By Asma Shabbir1, Umaima Tariq Khan2, Diya Nisar2, Parversh Kumar Rath2, Cheena Kumari3, Talat Zehra1, Syed Mehmood Hasan1
AFFLIATIONS:
- Department of Pathology, Sindh Medical College, Jinnah Sindh Medical University, Karachi, Pakistan.
- Student, Sindh Medical College, Jinnah Sindh Medical University, Karachi, Pakistan.
- House Officer, Sindh Medical College, Jinnah Sindh Medical University, Karachi, Pakistan.
ABSTRACT
Background: Prostatic diseases are a leading cause of frequent urinary complaints in elderly males. The most common diseases include prostatitis, benign prostatic hyperplasia, and prostate cancer. This study aimed to determine the frequency of the prostatic diseases, their trend over the years, and the association of age and diagnosis.
Methods: A retrospective descriptive study was conducted in Basic Medical Sciences Institute (BMSI) at Jinnah Postgraduate Medical Centre, Karachi. Data was collected from the histopathological files and all the cases diagnosed from 2014 to 2018 were included. Statistical analysis was done using SPSS with 95% confidence interval and p-value of ≤ 0.05 was considered significant. The Chi-square test was applied to find the association with age and year of diagnosis.
Results: Total 163 prostate cases were documented from 2014 to 2018, out of which 98 (60.1%) were of benign prostatic hyperplasia, which was most commonly diagnosed in men aged, 61-70. Prostatic adenocarcinomas having Gleason scores 8-10 were frequent and commonly seen in men aged 51-60 years. An increasing trend (p-value=0.053) was observed in the diagnosis of these prostatic diseases within these five years.
Conclusion: Benign prostatic hyperplasia is the most frequently (p-value=0.140) diagnosed prostatic disease in men, followed by adenocarcinoma and prostatitis. Advanced stage prostatic adenocarcinoma was diagnosed more frequently 17(10.4%) and at an earlier age. There is an increase in the number (p-value=0.053) of cases of prostatic diseases diagnosed each year. National-level studies and health policies are needed to facilitate early diagnosis and treatment.
Keywords: Prostate; Prevalence; Benign Prostatic Hyperplasia; Prostatic Cancer; Gleason Score; Prostatitis.
The prostate is an important exocrine gland that is anatomically located underneath the urinary bladder and is a part of the male reproductive system. It synthesizes and secretes prostatic fluid, a component of semen, which helps in the protection and nourishment of sperms. The prostate gland also assists in the ejaculation of semen into the urethra by contraction of its muscles. As the age advances, this gland becomes susceptible to many diseases such as inflammation, infections, benign enlargement, and neoplasia. These disorders are an important cause of frequent urinary complaints such as poor flow, nocturia, frequency, and urgency; commonly referred to as lower urinary tract symptoms (LUTS) in the ageing male population1. Lower urinary tract symptoms negatively influence the patient’s quality of life and these patients reported depressive symptoms and diminished sexual activity more frequently than those without lower urinary tract symptoms diminish. Moreover, patients with LUTS also reported poor overall health and decreased productivity at work due to their symptoms2.
Prostatitis is defined as a surge in the inflammatory cells present in the prostate following an infectious or inflammatory cause which may present as acute bacterial prostatitis, chronic bacterial prostatitis, a chronic pelvic pain syndrome, or asymptomatic prostatitis3. It is the third most commonly diagnosed urinary tract disease in men, following benign prostatic hyperplasia and prostate cancer4. Previous studies suggested that prostatitis could be associated with or lead to the development of other diseases of the prostate gland like benign prostatic hyperplasia and prostate cancer5,6.
Benign prostatic hyperplasia (BPH) is a very common histological diagnosis of prostatic diseases in ageing men. It can be described as the benign overgrowth of prostatic tissue, which results in glandular enlargement, leading to constriction of the urethra and ultimately causing lower urinary tract symptoms and urinary retention7. According to a global study, the prevalence of benign prostatic hyperplasia was found to be 14.8% at 40 years of age and 36.8% in ages 80 and above8. This suggests that the prevalence of BPH increases with increasing age. Another study conducted in North America reported that about 50% to 75% of men over the age of 50 years and about 80% of men over the age of 70 years suffered from benign prostatic hyperplasia and associated LUTS9.
