By Hafsa Saeed, Fatima Jehangir, Misbah Mohammad, Aliya Mazhar
AFFLIATIONS:
Family Medicine Clinic, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-3/006
ORCID iD: 0000-0002-6094-4738
How to cite: Saeed H, Jehangir F, Mohammad M, Mazhar A. Hypertension and Its Predictors in a Squatter Settlement of Karachi. Pak J Med Dent. 2022;11(3): 30-36. doi: 10.36283/PJMD11-3/006
Background: Hypertension, the ‘silent killer’, is the cause of high mortality and is one of the major health problems worldwide. This study aimed to determine the frequency of hypertension and its predictors in a squatter settlement in Karachi.
Methods: A cross-sectional study (n=212) was conducted at the Family Medicine Clinic, Karachi. The participants aged 18 to 65 years, from Jan 1st to 30th June 2020 were recruited. Thorough examination (including blood pressure, weight, and height) and interviews of the participants were done regarding lifestyle, cardiovascular risk factors, personal and family history of cardiovascular diseases, or other chronic illnesses. The Chi-square test was used to identify the association of the risk factors with hypertension and a p-value <0.05 was considered statistically significant.
Results: The overall burden of hypertension calculated was 63(29.7%). The mean age of participants was 39.3+15.4 years. A very strong association (p<0.01) of hypertension (76.5%) was seen with a history of dyslipidemia compared to non-hypertensives (23.5%). Among diabetics, it was found that 84% were hypertensive and 16% were non-hypertensive with a statistically significant (p =0.00) association. Personal history of ischemic heart disease (77.8%, p-value 0.003), transient ischemic attack (TIA)/stroke (100%, p-value 0.087) and family history of premature coronary artery diseases (88.9%, p-value <0.01) were seen more common in individuals with high blood pressure.
Conclusion: The frequency of hypertension is high in a squatter settlement in Karachi and it is highly associated (p<0.01) with the development of dyslipidemia, diabetes, family history of coronary artery and cerebrovascular diseases respectively.
Keywords: Hypertension; Dyslipidemia; Coronary Artery Disease; Cerebrovascular Disorders.
Hypertension, commonly referred to as High Blood Pressure is characterized by chronic damage to the blood vessels leading to formidable consequences such as coronary artery disease, heart failure, cerebrovascular disease, and chronic kidney disease1. Often quoted as the ‘silent killer’ because of its high mortality and lack of early warning signs, it is a major cause of premature deaths worldwide2. The burden of hypertension is rising in both developed and developing countries making it a major factor in mortality and morbidity around the world. According to an estimate, one-quarter of the world’s population above 18 years of age has hypertension and this figure is expected to increase to 29% by 2025 3.
Pakistan like other developing countries is changing its diet and lifestyle pattern. Due to this change, hypertension is emerging as a significant public health problem. The health and economic systems of Pakistan, which is a low-income country, seem to be unprepared to face this challenge. Prevention and early detection, and adequate management of hypertension will reduce the risk of stroke, myocardial infarction, chronic kidney diseases and heart failure, and will consequently reduce the burden on Pakistan’s health care system. Some studies have been done previously to estimate the prevalence of hypertension in the squatter of Karachi1-3. Nevertheless, these published data had become old, therefore revised data is needed. Therefore, this study aimed to determine the prevalence of hypertension and its risk factors in a squatter settlement in Karachi.
A cross-sectional study, approved under ERC Reference code: 2340720FJFM, was done by recruiting all patients aged 18 or more to come to a primary health care center from Jan 1 2020 to 30 June 2020. The estimated sample size according to openepi.com sample size calculator for cross-sectional studies was 227 taking 95% as the confidence interval with an estimated population of 100,000 in Sikandarabad using 18% prevalence from the previous study4. The current study recruited 212 participants. The exclusion criteria were as follows: pregnant and lactating women and those who had any immuno-compromising condition e.g., cancer and HIV. After taking written consent, contact details including name and contact number were taken by each participant to ensure duplication was avoided.
All the vitals such as blood pressure (standing and sitting position), heart rate (resting and after 5 minutes of exercise), respiratory rate, height, weight and BMI were checked. Anemia, cyanosis, jugular venous pressure, palpable thyroid gland and pedal edema were documented. Systemic examinations including heart sounds and basal crepitations were assessed. A family physician assessed the comorbidity and lifestyle factors such as consumption of salt, fruits, vegetables and dairy products. The level of physical activity was estimated at 150 minutes a week of a brisk walk. Age, sex, marital status, education, work history, smoking, alcohol intake, personal, and family history of hypertension, diabetes, premature cardiovascular deaths and stroke was also noted.
