By Mazhar Shafiq1, Akhter2, Lubna Shamshad3, Nisar Ahmed4, Sadaf Saleem5, Rahat Shahid6, Shumaila7, Muhammad Ali Mazhar8
AFFLIATIONS:
- Department of Radiology, Combined Military Hospital (CMH) Kohat Cantt, Pakistan.
- Department of Radiology, Combined Military Hospital (CMH), Abbottabad, Pakistan.
- Department of Radiology, Indus hospital Karachi, Pakistan.
- Armed Forces Institute of Radiology and Imaging (AFIRI), Rawalpindi, Pakistan.
- Department of Biochemistry, Shalamar Medical and Dental College, Lahore, Pakistan.
- PNS Hospital Hafiz Islamabad, Pakistan.
- PNS Hospital Shifa, Karachi, Pakistan.
- Student, Central Park Medical College, Lahore, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-3/003
How to cite: Shafiq M, Shamshad L, Ahmed N, Saleem S, Shahid R, Mazhar MA, et al. Diagnostic Accuracy of Mammography Versus Ultrasound in Prediction of Malignancy with Palpable Breast Lesion. Pak J Med Dent. 2022;11(3): 11-16. doi: 10.36283/PJMD11-3/003
Background: Breast malignancy is globally the most prevalent type of cancer. Early and appropriate screening is important for proper treatment. Ultrasonography (USG) is extensively useful as an adjunct to mammography in clinical practice. This study aimed to compare the diagnostic accurateness of mammography versus ultrasound imaging in predicting breast malignancies in women with palpable lesions using histopathology as the gold standard.
Methods: The bilateral mammography was performed on 100 patients of age 35-80 years in the Radiology department, PNS Shifa hospital, Karachi. Bilateral whole-breast USG was also performed and findings were recorded. Then histopathology was done by taking samples (localized solid swelling fixed to breast tissue and skin feeling different from normal breast parenchyma, present more than 1 month) through TruCut 18 G needle and compared with mammography and ultrasound. The data was analyzed by SPSS and a screening test was applied to check the sensitivity and specificity.
Results: The mean age of the patients (n=100) was 58.91±13.46 years. The USG diagnosed malignant breast lesions in 46% and benign breast lesions in 54% of patients. Whereas, by mammography, malignancy was diagnosed in 47% and benign in 53% of patients. The USG tool showed 69.64% sensitivity, 84.09% specificity, 84.78% negative predictive value (NPV), 68.52% positive predictive value (PPV) and 76% diagnostic accuracy, respectively. However, mammography had 60.71% sensitivity, 70.45% specificity, 72.34% NPV, 58.49% PPV and 65% accuracy, while considering histopathology as the gold standard.
Conclusion: The ultrasonography (USG) was found more sensitive than mammography in the prediction of breast malignancy presenting with palpable breast lesions.
Keywords: Mammography; Ultrasonography; Accuracy; Histopathology; Breast Cancer.
Breast malignancy is the predominant cancer of females globally with around one million new cases reported every year and is likewise the primary cause of female death after cardiovascular disease. In Pakistan, the incidence of breast cancer in comparison to other Asian nations like India and Iran is 2.5 times higher1. Therefore, a palpable breast abnormality should be further investigated2.
Women often report to the imaging department with palpable breast abnormalities. However, the most suitable sequence and degree of imaging required are still not clear3. Breast cancers with palpable lesions are common among women not undertaking mammography annually4. A mammogram is a screening program, which is very helpful and effective in the detection of the disease5. It is a key screening tool for early detection of breast malignancy even before it becomes palpable on self-examination of the breast6. Breast density is related to a four to six times increase in the chance of breast cancer development in women7. Mammographic breast density has been perceived by investigators as a novel and independent risk factor for malignant breast disease7, 8.
In the clinical setting breast USG has become a convenient and widely available adjunct to mammography. It is frequently used to assist in the clinical evaluation of suspicious breast lesions found on mammograms or physical examinations. There are quite a few factors that limit the use of USG as a screening tool, for example, its failure to detect micro calcifications and its less specificity (34%) 9. However, USG has now become a well-established imaging technique in breast cancer detection and provides useful information about the nature and magnitude of all types of breast lesions and can often provide valuable info regarding axilla staging10. USG-guided biopsies and therapeutic procedures are now routinely done, and modern research is more focusing on evaluating its role in screening breast and other cancers10.
Mammography and ultrasound of the breast are now universally used diagnostic imaging methods for the estimation of the primary tumor size at diagnosis time11. The rationale of the study was to compare the diagnostic precision of mammography versus ultrasound imaging in the prediction of malignancy of breast in women presenting with palpable breast lesions. Mammography is highly efficient in detecting the type of breast lumps. But the literature above showed that ultrasound is more accurate in detecting breast malignancy as compared to mammography. Ultrasound is a cheap and readily available tool for early detection of breast malignancy while mammography requires expertise and is comparatively very expensive. Subsequently, this study will confirm the most suitable and efficient method and may be implemented in the future in a local setting.
Therefore, this study aimed to compare the diagnostic precision of mammography versus USG imaging in the prediction of malignancy of breast in females presenting with palpable breast lesions taking histopathology as a gold standard.
It was a descriptive cross-sectional study done at the Radiology department, PNS Shifa hospital, Karachi. The total study duration was six months after synopsis approval. The sample size was determined to be 100 patients (confidence level 95%) and taking an estimated percentage of breast malignancy i.e., 25% in females, the sensitivity of mammography i.e., 80.47% with a 16% error margin, and specificity of mammography i.e., 73.07% with 10.5% error margin in patients presenting with palpable breast lumps.
