By Sadaf Ali1, Tasleem Hosein2, Khizra Rehman3, Rafia Ruaaz4, Yasir Raza5, Pooja Balani1
AFFLIATIONS:
- Department of Operative Dentistry, Ziauddin College of Dentistry, Karachi, Pakistan.
- Fatima Jinnah Dental College, Karachi, Pakistan.
- Department of Community and Preventive Dentistry, Ziauddin College of Dentistry, Karachi, Pakistan.
- Department of Oral Biology, Fatima Jinnah Dental College, Karachi, Pakistan.
- Department of Operative Dentistry, Muhammad Medical and Dental College, Mirpur Khas, Sindh, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-3/005
How to cite: Ali S, Hosein T, Rehman K, Ruaaz R, Raza Y, Balani P. Root Resorption Patterns of Primary Mandibular Molars and Location of Premolar Successors Through Radiographs in Pakistani Population. Pak J Med Dent. 2022;11(3): 24-29. doi: 10.36283/PJMD11-3/005
Background: Primary teeth undergo physiological root resorption followed by eruption of their permanent successors. Roots of primary mandibular molars can have either symmetrical or asymmetrical resorption patterns. This study aimed to determine the frequency of root resorption patterns of primary mandibular molars and the position of premolar successors through radiographs in children.
Methods: A total sample of 240 primary mandibular teeth from 140 patients (5-12 years) who visited the Paediatric Dentistry Department of Fatima Jinnah dental college were reviewed using radiographs. The root resorption patterns of primary mandibular molars and the location of the premolar successors were determined. Effect modifiers were controlled through stratification concerning age, gender, right or left side and presence of caries. Post-stratification chi-square analysis was used and p<0.05 was considered statistically significant.
Results: In primary first molars, 51(71%) root resorption was seen in the distal roots and 19(26%) of root resorption was symmetrical. In primary second molars, 81(48%) of root resorption was in the distal roots and 62(37%) was symmetrical. The distal location of the premolar was most common at 85(51%). Further, [31(89%) and 54(64%)] distal root resorption occurred when the first and second premolars were located distal to the long axis of the first and second molars respectively. The association between premolar location and root resorption pattern of the primary mandibular molars was highly significant (p<0.001).
Conclusion: A high number of asymmetrical root resorption of primary mandibular molars exists especially in distal roots 51 (71%) in Pakistani population. The mesial location of the premolar was least common.
Keywords: Root Resorption; Radiography; Bicuspid; Deciduous Tooth.
Root resorption is a physiological event for the primary teeth which leads to its exfoliation1,2. The pattern of root resorption is determined by several factors including the position of the permanent successor with the primary predecessor3. Root resorption is initiated on the side of the root which is nearest to the permanent tooth. Incomplete root resorption may disrupt the normal exfoliative process4. This series of events is controlled by odontoclasts in the root surrounding tissues. They have similar enzymatic and metabolic properties as osteoblasts5,6.
The pressure of the erupting permanent tooth plays a role in the resorption of primary teeth. Other factors which affect root resorption are the function of endocrine glands and nutrition. Deficiency in Vitamin A, C and D, calcium and magnesium, hypothyroidism and pituitary dwarfism can all delay the exfoliation of primary teeth1,3. The portions of the root which escape root resorption may be retained in the form of root fragments, which may cause the failure of eruption or ectopic eruption of the permanent successor or cyst formation. It may also lead to future crowding3.
Other factors which affect the exfoliation and eruption processes include occlusal trauma, elongation of the root, forces exerted by the vascular tissues surrounding the root, pull of the periodontal membrane, hormonal influences, presence of a viable dental follicle, pressure from the muscular action and resorption of the alveolar crest7,8. Dental caries have also been reported to accelerate the root resorption and eruption of the permanent successor9. It is the most prevalent chronic disease in the world,10 affecting 60% to 90% of school-aged children11. It harms children’s oral and general health as it can cause pain and swelling if it reaches the pulp12.
