a programme’s success29,30. Lack of readily available cost-effective point of care screening tools has resulted in poor implementation of population-based screening programs in these settings17. Furthermore, most patients are lost to follow up even after submitting their Pap smear samples due to lack of education, awareness and limited access to hospital. To the best of our knowledge, VIA is a simple and cost-effective test with wide coverage. Hence, it can be considered as a useful screening method for underdeveloped areas, which allows see and treat policy thus reducing the burden of cervical malignancy.
The increasing burden of cervical cancer in low socioeconomic states is due to non-existent or poor administration of cost-effective preventive programs. Because of its rapidity and simplicity, visual inspection with acetic acid (VIA) can be considered as a reliable alternative to cytological test in these population as a screen and treat policy. There should be organized cervical screening awareness programs to encourage women for cervical check.
We are thankful to the DOW University of Health Sciences (DUHS) for supporting the study.
There was no conflict of interest among the authors.
The Ethical Board of DUHS approved the study with the ERC Ref number: IRB-545/DUHS/14.
Verbal and written consents were obtained from all patients.
TT was involved in randomization of patients, data collection and analysis, literature review and authored the study. SY was involved in literature review, result, discussion and reference writing. DR helped in data collection and statistical analysis.
- World Health Organization. Cervical cancer [Internet]. World Health Organization; 2018 [cited 2020 Aug 21]. Available from: http://www.who.int/cancer/ prevention/diagnosis-screening/cervical-cancer/en/
- Bano A, Haq G, Sheikh A. Pap smear versus visual inspection of cervix with acetic acid (VIA) for detection of cervical abnormalities. Pak J Surg. 2013;29(1):46-51.
- Shehkhar S, Sharma C, Thakur S, Raina N. Cervical cancer screening: knowledge, attitude and practices among nursing staff in a tertiary level teaching institution of rural India. Asian Pac J Cancer Prev. 2013;14(6):3641-3645.
- Hedge D, Shetty H, Shetty P, Rai S, Manjeera L, Vyas N, et al. Diagnostic value of VIA comparing with conventional pap smear in the detection of colposcopic biopsy proved CIN. Nepal J Obstet Gynaecol. 2011;6(1):7-12.
- Garg P. Evaluation of visual inspection with acetic acid (VIA) and visual inspection with Lugol’s Iodine (VILI) as a screening tool for cervical intraepithelial neoplasia in comparison with cytologic screening. Webmedcentral Obstet Gynaecol. 2011;2(6):1-10.
- Saslow D, Solomon D, Lawson HW, Killackey M, Kulasingam SL, Cain J, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. CA Cancer J Clin. 2012;62(3):147-172.
- Rashid MH, Ahmed MM, Chowdhury S, Ahmed S. Effectiveness of visual inspection with acetic acid as a test for cervical cancer screening. Int J Noncommun Dis. 2017;2(1):3-7.
- El Sokkary HH. Comparison between Pap smear and visual inspection with acetic acid in screening of premalignant cervical intraepithelial lesion and subclinical early cancer cervix. Int J Reprod Contracept Obstet Gynecol. 2016;6(1):54-59.
- Mustafa RA, Santesso N, Khatib R, Mustafa AA, Wiercioch W, Kehar R, et al. Systematic reviews and meta-analyses of the accuracy of HPV tests, visual inspection with acetic acid, cytology, and colposcopy. Int J Gynecol Obstet. 2016;132(3):259-265.
- Catarino R, Petignat P, Dongui G, Vassilakos P. Cervical cancer screening in developing countries at a crossroad: Emerging technologies and policy choices. World J Clin Oncol. 2015;6(6): 281-290.
- Sauvaget C, Fayette JM, Muwonge R, Wesley R, Sankaranarayanan R. Accuracy of visual inspection with acetic acid for cervical cancer screening. Int J Gynecol Obstet. 2011;113(1):14-24.
- Murillo R, Luna J, Gamboa O, Osorio E, Bonilla J, Cendales R, et al. Cervical cancer screening with naked-eye visual inspection in Colombia. Int J Gynecol Obstet. 2010;109(3):230-234.
- Vahedpoor Z, Behrashi M, Khamehchian T, Abedzadeh-Kalahroudi M, Moravveji A, Mohmadi-Kartalayi M. Comparison of the diagnostic value of the visual inspection with acetic acid (VIA) and Pap smear in cervical cancer screening. Taiwan J Obstet Gynecol. 2019;58(3):345-348.