For the classification of hypertension, the standard classification of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7 was used. Hypertension was defined as a systolic BP level of ≥140 mmHg and/or diastolic BP level of ≥90 mmHg or being previously diagnosed as hypertensive by any health professional. The area falling between 120–139 mmHg systolic BP and 80–89 mmHg diastolic BP is defined as “pre-hypertension”5. Current daily smokers are defined as those who were currently smoking cigarettes, bidis, or hookah daily. Those who take > 5 units of alcohol per day were labeled as Alcoholics. WHO International BMI classification: BMI <18.5 was classified as “underweight”; 18.50–24.99, “normal range”; “overweight”; 25.0–29.99, “obese”; >30.006. Physical activity was measured in terms of an active lifestyle for those who do 150 min/week walk (CDC) and sedentary for those who did <150 min/week walk.
The SPSS version 20 was used for analyzing the data. Mean and standard deviation was calculated for numerical variables and frequency and percentage for categorical variables. Chi-square was used to identify the association of variables with the outcome. A p-value <0.05 was considered to show a significant association.
Among 212 individuals, the prevalence of hypertension was 63 (29.7%). The mean age of participants was 39.3+15.4 years. Most of the subjects were overweight with a mean BMI of 25.3+6.1kg/m2. Males who were employed were 38(48.1%), the rest being jobless, whereas females who were employed were 41 (51.9%).
Of those who were hypertensive, 44% were employed with statistically significant results (p-value 0.001). A sedentary lifestyle was observed by 187 (88.2%) while 25(11.8%) had an active lifestyle. Of those who were hypertensive, the majority (30.3%) had a sedentary lifestyle as compared to 28% of subjects who had an active lifestyle but the results were statistically insignificant p=0.78. DASH diet was consumed by 38(17.9%) individuals (Table 1). The hypertensive 26.3% took the DASH diet demonstrating that hypertension was not common in subjects who took the DASH diet but the results were statistically insignificant (p-value 0.38). Male smokers were 20 (25.3%) whereas there was no female smoker in the study. Of the participants having high blood pressure, 25% were smokers showing smoking had no impact on high blood pressure in this study but the results were statistically insignificant p=0.421. Among hypertensive, none consumed alcohol in this study (p-value 0.49) when co-morbid were identified along with HTN, 11.8% (25) were diabetic, 16% (34) had hyperlipidemia, 4.2% (9) and 0.9% (2) had a history of ischemic heart disease and TIA/stroke respectively (Table 1). When family history was evaluated 7.6% (16) and 4.2% (9) had a history of premature coronary artery disease and stroke respectively. Those who were hypertensive, 77.8%, 100% and 88.9% had a history of ischemic heart disease (p-value 0.003), TIA/stroke (p-value 0.087) and family history of premature CAD (p-value <0.001) respectively, all having statistically significant results showing association of hypertension with CAD and CVD.
Table 1: Comparison of hypertension with associated risk factors.