In another animal study by Baume et al., female rat incisors were observed in response to growth hormone, thyroxin and a combination of both. This study shows that both hormones in synergism control the tooth eruption13. Very few studies have been done worldwide on root resorption patterns of primary molars and the position of the premolar successors. To the best of our knowledge, this is the first study conducted on Pakistani children to assess the root resorption patterns of primary mandibular molars and the location of premolar successors.
Patients (n=240), who visited Fatima Jinnah Dental College Hospital (FJDC) Paediatrics Dentistry Department were selected for this descriptive cross-sectional study. The Institutional Ethical Review Committee of FJDC provided clearance for this study. Informed consent was taken from the parents. Digital radiographs were taken with Evolution x 3000 X-ray machine, by New Life Radiology, Italy, operating at 8 mA and 70 kV. A Paediatric digital sensor was used and a lead collar was provided. Inclusion criteria were: both male and female healthy patients aged between 5-12 years, Primary mandibular molars of both right and left sides and Clear images of the roots of the primary mandibular molars, cementoenamel junction (CEJ) and successor premolars. Known patients of any systemic disease such as diabetes, vitamin deficiency, or any chronic condition were excluded.
The exclusion criteria involved teeth with pulp treatment or periapical/furcation pathology, stainless-steel crowns, traumatized teeth with internal or external resorption seen in radiographs and diagnosed cases of dentinogenesis imperfecta, dentinal dysplasia or endocrine disturbances.
A total of 240 periapical radiographs were evaluated. The sample size was calculated using WHO Sample Size Calculator, Version 2.0.21. Keeping level of confidence at 95% and margin of error at 2.5%. To check the root resorption pattern, a line was drawn connecting the mesial and distal apices of the primary molar and another line was drawn connecting the cementoenamel junction of the primary molar at the mesial and distal sides. A pattern was defined as symmetrical if both these lines were parallel and asymmetrical if the lines were not parallel. If the line was tilting mesially then the mesial root was more resorbed and if the line was tilting distally then the distal root was more resorbed as shown in Figure 1. To check the premolar successor location a line was drawn through the long axis of the primary molar through the middle of the furcation and it was extended apically. The location of the premolar was defined as mesial, centered and distal as shown in Figure 2. All information was recorded in a pre-designed proforma by the researcher herself.
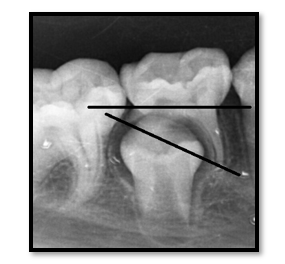
Figure 1: Asymmetrical root resorption.
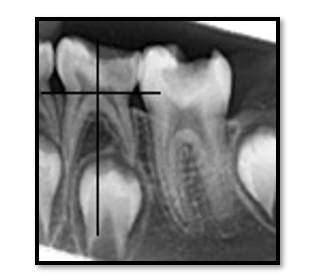
Figure 2: Premolar distal.
Data was collected in SPSS Version 23. The mean and standard deviation of the age was computed. Frequency and percentage were calculated for symmetry of root resorption, asymmetry of root resorption- mesial or distal resorption and premolar location-mesial, centered or distal. Effect modifiers were controlled through stratification for age, gender, right or left side and presence of caries. Post-stratification chi-square analysis was used with gender, side, age and presence of caries with p < 0.05 was considered statistically significant.
A total sample of 240 primary mandibular teeth from 140 patients was included in the study. The mean age was 8.46 ± 1.95 years ranging from 5 years to 12 years. The study included 134 (56%) males and 106 (44%) females. 114 (47.5%) of the teeth were left mandibular first and second molars and 126 (52.5%) teeth were right mandibular first and second molars. The distributions of the root resorption patterns of primary molars and the premolar successor location are shown in Table 1.
Table 1: Frequency of root resorption patterns of primary mandibular first and second molars and location of the premolar successors.
| Characteristics | Primary First Molar
n (%) 72 (100%) |
Primary Second Molar
n (%) 168 (100%) |
|
| Root resorption patterns | Distal Root More Resorbed | 51 (71%) | 81 (48%) |
| Symmetrical Root Resorption | 19 (26%) | 62 (37%) | |
| Mesial Root More Resorbed | 2 (3%) | 25 (15%) | |
| Location of the premolar successors | Distal to the long axis | 35 (49%) | 85 (51%) |
| Centered | 35 (49%) | 81 (48%) | |
| Mesial to long axis | 2 (2%) | 2 (1%) | |
The association between the root resorption patterns of primary mandibular molars and the location of premolar successors is shown in Table 2.