Prostate cancer is the second most common malignancy diagnosed in males after lung cancer and is the fourth leading cause of mortality in males worldwide (6.7% of total male mortality by cancer)10. The incidence rates are highest in developed countries like Australia/New Zealand (86.4%), Northern Europe (85.7%), Western Europe (75.8%), and North America (73.7%) 11. Studies have reported that there is a direct correlation between the Human Development Index (HDI) of a country and the incidence of prostate cancer. Therefore, the incidence rate of prostate cancer, which used to be relatively lower in the developing Asian countries, is seen to be increasing steadily over the past decade and this may be due to the adoption of western lifestyles and excessive fatty diet12,13. Asian countries with high HDI such as Israel, Turkey, Lebanon, Singapore, Japan, and South Korea were seen to have a higher incidence of prostate cancer and this incidence is predicted to increase significantly in the future14. It has become the sixth most frequent cancer among men in Asia, the average mortality rate being 3.8 per 100,00015.
The number of cases of prostate cancer documented in Pakistan has increased in the past decade. According to the Karachi Cancer Registry (KCR), there has been a 60% rise in the prostate cancer cases observed from 1995-200216. A recent study shows that the overall prevalence of prostate cancer in Pakistan is 5%17. Cancer registry of Shaukat Khanum Memorial Cancer Hospital for the year 2018 reported prostate cancer to be the most common malignancy diagnosed in males18. Punjab Cancer Registry report of 2018 documented that prostate cancer is the second most frequently diagnosed cancer of males19. Unfortunately, despite the high prevalence of prostatic diseases, no recent studies have been conducted related to all prostatic pathologies in Karachi. Therefore, this study aimed to identify the frequency of prostatitis, benign prostatic hyperplasia, and prostate cancer at a tertiary care hospital in Karachi. Furthermore, the trends of these diseases over the study period from 2014-2018, and the association of each condition with the age of the patient had also analysed. This will help in better prevention, earlier diagnosis, and treatment of those affected by these diseases and serve as a starting point for future research.
A descriptive cross-sectional study was conducted to evaluate the frequency of different prostatic diseases in Karachi (prostatitis, benign prostatic hyperplasia, and prostatic cancer) and to assess their possible association with age. After getting approval from the Institutional Review Board (IRB number: JSMU/IRB/2019/-192), data was collected from the histopathological records present at the Basic Medical Sciences Institute (BMSI) at Jinnah Postgraduate Medical Centre (JPMC). This data included the records of patients from diverse areas of the country as the location of the institution being a major tertiary care hospital. The authors noted down all histologically diagnosed patients with prostatitis, benign prostatic hyperplasia, and prostatic cancer from the year 2014 to 2018.
Cases of benign prostatic hyperplasia that were associated with prostatitis and prostate cancer were also noted. The biopsy specimens were transferred to 10% neutral buffer formalin and gross features of samples were examined. Paraffin blocks were prepared for subsequent staining and microscopy. Tissue sections (3-4 µm) were cut from paraffin blocks and treated with haematoxylin and eosin (H and E) stain. Then examine under the microscope. The registration number of each patient, year of diagnosis, age, histological diagnosis, and Gleason scores (for grading of prostate cancer) was also recorded. Furthermore, Gleason scores were stratified into four groups as follows: 2-4 (very low grade), 5-6 (low grade), 7 (medium grade), and 8-10 (high grade) 20. Cases with deficient data were excluded from the study.
After collection, the data was entered and statistically analysed using Statistical Package for the Social Sciences (SPSS) version 23.0. The frequency of each prostatic disease and mean age of the patients was calculated. The Chi-square test was applied to assess both the association of prostatic diseases with the age of the patients as well as to see the pattern of prostatic diseases over the 5 years being studied (2014-2018). Furthermore, an analysis was done to find the frequency of Gleason scores seen in different ages of prostatic cancer cases20. The authors set a 95% confidence interval and a p-value of ≤ 0.05 was considered significant.