| Characteristics | Frequency (n)
Percentage (%) |
Hypertensives n=63 (%) | Non-Hypertensives
n=149 (%) |
p-Value | |
| Gender | Female | 79(37.3) | 27.8 | 72.2 | 0.38 |
| Male | 133(62.7) | 30.8 | 69.2 | ||
| Employment status | |||||
| Jobless
Employed |
75(35.4)
137(64.6) |
44
21.9 |
56
78.1 |
0.001 | |
| Marital status | |||||
| Married
Single |
178(84)
34 (16) |
32.6
14.7 |
67.4
85.3 |
0.025 | |
| Level of education | |||||
| Matric
Intermediate University |
144(67.9)
17(8) 3(1.4) |
29.2
41.2 0 |
70.8
58.8 100 |
0.31 | |
| Lifestyle | |||||
| Sedentary
Active |
187(88.2)
25 (11.8) |
30.3
28 |
69.7
72 |
0.78 | |
| Smoking status | |||||
| Smokers
Non-smokers |
20(9.4)
192(90.6) |
25
30.2 |
75
69.8 |
0.42 | |
| Alcohol intake | |||||
| Yes
No |
2(0.9)
210 (99.1) |
0
30 |
100
70 |
0.49
|
|
| History of Diabetes Mellitus (DM) | |||||
| Present
Absent |
25(11.8)
187(88.2) |
84
22.5 |
16
77.5 |
<0.01 | |
| History of hyperlipidemia | |||||
| Present
Absent |
34(16)
178(18) |
76.5
20.8 |
23.5
79.2 |
<0.01 | |
| History of Ischemic Heart Disease (IHD) | |||||
| Present
Absent |
9(4.2)
203 (95.8) |
77.8
27.6 |
22.2
72.4 |
0.003 | |
| History of Transient Ischemic Attack (TIA)/Stroke | |||||
| Present
Absent |
2(0.9)
210(99.1) |
100
29 |
0
71 |
0.087 | |
| Dietary Approaches to Stop Hypertension (DASH) diet | |||||
| Users
Non-users |
38(17.9)
174 (82.1) |
26.3
30.5 |
73.7
69.5 |
0.38 | |
| Family history of premature Coronary Artery Disease (CAD) | |||||
| Present
Absent |
16(7.6)
196 (92.5) |
88.9
27.1 |
11.1
72.9 |
<0.001 | |
| Family history of stroke | |||||
| Present
Absent |
9(4.2)
203(95.8) |
37.5
29.1 |
62.5
70.9 |
0.33 | |
| Indulgence in recreational activities | |||||
| Rarely
Sometimes Often |
90(42.5)
30(14.2) 92(43.4) |
96.8
3.2 0 |
19.5
18.8 61.7 |
<0.001 |
|
| Commuting mode | |||||
| Walking and Cycling
Motorized vehicle |
75(35.4)
137(64.6) |
4.8
95.2 |
48.3
51.7 |
<0.001 |
|
Figure 1 shows that among hypertensive, the majority (76.5%) had hyperlipidemia with statistically significant results (p-value <0.01). Figure 2 represents that 88.9% of hypertensive had a family history of premature coronary artery disease, again with statistically significant results (p-value<0.01)
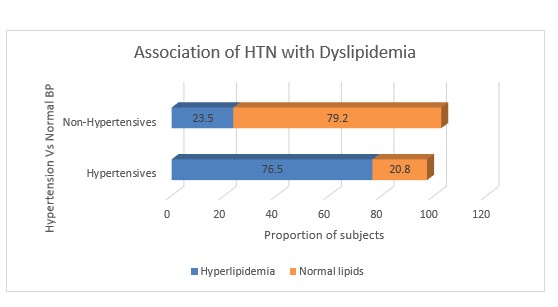
Figure 1: Association of deranged lipids with high blood pressure.
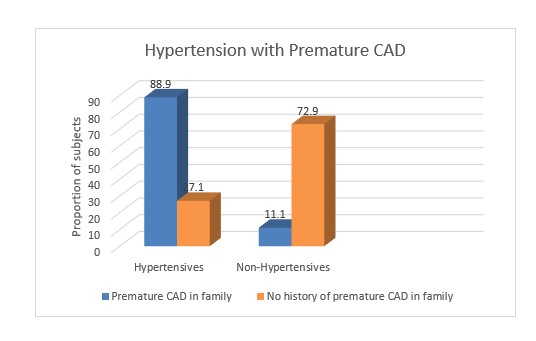
Figure 2: Association of family history of premature coronary artery (CAD) disease with hypertension.
Pakistan is undergoing a shift in diet and lifestyle patterns. Due to this epidemiologic and nutritional transition, hypertension is emerging as one of the significant public health concerns. National sampling study from 1990 to 1994 reported the prevalence of hypertension in adults aged more than 15 years to be 19.75% which surged up to 46.2% as indicated in the Second National Diabetes Survey Report of Pakistan (NDSP) 2016–2017 7. Pakistan is ranked as the third country in the South Asian Association for Regional Cooperation for its high prevalence of hypertension8. In line with the trend at the national level mentioned above, this study showed a high prevalence of hypertension of about 29.7%with 37.3% of male subjects and 62.7% of females. This is very high as compared to the 15% rate which was reported in Siddiqui et al study in 2005, conducted in the same slums squatter settlement in Karachi9. This study correlates to the study conducted in another squatter settlement of Karachi by Safdar et al who found a prevalence rate of 26%, with 34% in males and 24% in females and Ishtiaq et al. also found a prevalence rate of 29.2% in twin cities of Pakistan (i.e., Rawalpindi-Islamabad) 10,11.