Table 2: Association between the symmetry of root resorption of the primary mandibular first and second molars and the location of the premolar successor.
| Features | Tooth | Distal Root Resorbed
n (%) |
Symmetry
n (%) |
Mesial Root Resorbed
n (%) |
p-Value |
| Primary mandibular first molar | Premolar mesially | 0 (0%) | 2 (100%) | 0 (0%) | 0.006 |
| Premolar centered | 20 (57%) | 13 (37%) | 2 (6%) | ||
| Premolar distally | 31 (89%) | 4 (11%) | 0 (0%) | ||
| Primary mandibular second molar | Premolar mesially | 0 (0%) | 0 (0%) | 2 (100%) | <0.001 |
| Premolar centered | 27 (33%) | 39 (48%) | 15 (19%) | ||
| Premolar distally | 54 (64%) | 23 (27%) | 8 (9%) |
Stratification was done concerning age, gender, side: right or left side and presence of caries. Post-stratification chi-square analysis was done to see the effect of these variables on outcome taking p<0.05 as significant.
Results showed that a higher percentage of children in the age group 5-8 years had symmetrical root resorption (41%) than in the older age group (25%). Children in the older age group of 9-12 years had more asymmetrical root resorption (75%) as compared to the younger age group (59%). Statistically, no significant results were observed to gender, side and presence of caries (p>0.05).
Physiological root resorption in primary teeth leads to the exfoliation of the teeth and allows the permanent teeth to erupt14,15. The dental pulp plays an important role in the resorption process16,17. Resorption starts between 1 and 3 years after the apical closure, followed by exfoliation after three years18,19. Asymmetrical root resorption may be due to several factors such as age, presence of caries/restorations, presence of pulpotomy, discrepancy in the size between the premolar and its predecessor and the position of the developing tooth in relation to the primary root20,21.
Cross-bites and other malocclusions can potentially develop if there is over retention of primary molars. Other complications include space loss, impaction of succedaneous teeth, tipping of adjacent teeth, supraeruption of opposing teeth and vertical bone loss. It can also lead to difficult extractions22. The findings of this study are like Peretz et al. in which over one-half (55%) of the root resorption in the primary first molar was in the distal root9. Another study done by Moorrees et al. had somewhat different results in which mesial roots resorbed earlier than the distal roots23. This difference could be due to different study populations or different methods of study.
In this study, the least amount of resorption was seen in the mesial roots of the primary mandibular teeth. Sharma et al. also had similar findings showing 3% mesial root resorption in primary first mandibular molars and 12% in primary second mandibular molars19. Most of the literature agrees with the findings of the present study. The premolar development starts between the divergent roots of the primary molars, and the position and size of the premolar affect the pattern of root resorption of primary molars24.
In the current study, 51% of the second premolars are located distally. Peretz et al. also observed that more than half (68%) of the permanent second premolars are located distally9. In the present study, the least number of premolars were located mesial to the long axis of both teeth, the results were very similar to the findings of the other studies5. The distal location of the premolar is intended for the future lateral expansion of the arch by using the “leeway” space5.
There was a significant association between the location of premolar successors and the root resorption pattern in the present study. These findings are like previous studies which reported 96% of distal root resorption in the primary first molar when the first premolar was placed distally19. Sahara reported that the resorption process is set off by the pressure of the erupting permanent tooth25. Harokopakis-Hajishengallis explained that the root resorption process starts at the site of the root which is closest to the permanent successor. This influences the root resorption pattern of the primary teeth1.
The study sample was divided into two groups according to age: 5-8 years and 9-12 years. Results showed that a higher percent (75%) of patients had asymmetrical root resorption in the older age group. This finding was supported by a study done by Prove et al., in which the prevalence of asymmetrical root resorption in the primary mandibular second molars was higher in the older age group of 9-10 years as compared to the lower age group of 7-8 years4.