The age of patients in this study ranged from 41 to 90 years in which most of the patients were between 61-70 years of age. From the data collected, 145 (88.9%) specimens were of benign prostatic hyperplasia, 17 (10.4%) were of prostate cancer and 1 (0.6%) was of prostatitis. Out of the 145 specimens (Table 1) of benign prostatic hyperplasia, 98 (60.1%) were of isolated BPH, 43 (26.4%) were associated with prostatitis, and 4 (2.5%) with metaplasia.
Table 1: Data from prostatic diseases according to age at diagnosis.
| Age in Years | Prostatitis
n(%) |
Benign Prostatic Hyperplasia
(BPH) n(%) |
BPH with Prostatitis
n(%) |
BPH with Metaplasia
n(%) |
Prostatic Adenocarcinoma
n(%) |
p-Value |
| 41-50 | 0 | 5 (3.1) | 3 (1.8) | 0 | 0 | |
| 51-60 | 0 | 30 (18.4) | 19 (11.7) | 1 (0.6) | 7 (4.3) | |
| 61-70 | 1 (0.6) | 52 (31.9) | 10 (6.1) | 3 (1.8) | 5 (3.1) | 0.140 |
| 71-80 | 0 | 11 (6.7) | 8 (4.9) | 0 | 4 (2.5) | |
| 81-90 | 0 | 0 | 3 (1.8) | 0 | 1 (0.6) | |
| Total | 1 (0.6) | 98 (60.1) | 43 (26.4) | 4 (2.5) | 17 (10.4) |
Chi-square test applied.
An increasing trend (Table 2) was observed in the number of prostatic diseases being diagnosed each year (p value= 0.053). There were 14.7% cases in 2014, 15.3% in 2015, 19.6% in 2016, 24.5% in 2017, and 25.8% in 2018. This increasing trend was particularly apparent in cases of isolated BPH and BPH with prostatitis. Out of the total cases of isolated BPH, 9.2% of cases were diagnosed in 2014, and this number grew to 14.1% in 2018. Similarly, cases of benign prostatic hyperplasia (BPH) with prostatitis grew from 3.1% in 2014 to 9.2% in 2018. No significant association was seen between the prostatic diseases and age at diagnosis (p-value= 0.140).
Table 2: Information related to different prostatic diseases over 5 years.
|
Diagnostic Parameters |
Year
n (%) |
p-Value | ||||
| 2014 | 2015 | 2016 | 2017 | 2018 | ||
| Prostatitis | 0 | 0 | 0 | 0 | 1 (0.6) | |
| Benign prostatic hyperplasia | 15 (9.2) | 20 (12.3) | 18 (11.0) | 22 (13.5) | 23 (14.1) | |
| Benign prostatic hyperplasia with prostatitis | 5 (3.1) | 2 (1.2) | 7 (4.3) | 14 (8.6) | 15 (9.2) |
0.053 |
| Benign prostatic hyperplasia with metaplasia | 2 (1.2) | 2 (1.2) | 0 | 0 | 0 | |
| Prostatic adenocarcinoma | 2 (1.2) | 1 (0.6) | 7 (4.3) | 4 (2.5) | 3 (1.8) | |
| Total | 24 (14.7) | 25 (15.3) | 32 (19.6) | 40 (24.5) | 42 (25.8) | 163
(100) |
Chi-square test applied.
Benign prostatic hyperplasia (Figure 1a, b) was most diagnosed in men aged between 61-70 years.