This significant rise is alarming, particularly in a developing country like Pakistan, where the health infrastructure is not yet at an optimal level; and requires serious and focused efforts to control the rate of hypertension in Pakistan. Although many studies have been done in Pakistan in the past to estimate the prevalence of hypertension at the national level, little is known about the burden and risk factors of hypertension in the slum population, which makes up one-third of the urban population in Pakistan. Lack of data regarding health issues from these communities can cause improper and unrealistic allocation of health care resources by the private and government sector. In the current study, investigators estimated the prevalence of hypertension and its risk factors in a selected population living in the slums of Karachi.
For the gender association, most of the studies showed a higher prevalence of hypertension in men as compared to women12. Whereas some studies indicated that the female gender is a risk factor in the development of hypertension and women are more prone to be hypertensive. For instance, a report from American Heart Association also observed that in the American population, women are more prone to develop hypertension than men13. This increased frequency of hypertension in females could be because of their high BMI and more sedentary lifestyle and lack of exercise or because females get more medical checkups during their pregnancy.
Many studies had shown a positive relationship between advancing age with hypertension. Increasing age led to a stiffening of the aorta and arterial wall which causes a higher prevalence of hypertension in the older population group. Contrary to these, this study did not show a positive relationship between advancing age and hypertension14,15.
The current study reported that 31% of individuals have a family history of coronary artery disease. The study also demonstrated a significant association between a family history of coronary artery disease with hypertension. Research studies from different countries have also shown a strong association between a family history of coronary artery disease and hypertension or blood pressure level16,17. Those with a positive family history of coronary artery disease were more likely to have hypertension in comparison to those with a negative family history of coronary artery disease. Thus, these people need strict positive changes in behavior and lifestyle. It is to be expected that it should lead to significant mitigation of risk over the long term.
Dyslipidemia, a strong predictor of cardiovascular disease, causes endothelial damage, and the loss of physiological vasomotor activity that becomes manifested as increased blood pressure (BP). In line with the previous studies that have reported a positive relation between dyslipidemia and hypertension18,19. The current study also gives important evidence that dyslipidemia is a strong risk factor in the development of hypertension in the Pakistani population. High intake of meat, ghee and butter in traditional Pakistani food and fewer intakes of fruits and vegetables with a sedentary lifestyle is responsible for dyslipidemia, once thought to be a disease in high-income countries and a rise in hypertension.
Diabetes significantly increases the odds of developing hypertension. Many studies demonstrated diabetes mellitus and hypertension are inter-linked and that can pose a risk of atherosclerotic cardiovascular disease in an individual. Compared to non-diabetics, hypertension is more likely to prevail in diabetics. Tsimihodimos et al. found that diabetes mellitus was an independent risk factor in the development of hypertension, irrespective of gender, age, body mass index, and familial diabetes mellitus. It further noted that hypertension was also an independent risk factor for diabetes mellitus20. Similarly, in another survey, Tatsumi et al. found approximately one-half of diabetic patients had hypertension, and approximately one-fifth of hypertensive patients had diabetes mellitus. Those with either of these two morbidity factors (i.e., hypertension or diabetes mellitus) had a 1.5 to 2.0 times likelihood of having both conditions21. This study also confirmed this association. “Over time, diabetes damages the small blood vessels in the body, causing the walls of the blood vessels to stiffen. This increases pressure, which leads to high blood pressure”.
Convenient means of transportation and the advancements in the internet led to more people spending a sedentary life22. Also increase in obesity due to higher consumption of fatty foods, which are no longer confined to high-income countries, has led to a higher burden of chronic diseases. Previous research noted a moderate physical activity every day was an important non-pharmacological treatment to lower the risk of hypertension and diabetes. In line with these studies, the present study found as the level of recreation increases, the prevalence of hypertension decreases; thus, showing an inverse relationship between recreation and hypertension. This study gives evidence that higher levels of physical activity in adulthood can partially offset the increased risks of hypertension23,24.