One limitation of the current study was the sample size. Higher sample size is needed to draw firmer conclusions. In the future longitudinal studies should be done to see cause-and-effect relationships amongst different variables. Newer technology such as cone beam computed tomography (CBCT) should be used in further studies to better understand the factors which affect the asymmetrical root resorption. The findings of this study should be used to improve the practices in Paediatric dentistry. It is recommended that if a tooth is undergoing asymmetrical resorption, that tooth should be followed up until it exfoliates to prevent any root remnants and other malocclusions to develop.
A high number of asymmetrical root resorption of primary mandibular molars exists in the Pakistani population, especially in the distal roots. The location of the premolar between the primary roots influences the root resorption pattern of the primary mandibular molars. However, children in the older age group of 9-12 years showed more asymmetrical root resorption.
The authors would especially like to thank Dr. Shakeel Qutub Khan and Dr. Uzma Shahbaz from Fatima Jinnah Dental College for their assistance. They would also like to acknowledge the Paediatric Dentistry Department of Fatima Jinnah Dental College and Hospital for their facilitation in the data collection process.
There was no conflict of interest among the authors.
The study approval was obtained by Fatima Jinnah Dental College’s institutional ethical and scientific review board (BEH No. FEB-2015-OPR01).
The authors also affirm that no financial aid was received from any organization or institution during the research conducted for this study.
Conception and study design were done by TH. SA also contributed to the study concept along with data recording, analysis and interpretation. Data entry was performed by RR. In addition, KR and PB drafted the manuscript while critical revision of the article was done by YR and RR. SA approved and finalized the paper.
-
- Harokopakis-Hajishengallis E. Physiologic root resorption in primary teeth: molecular and histological events. J Oral Sci. 2007;49(1):1-12. doi: 10.2334/josnusd.49.1
- Consolaro A. Should deciduous teeth be preserved in adult patients? How about stem cells? Is it reasonable to preserve them? Dent Press J Orthod. 2016;21(2):15-27. doi: 10.1590/2177-6709.21.2.015-027.oin
- Murthy P, Bhojraj N, Hegde U. Pattern of physiologic root resorption in deciduous teeth at different stages. J Clin Diagn Res. 2020;14(6): ZC18-ZC22.
- Prove SA, Symons AL, Meyers IA. Physiological root resorption of primary molars. J Clin Pediatr Dent. 1992;16(3):202-206.
- Fukushima H, Kajiya H, Takada K, Okamoto F, Okabe K. Expression and role of RANKL in periodontal ligament cells during physiological root-resorption in human deciduous teeth. Eur J Oral Sci. 2003;111(4):346-352. doi: 10.1034/j.1600-0722.2003.00051.x
- Shimazaki E, Karakida T, Yamamoto R, Kobayashi S, Fukae M, Yamakoshi Y, et al. TGF-β and physiological root resorption of deciduous teeth. Int J Mol Sci. 2017;18(1):2-14. doi: 10.3390/ijms18010049
- Dos Santos CC, Melo DL, da Silva PP, Normando D. What is the survival rate of deciduous molars in cases with agenesis of premolar successors? A systematic review. Angle Orthod. 2022;92(1):110-117. doi: 10.2319/123020-1039.1
- Mulia DP, Indiarti IS, Budiarjo SB. Effect of root resorption of primary teeth on the development of its permanent successors: An evaluation of panoramic radiographs in 7–8 year-old boys. J Phys Conf Ser. 2018; 1073(3): p. 032015. IOP Publishing. doi :10.1088/1742-6596/1073/3/032015
- Peretz B, Nisan S, Herteanu L, Blumer S. Root resorption patterns of primary mandibular molars and location of the premolar successors: a radiographic evaluation. Pediatr Dent. 2013;35(5):426-429.
- Coll JA, Vargas K, Marghalani AA, Chen CY, AlShamali S, Dhar V, et al. A systematic review and meta-analysis of nonvital pulp therapy for primary teeth. Pediatr Dent. 2020;42(4):256-461.