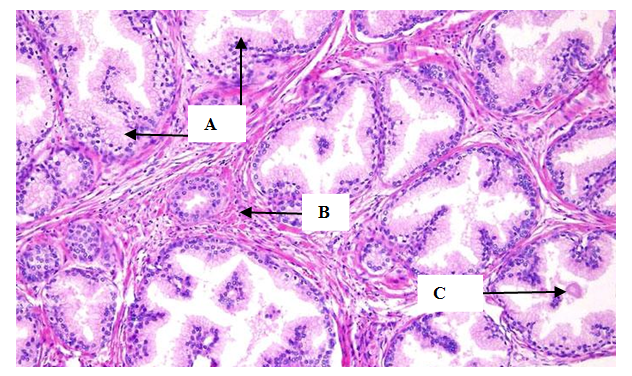
Figure 2a: Benign prostatic hyperplasia (H and E, 40x). Arrow A: Proliferating glands, Arrow B: Fibromuscular stroma arrow C: Corpora amylacea.
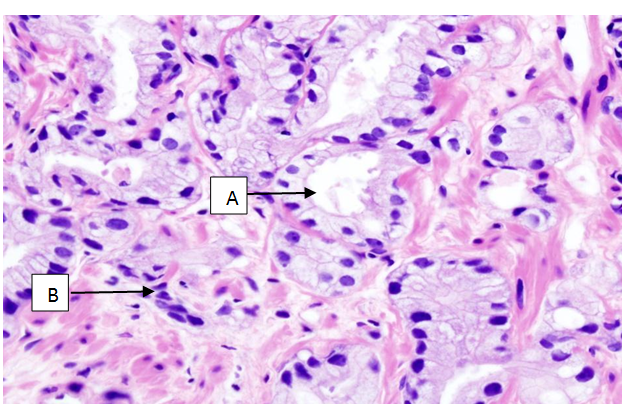
Figure 2b: Prostatic adenocarcinoma having Gleason score-7 (H and E, 40x). Arrow A: Small acinar arrangement, a few with well-formed lumina and back-to-back arranged glands, Arrow B: Less intervening stroma with malignant cells arranged in cords
Poorly differentiated cases of adenocarcinoma (Table 3) having Gleason scores 8-10 were seen to be more common in our study and were most commonly seen in men aged between 51-60 years (p-value=0.050).
Table 3: Gleason scores seen in different age groups.
| Age (years) | Gleason Score 2-4
n (%) |
Gleason Score 5-6
n (%) |
Gleason Score 7
n (%) |
Gleason Score 8-10
n (%) |
p-Value |
| 41-50 | 0 | 0 | 0 | 0 | |
| 51-60 | 0 | 0 | 0 | 7 (41.2) | |
| 61-70 | 0 | 1 (5.9) | 0 | 4 (23.5) | 0.050 |
| 71-80 | 0 | 0 | 1 (5.9) | 3 (17.6) | |
| 81-90 | 0 | 1 (5.9) | 0 | 0 |
Prostatic diseases remain the most common cause of lower urinary tract symptoms in the ageing male population worldwide. Prostatic diseases occurring in a patient interfere substantially with their quality of life, and if diagnosed late, may lead to poor prognosis and early death of the patient, in case of carcinoma.
The results of this study infer that benign prostatic hyperplasia was the most commonly diagnosed lesion of the prostate gland (88.9%), was isolated in most of the cases, and was most frequently seen in 61-70 years of age. Similar results have been found in a study conducted in India, a neighboring country of Pakistan21. A study conducted at Dow University of Health Sciences Karachi in 2013 reported the frequency of benign prostatic hyperplasia to be 87.5% 22. Another study, conducted in King Edward Medical University Lahore, reported their frequency to be 77.0% 23. The age group affected most frequently in both of these studies is 61-70 years, which is similar to this study. The similarity in these results can be explained by multiple studies conducted in the west, which show that the development of benign prostatic hyperplasia is strongly associated with age and it is often considered a normal part of the ageing process9,24. A literature review carried out in France using data from 1990 to 2018 also observed that the demographic trends and increase in expected lifespan has led to a steady rise in the prevalence of Benign prostatic hyperplasia (BPH) in many countries worldwide, making it a major health concern25.