- Adsul P, Manjunath N, Srinivas V, Arun A , Madhivanan Implementing community-based cervical cancer screening programs using visual inspection with acetic acid in India: A systematic review. Cancer Epidemiol. 2017; 49:161-174.
- Fokom-Domgue J, Combescure C, Fokom-Defo V, Tebeu PM, Vassilakos P, Kengne AP, et al. Performance of alternative strategies for primary cervical cancer screening in sub-Saharan Africa: systematic review and meta-analysis of diagnostic test accuracy studies. BMJ. 2015;351:1-11.
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359-E386.
- Gupta R, Gupta S, Mehrotra R, Sodhani P. Cervical screening in resource constrained countries: current status and future directions. Asian Pac J Cancer Prev. 2017;18(6):1461-1467.
- Agarwal S, Gupta R, Agarwal A, Pandey K, Gupta N, Katiyar A. Visual inspection with acetic acid for cervical cancer screening in a tertiary health care centre. Int J Reprod Contracept Obstet Gynecol. 2016; 5:752-576.
- Naz U, Hanif S. Agreement between visual inspection with acetic acid and papanicolaou’s smear as screening methods for cervical cancer. J Coll Physicians Surg Pak. 2014;24(4):228-231.
- Silkensen SL, Schiffman M, Sahasrabuddhe V, Flanigan JS. Is it time to move beyond visual inspection with acetic acid for cervical cancer screening? Glob Health Sci Pract. 2018;6(2):242-246.
- Consul S, Agrawal A, Sharma H, Bansal A, Gutch M, Jain N. Comparative study of effectiveness of Pap smear versus visual inspection with acetic acid and visual inspection with Lugol’s iodine for mass screening of premalignant and malignant lesion of cervix. Indian J Med Paediatr Oncol. 2012;33(3):161-165.
- Nessa A, Nahar KN, Begum SA, Anwary SA, Hossain F, Nahar K. Comparison between visual inspection of cervix and cytology based screening procedures in Bangladesh. Asian Pac J Cancer Prev.2013;14 (12):7607-7611.
- Shastri SS, Mittra I, Mishra GA, Gupta S, Dikshit R, Singh S, Badwe RA. Effect of VIA screening by primary health workers: randomized controlled study in Mumbai, India. J Natl Cancer Inst. 2014;106(3):1-7.
- Sherigar B, Dalal A, Durdi G, Pujar Y, Dhumale H. Cervical cancer screening by visual inspection with acetic acid – interobserver variability between nurse and physician. Asian Pacific J Cancer Prev. 2010; 11:323-326.
- Raifu AO, El-Zein M, Sangwa-Lugoma G, Ramanakumar A, Walter SD, Franco EL, et al. Determinants of cervical cancer screening accuracy for visual inspection with acetic acid (VIA) and lugol’s iodine (VILI) performed by nurse and physician. PLoS One. 2017;12(1):1-13.
- Parham GP, Mwanahamuntu MH, Kapambwe S, Muwonge R, Bateman AC, Blevins M, et al. Population-level scale-up of cervical cancer prevention services in a low-resource setting: development, implementation, and evaluation of the cervical cancer prevention program in Zambia. PLoS One. 2015;10(4):1-19.
- Schiffman M, Castle PE. The promise of global cervical-cancer prevention. New Engl J Med. 2005;353(20):2101-2104.
- Nessa A, Hussain MA, Rahman JN, Rashid MH, Muwonge R, Sankaranarayanan R. Screening for cervical neoplasia in Bangladesh using visual inspection with acetic acid. Int J Gynecol Obstet. 2010;111(2):115-118.
- Graffikin L, Blumenthal PD, Emerson M, Limpaphayom K. Safety, acceptability and feasibility of single visit approach to cervical cancer prevention in rural Thailand: a demonstration project. Lancet. 2003;361:814-820.
- Blumenthal PD, Graffikin L, Deganus S, Lewis R, Emerson M, Adadevoh S. Cervical cancer prevention: safety, acceptability and feasibility of a single visit approach in Africa, Ghana. Am J Obstet Gynecol. 2007;196:e1-e9.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