- Urquhart O, Tampi MP, Pilcher L, Slayton RL, Araujo MW, Fontana M, et al. Nonrestorative treatments for caries: systematic review and network meta-analysis. J Dent Res. 2019;98(1):14-26. doi: 10.1177/0022034518800014
- Najjar RS, Alamoudi NM, El‐Housseiny AA, Al Tuwirqi AA, Sabbagh HJ. A comparison of calcium hydroxide/iodoform paste and zinc oxide eugenol as root filling materials for pulpectomy in primary teeth: A systematic review and meta‐analysis. Clin Exp Dent Res. 2019;5(3):294-310. doi.org/10.1002/cre2.173
- Baume LJ, Becks H, Ray JC, Evans HM. Hormonal control of tooth eruption: II. The effects of hypophysectomy on the upper rat incisor following progressively longer intervals. J Dent Res. 1954;33(1):91-103. doi: 10.1177/00220345540330011701
- Chhabra R, Rao S, Kumar BM, Shetty AV, Hegde AM, Bhandary M. Characterization of stem cells from human exfoliated deciduous anterior teeth with varying levels of root resorption. J Clin Pediatr Dent. 2021;45(2):104-111. doi: 10.17796/1053-4625-45.2.6
- Lee JE, Lee JH, Choi HJ, Kim SO, Song JS, Son HK, et al. Root resorption of primary teeth without permanent successors. J Korean Acad Pedtatr Dent. 2009;36(4):625-630.
- Rölling I. Histomorphmetric analysis of primary teeth during the process of resorption and shedding. Eur J Oral Sci. 1981;89(2):132-142. doi: 10.1111/j.1600-0722.1981.tb01663.x
- Wang C, Wang Y, Liu N, Cai C, Xu L. Effect of tumor necrosis factor α on ability of SHED to promote osteoclastogenesis during physiological root resorption. Biomed Pharmacother. 2019;114:108803. doi: 10.1016/j.biopha.2019.108803
- Al-Sehaibany FS, Alomran W, Almutairi A, Al-Homaidhi MA, Aldosari MA, Albarakati SF. Patterns of Root Resorption in Primary Mandibular Molars of Saudi Children. Biosc Biotech Res Comm. 2020;13(4): 1967-1971. doi: 10.21786/bbrc/13.4/50
- Sharma A, Kulkarani S, Swamy N, Khandelwal V, Nenava D, Agrawal P. Co-Relation between root resorption patterns of deciduous mandibular molars and position of erupting permanent successors: A radiographic evaluation. Int J Appl Res. 2016; 2(5): 440-444.
- Vieira-Andrade RG, Drumond CL, Araújo MS, Santos GS, Fonseca-Silva T, Ramos-Jorge ML Asymmetrical root resorption in primary mandibular molars: Prevalence and determinants factors. Int Dent Med J Adv Res. 2016;2:1-5. doi: 10.15713/ins.idmjar.40
- de Lima EM, Schmidt CB, de Araujo LL, Rizzatto SM, Martinelli FL. How to predict the timing of eruption of mandibular second premolars. Angle Orthod. 2012;82(6):1067-1070. doi: 10.2319/092111-600.1
- Rodrigues LV, Del Puerto HL, Brant JM, Leite RC, Vasconcelos AC. Caspase‐3/caspase‐8, bax and bcl2 in pulps of human primary teeth with physiological root resorption. Int J Paediatr Dent. 2012;22(1):52-59. doi: 10.1111/j.1365-263X.2011.01157.x
- Moorrees CF, Fanning EA, Hunt Jr EE. Formation and resorption of three deciduous teeth in children. Am J Phys Anthropol. 1963;21(2):205-213. doi: 10.1002/ajpa.1330210212
- Fulton AJ, Liversidge HM. A radiographic study of estimating age by deciduous mandibular canine and molar root resorption. Ann Anat. 2016;203:33-37. doi: 10.1016/j.aanat.2015.02.010
- Sahara N. Cellular events at the onset of physiological root resorption in rabbit deciduous teeth. Anat Rec. 2001;264(4):387-396. doi: 10.1002/ar.10017
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