Moreover, in this study, BPH was found to be associated with inflammation in some cases (26.4%), and very rarely with metaplasia (2.5%). The association of BPH with metaplasia is poorly understood but it has been suggested that hyperplasia may increase the risk of developing prostatic metaplasia especially in Asian populations15. This study also found an increasing trend in the number of cases of prostatic diseases over the study period. This rise is notably evident in the cases of benign prostatic hyperplasia. A mere 9.2% of the cases of isolated BPH were diagnosed in 2014, whereas, in 2018, this percentage raised to 14.1%. Such rise was also evident in the cases of BPH associated with inflammation (prostatitis), the lowest number of cases being reported in 2015 (1.2%), and the highest in 2018 (9.2%). The increase in the incidence of BPH may be associated with certain changes in the lifestyle and an increased life expectancy due to advancements in health care. Hence, screening processes should be regularly performed in elderly men and in individuals with a higher risk to promote early diagnosis and a better prognosis of the disease.
Prostate cancer was found in 10.4% of all the cases in the current study. The number was similar to the previous single-centre studies conducted in Karachi, Lahore, and Faisalabad, which reported their frequencies to be 12.5%, 13%, and 13.5% respectively22,26,27. The incidence of prostate cancer is said to be high in developed countries because of their lifestyle, but in recent years, it has been reported that this incidence is rising in the developing countries as well due to the rapid urbanisation and westernisation and modification of lifestyle10,12. In Pakistan, Shaukat Khanum Memorial Cancer Hospital and Punjab Cancer Registry have reported an increase in the number of cases diagnosed with prostate cancer in recent years18. According to the Punjab Cancer Registry, the incidence of prostate cancer has increased in the last three years, being 7.2% in 2016 and 8.3% in 201826. As presented in the Fourth Asian Prostate Cancer study meeting, various countries reported an increase in the number of cases being diagnosed. In China, the incidence of prostate cancer is rising more rapidly than any other cancer, it is also reported to be the third most common cancer of men in Singapore and its incidence is rising steadily in many other countries like Japan, Korea, Malaysia, and Vietnam27. However, such an increase in the cases of prostate cancer was not noted during this study.
Since cancer registry centers are not functional in Sindh, the exact frequency at which prostate cancer is being diagnosed in the province cannot be calculated. Hence, there is a dire need to establish regional as well as national cancer registry centers so that the overall frequency of prostate cancer can be calculated and compared with the statistics of other countries12.
In this study, it was also observed that almost half of the cases of prostate cancer documented in the last five years were diagnosed at an earlier age (<60 years). This finding may be associated with western studies where the incidence of prostate cancer was observed to be increasing in younger ages28. On the contrary, a study conducted in Peshawar reported their mean ages to be 65 years or older. Unfortunately, sufficient data is not available regarding the genetic variants in this society. Therefore, genetic screening for prostate cancer remains a clinical entity that may be beneficial in the early diagnosis of prostate cancer and requires more consideration28.
The Gleason score also has an important association with age at diagnosis. In our study, the scores of 8-10 were most common and were found throughout the fifth, sixth, and seventh decades of life. Additionally, the scores of 8-10 were mostly seen in men aged between 51-60 years. Studies conducted in the west have suggested that the probability of being diagnosed with a high Gleason score increases with increasing age29. However, such an age-related association was not observed in this research. Furthermore, the results of previous research carried out in Aga Khan University Hospital found Gleason score 7 to be the most common score in their study at the time of diagnosis28. However, there is no recent data available in the study population to compare and evaluate the possible causes of finding higher scores at the time of diagnosis. Possible reasons for this could be the rapid urbanization, changes in lifestyle, or exposure to carcinogenic substances, which lead to the disease occurring at an earlier age, and hence by the time of diagnosis, the disease has progressed to its later stages. Early pre-prostate-specific antigen (PSA) screening i.e., screening at or before 50 years of age, has been proven to be very helpful in predicting the diagnosis of advanced-stage prostate cancer later in life, therefore, it may be suggested that the screening processes for prostate cancer should be started earlier than that practiced now25.