Other studies suggested that hypertension is more common in alcohol users and smokers25-27. Thus, alcohol consumption and tobacco use are considered a strong risk factor for the development of hypertension. In this study, of those who had hypertension only 25% were smokers showing smoking and alcohol had no impact on high blood pressure, so the study did not find a significant relationship between alcohol and tobacco use and hypertension. The analysis identified a strong relationship between personal history of ischemic heart disease and TIA with that hypertension that was similar to previous studies28,29. Likewise, Cipolla et al. reported that hypertension is a prominent determinant in the stroke population30. It causes increased shear stress, endothelial dysfunction, and large artery stiffness to the cerebral microcirculation. And this is a significant risk factor in the development of stroke. Effective measures should be taken to control hypertension which will reduce the risk of stroke.
It would be pertinent to mention certain limitations in this study. As this study was conducted in a selected slum area in Karachi, it might not be representative of the entire slum population of Pakistan. In the study, only a few participants have disclosed alcohol and tobacco intake; which might be under-representation owing to the religious and cultural environment and fear of shame.
Immediate measures such as awareness, early detection of hypertension, and adequate treatment and good control of dyslipidemia and diabetes are required through organized health education programs for the prevention and control of hypertension and its risk factors among the general mass.
The prevalence of hypertension (29.7%) in the slums of Karachi was quite high. The disease has strong associations with determinants such as hyperlipidemia, diabetes and a family history of premature coronary artery disease that adds to morbidities like ischemic heart disease and cerebrovascular diseases. Therefore, immediate and effective measures to increase awareness, early detection and control of hypertension, diabetes and hyperlipidemia should be taken through effective community programs at the individual as well as national level.
The authors are thanking all consultant family physicians and staff of the Family Medicine Health Care Center for cooperating in examining the subjects enrolled in the study.
There was no conflict of interest among the authors.
The study had been approved by ethics review committee with the reference code: 2340720FJFM.
Informed consent was taken from all the participants of the study.
HS was involved in the conception, designing, bench work and writing the manuscript. FJ was involved in writing the paper, and proofreading and supervising the project. AM and MM helped in data collection.
- D’Agostino Sr RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117(6):743-753. doi: 10.1161/CIRCULATIONAHA.107.699579
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224-2260. doi: 10.1016/S0140-6736(12)61766-8
- Sarafidis PA, Li S, Chen SC, Collins AJ, Brown WW, Klag MJ, et al. Hypertension awareness, treatment, and control in chronic kidney disease. Am J Med. 2008;121(4):332-340. doi: 10.1016/j.amjmed.2007.11.025
- Basit A, Tanveer S, Fawwad A, Naeem N, NDSP Members. Prevalence and contributing risk factors for hypertension in urban and rural areas of Pakistan; a study from second National Diabetes Survey of Pakistan (NDSP) 2016–2017. Clin Exp Hypertens. 2020;42(3):218-224. doi: 10.1080/10641963.2019.1619753
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2571. doi:10.1001/jama.289.19.2560
- Hypertension Pakistan 2020 country profile [Internet]. World Health Organization 2022. Available from: https://cdn.who.int/media/docs/default-source/country-profiles/hypertension/pak_en.pdf?sfvrsn=79fa29fd_9&download=true Pakistan medical
- Research Council, Pakistan National Health Survey.1990-1994. Pakistan Medical Research Council publication. Available from: https://ghdx.healthdata.org/record/pakistan-national-health-survey-1990-1994
- Neupane D, McLachlan CS, Sharma R, Gyawali B, Khanal V, Mishra SR, et al. Prevalence of hypertension in member countries of South Asian Association for Regional Cooperation (SAARC): systematic review and meta-analysis. Medicine (Baltimore). 2014; 93(13):1-10. doi: 10.1097/MD.0000000000000074
- Siddiqui H, Anjum Q, Omair A, Usman J, Rizvi R, Ashfaq T. Risk factors assessment for hypertension in a squatter settlement of Karachi. J Pak Med Assoc. 2005;55(9):390-392.
- Safdar S, Omair A, Faisal U, Hasan H. Prevalence of hypertension in a low income settlement of Karachi, Pakistan. J Pak Med Assoc. 2004; 54(10):506-509.
- Ishtiaq S, Ilyas U, Naz S, Altaf R, Afzaal H, Muhammad SA, et al. Assessment of the risk factors of hypertension among adult & elderly group in twin cities of Pakistan. J Pak Med Assoc. 2017;67(11):1664-1669.