One limitation of this study was that since this was a single-centre study, the data was not representative of the entire region. Furthermore, there is a lack of awareness about prostatic diseases in the general population, as proposed by a recent study conducted in Karachi, which reports that as much as 64% of men aged 45 and above were unaware of prostatic diseases and approximately 85% of them were not screened30. Therefore, patients may not be aware of these prevention practices and fail to consult a physician when the disease is at its initial stage. In this way, a large number of cases of prostatic diseases may either remain undiscovered or only become apparent when the disease has progressed into its late stage. This not only leads to poor prognosis, but it also means that many subclinical cases would be missed in this study sample. There is a dire need for awareness among the public regarding prostate health as well as the need for early screening practices so that diagnosis can be made before the disease progresses to an advanced stage. Additionally, more multicentre studies in Karachi and at the national level are needed to find out the frequency of prostatic diseases in our population30.
In this study, a higher prevalence of benign prostatic hyperplasia (88.9%) was observed as compared to the other prostatic diseases and it was seen to be most frequently diagnosed between the ages 61-70 years. Adenocarcinoma of the prostate, although less common overall (10.4%), was frequently of higher grade (Gleason score 8-10) and diagnosed in the younger age group of 51-60 years. An increasing trend in the number of prostatic diseases diagnosed each year was observed, most notably in cases of benign prostatic hyperplasia.
We would like to thank Prof. Shehnaz Kher and Dr. Naushaba Rahat for allowing us to collect data from the Basic Medical Sciences Institute at Jinnah Postgraduate Medical Centre (JPMC).
The authors declare no conflict of interest.
This research was initiated after obtaining approval from the Institutional Review Board of Jinnah Sindh Medical University, Karachi (IRB number: JSMU/IRB/2019/-192).
Not applicable since data was collected from the histopathological files and the study has been exempted from full IRB review.
AS contributed in conception and design of the study, acquisition, and analysis of data, and critical review of the manuscript. UT drafted the manuscript, and critically reviewed it. DN took part in critical analysis, data interpretation and manuscript writing. CK and PK also performed the data acquisition and critical review. TZ also collected the data, did the critical analysis and SMH preformed the critical review.
- Oyelekan A, Ogunsemi O, Afe T, Ayoade B, Nwokoro C, Oluyemi O, et al. Sleep quality and lower urinary tract symptoms among patients with prostatic diseases. Ann Afr Surg. 2020;17(2):69-71.
- Kim TH, Han DH, Ryu DS, Lee KS. The impact of lower urinary tract symptoms on quality of life, work productivity, depressive symptoms, and sexuality in Korean men aged 40 years and older: a population-based survey. Int Neurourol J. 2015;19(2):120-129.
- Smieško GM. Acute and chronic prostatitis. SANAMED. 2020;15(1):71-76.
- Khan FU, Ihsan AU, Khan HU, Jana R, Wazir J, Khongorzul P, et al. Comprehensive overview of prostatitis. Biomed Pharmacother. 2017;94:1064-1076.
- Repetto E, Sosa A, Colla R, Revol M, Metrebian E, Metrebian S. Relationship of prostatitis in the appearance of prostate cancer and benign prostatic hyperplasia. Revista Cubana de Urología. 2019;8(1):22-33.
- Zhang L, Wang Y, Qin Z, Gao X, Xing Q, Li R, et al. Correlation between Prostatitis, benign prostatic hyperplasia and prostate cancer: A systematic review and meta-analysis. J Cancer. 2020;11(1):177-189.
- María Molero J, Miñana B, Palacios‐Moreno JM, Téllez Martínez‐Fornes M, Lorite Mingot D, Agra Rolán A, et al. Real‐world assessment and characteristics of men with benign prostatic hyperplasia (BPH) in primary care and urology clinics in Spain. Int J Clin Pract. 2020;74(11):e13602:1-12.
- Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Sci Rep. 2017;7(1):7984:1-10.
- Egan KB. The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am. 2016;43(3):289-297.
- Ferlay J, Colombet M, Soerjomataram I, Mathers C, Parkin D, Piñeros M, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer. 2019;144(8):1941-1953.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
- Taitt HE. Global trends and prostate cancer: a review of incidence, detection, and mortality as influenced by race, ethnicity, and geographic location. Am J Mens Health. 2018;12(6):1807-1823.
- Hassanipour-Azgomi S, Mohammadian-Hafshejani A, Ghoncheh M, Towhidi F, Jamehshorani S, Salehiniya H. Incidence and mortality of prostate cancer and their relationship with the Human Development Index worldwide. Prostate Int. 2016;4(3):118-124.
- Pakzad R, Mohammadian-Hafshejani A, Ghoncheh M, Pakzad I, Salehiniya H. The incidence and mortality of prostate cancer and its relationship with development in Asia. Prostate Int. 2015;3(4):135-140.
- Chen R, Ren S, Yiu MK, Fai NC, Cheng WS, Ian LH, et al. Prostate cancer in Asia: a collaborative report. Asian J Urol. 2014;1(1):15-29.
- Bhurgri Y, Kayani N, Pervez S, Ahmed R, Tahir I, Afif M, et al. Incidence and trends of prostate cancer in Karachi South. Asian Pac J Cancer Prev. 2009;10(1):45-48.
- Idrees R, Fatima S, Abdul-Ghafar J, Raheem A, Ahmad Z. Cancer prevalence in Pakistan: meta-analysis of various published studies to determine variation in cancer figures resulting from marked population heterogeneity in different parts of the country. World J Surg Oncol. 2018;16(1):129-139.
- Collective Cancer Registry Report From December 1994 Till December 2018 [Internet]. Shaukat Khanum Memorial Cancer Hospital and Research Center, Pakistan; 2018 [cited 11 March 2020]. Available from: http://shaukatkhanum.org.pk/
- Punjab Cancer Registry Report [Internet]. 2018 [cited 1 February 2020]. Available from: http://punjabcancerregistry.org.pk/reports/PCR_2018.pdf
- Gordetsky J, Epstein J. Grading of prostatic adenocarcinoma: current state and prognostic implications. Diagn Pathol. 2016;11(1):25-32.
- Rajani R, Mehta N, Goswami H. Histopathological study of prostatic lesions at tertiary care centre. Int J Clin Diagn Pathol. 2020;3(2):172-176.
- Aslam HM, Shahid N, Shaikh NA, Shaikh HA, Saleem S, Mughal A. Spectrum of prostatic lesions. Int Arch Med. 2013;6(1):36-40.
- Sarwar A, Rathore Z, Rathore S, Butt R. Prostatic diseases common cause of morbidity in adult males. Pak J Med Health Sci. 2016;10(2):526-529.
- Vuichoud C, Loughlin KR. Benign prostatic hyperplasia: epidemiology, economics and evaluation. Can J Urol. 2015;22(Suppl 1):1-6.
- Dai X, Fang X, Ma Y, Xianyu J. Benign prostatic hyperplasia and the risk of prostate cancer and bladder cancer: a meta-analysis of observational studies. Med (Baltimore). 2016;95(18):3493:1-8.
- Punjab Cancer Registry Report [Internet]. 2016 [cited 3 March 2020]. Available from: http://punjabcancerregistry.org.pk/reports/PCR_2016.pdf
- Youl Lee J, Taniguchi T, Zhang K, Ng CF, Hakim L, Umbas R, et al. Report of the forth Asian Prostate Cancer (A-CaP) study meeting. Jpn J Clin Oncol. 2019;49(6):581-586.
- Rasul G, Khan I, Jan MA, Ahmad T, Khattak IU, Aslam M. Frequency of incidental prostate cancer in patients presenting with palpable enlarged prostate gland. J Postgrad Med Inst. (Peshawar-Pakistan). 2019;33(3):210-215.
- Muralidhar V, Ziehr DR, Mahal BA, Chen YW, Nezolosky MD, Viswanathan VB, et al. Association between older age and increasing Gleason score. Clin Genitourin Cancer. 2015;13(6):525-530.
- Tanveer M, Tahir F, Majid Z, Hussain MM, Asghar SA, Qadar LT, et al. Awareness and self care practices of elderly men regarding prostate diseases in Karachi, pakistan. Cureus. 2019;11(5):4617.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