- Song JJ, Ma Z, Wang J, Chen LX, Zhong JC. Gender differences in hypertension. J Cardiovasc Trans Res. 2020;13(1):47-54. doi: 10.1007/s12265-019-09888-z
- Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135(10):146-603. doi: 10.1161/CIR.0000000000000485
- Shukuri A, Tewelde T, Shaweno T. Prevalence of old age hypertension and associated factors among older adults in rural Ethiopia. Integr Blood Press Control. 2019; 12: 23-31. doi: 10.2147/IBPC.S212821
- Hu L, Huang X, You C, Li J, Hong K, Li P, et al. Prevalence and risk factors of prehypertension and hypertension in Southern China. PLoS One. 2017;12(1):1-15. doi: 10.1371/journal.pone.0170238
- Bushnik T, Hennessy DA, McAlister FA, Manuel DG. Factors associated with hypertension control among older Canadians. Health Rep. 2018;29(6):3-10.
- Valerio L, Peters RJ, Zwinderman AH, Pinto‐Sietsma SJ. Association of family history with cardiovascular disease in hypertensive individuals in a multiethnic population. J Am Heart Assoc. 2016;5(12):1-9. doi: 10.1161/JAHA.116.004260
- Ariyanti R, Besral B. Dyslipidemia associated with hypertension increases the risks for coronary heart disease: a case-control study in Harapan Kita Hospital, National Cardiovascular Center, Jakarta. J Lipids. 2019;2019:1-6. doi: 10.1155/2019/2517013
- Ayoade OG, Umoh I, Amadi C. Dyslipidemia and associated risk factors among nigerians with hypertension. Dubai Med J. 2020;3(44):155-161. doi: 10.1159/000509570
- Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus: coprediction and time trajectories. Hypertension. 2018;71(3):422-428. doi: 10.1161/HYPERTENSIONAHA.117.10546
- Tatsumi Y, Ohkubo T. Hypertension with diabetes mellitus: significance from an epidemiological perspective for Japanese. Hypertens Res. 2017;40(9):795-806. doi: 10.1038/hr.2017.67
- Lee JY, Ryu S, Sung KC. Association of baseline level of physical activity and its temporal changes with incident hypertension and diabetes mellitus. Eur J Prev Cardiol. 2018;25(10):1065-1073. doi: 10.1177/2047487318774419
- Ryu S, Frith E, Pedisic Z, Kang M, Loprinzi PD. Secular trends in the association between obesity and hypertension among adults in the United States, 1999–2014. Eur J Intern Med. 2019;62:37-42. doi: 10.1016/j.ejim.2019.02.012
- Shariq OA, McKenzie TJ. Obesity-related hypertension: a review of pathophysiology, management, and the role of metabolic surgery. Gland Surg. 2020; 9(1): 80-93. doi: 10.21037/gs.2019.12.03
- Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in urban Varanasi. Int J Hypertens. 2017;2017:1-10. doi: 10.1155/2017/5491838
- Noubiap JJ, Nansseu JR, Endomba FT, Ngouo A, Nkeck JR, Nyaga UF, et al. Active smoking among people with diabetes mellitus or hypertension in Africa: a systematic review and meta-analysis. Sci Rep. 2019;9(1):1-11. doi: 10.1038/s41598-018-37858-z
- Tumwesigye NM, Mutungi G, Bahendeka S, Wesonga R, Katureebe A, Biribawa C, et al. Alcohol consumption, hypertension and obesity: Relationship patterns along different age groups in Uganda. Prev Med Rep. 2020;19:1-8. doi: 10.1016/j.pmedr.2020.101141
- Wajngarten M, Silva GS. Hypertension and stroke: update on treatment. Eur Cardiol. 2019; 14(2): 111-115. doi: 10.15420/ecr.2019.11.1
- O’Donnell M, Hankey GJ, Rangarajan S, Chin SL, Rao-Melacini P, Ferguson J, et al. Variations in knowledge, awareness and treatment of hypertension and stroke risk by country income level. Heart. 2021;107(4):282-289. doi: 10.1136/heartjnl-2019-316515
- Cipolla MJ, Liebeskind DS, Chan SL. The importance of comorbidities in ischemic stroke: Impact of hypertension on the cerebral circulation. J Cereb Blood Flow Metab. 2018;38(12):2129-2149. doi: 10.1177/0271678X18800589
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