Non-probability convenient sampling technique was used. Proforma was used to record all the information. The inclusion criteria were age between 35-80 years presenting with breast lumps (localized solid swelling fixed to breast tissue and skin feeling different from normal breast parenchyma) for >1 month and planned to undergo biopsy by using TruCut core biopsy. Unmarried females, already diagnosed with cases of breast cancer and females with recurrence of malignancy in the same site and taking chemotherapy or radiotherapy on the same side (on medical record) were not included in the study.
The patients were referred to Radiology Department, PNS Shifa Hospital, Karachi and satisfying the selection criteria were considered for the study. Demographic detail including name, age, parity, and history of breastfeeding was noted after taking informed consent. The mammography was performed and included standard bilateral craniocaudal and mediolateral oblique views. The spot or global-magnification views were taken for microcalcification detection over the malignant growth. Results were documented using the Breast Imaging Reporting and Data System (BI-RAD)9.
The core-needle USG was performed bilaterally for the whole breast with prior information of clinical and mammographic findings by a radiologist or senior fellow having 6 months to 4 years of experience in breast USG execution and interpretation. The USG guided core needle biopsy was carried out preoperatively by single senior radiologists having 4 years of experience. Images were obtained and discussed with the supervisor. Then histopathology was done by taking samples through a TruCut needle and sent to the hospital histopathology department. Reports were assessed and compared with results of mammography and ultrasound. SPSS version 20.0 was utilized to enter and analyze the data. The screening test was applied to check the sensitivity and specificity of the tool.
In this study histopathology diagnosed malignant breast lesions among 56(56%) patients and benign breast lesions among 44(44%) (Figure 1).
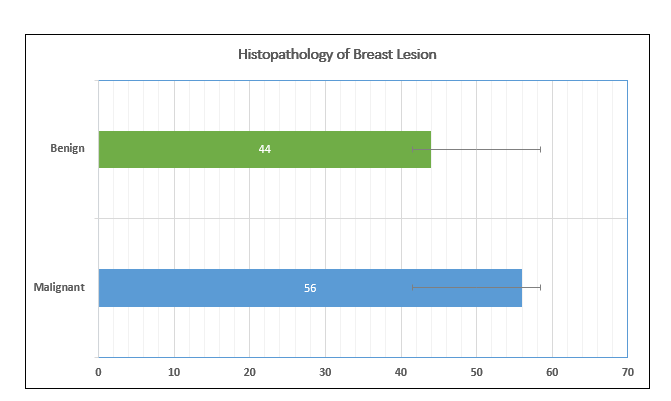
Figure 1: Histopathological results of female patients presenting with breast lesions.
The mean age of the 100 patients was 58.91±13.46 years with minimum and maximum ages of 35 and 80 years respectively. The mean value of disease time duration of the patients was 2.88±1.31 months with a minimum and maximum of 1 and 5 months respectively (Table 1).
Table 1: Diagnostic accuracy of mammography and ultrasound in the prediction of malignancy in women with palpable breast lesions.
| Variables | Mean± SD | Minimum | Maximum | |||||
| Age (years) | 58.91±13.46 | 35 | 80 | |||||
| Time duration (months) | 2.88±1.31 | 1 | 5 | |||||
| With histopathology | Sensitivity | Specificity | Positive Predicted Value | Negative Predicted Value | Diagnostic Accuracy | |||
| Ultrasonography (USG) | 69.64% | 84.09% | 84.78% | 68.52% | 76% | |||
| Mammography | 60.71% | 70.45% | 72.34% | 58.49% | 65% | |||
| USG breast lesion with histopathology | ||||||||
| Malignant 46(46.0) | 69.64% | 84.09% | 84.78% | 68.52% | 76% | |||
| Benign 54(54.0) | ||||||||
| Comparison of mammography with histopathology | ||||||||
| Malignant 47(47.0) | 60.71% | 70.45% | 72.34% | 58.49% | 65% | |||
| Benign 53(53.0) | ||||||||
| Comparison of USG lesion with histopathology stratified by anatomical site | ||||||||
| Right | Malignant | 75.76% | 94.44% | 96.15% | 68% | 82.35% | ||
| Benign | ||||||||
| Left | Malignant | 60.87% | 76.92% | 70% | 68.97% | 69.39% | ||
| Benign | ||||||||
| Comparison of mammography lesion with histopathology stratified by anatomical site | ||||||||
| Right | Malignant | 83.33% | 60% | 71.43% | 75% | 72.73% | ||
| Benign | ||||||||
| Left | Malignant | 58% | 71.79% | 72.5% | 57.14% | 64.04% | ||
| Benign | ||||||||
Out of the total, 89(89%) patients were with a positive history of breastfeeding and 11(11%) patients were with negative history of breastfeeding. The USG diagnosed malignant breast lesion was present among 46(46%) patients and benign breast lesion among 54(54%) patients. In this study, the mammography diagnosed malignant breast lesions was among 47(47%) patients and benign breast lesions among 53(53%) patients. The sensitivity, specificity, NPV, PPV and diagnostic accuracy of USG breast lesion was 69.64%, 84.09%, 84.78%, 68.52% and 76% respectively taking histopathology as the gold standard. While the sensitivity, specificity, NPV, PPV and diagnostic accuracy of mammography breast lesion was 60.71%, 70.45%, 72.34%, 58.49% and 65% respectively taking histopathology as the gold standard.
The study results showed that in ≤ 50 years patients, the sensitivity, specificity and diagnostic accuracy of USG lesion was 75%, 81.82% % and 77.42% respectively. In patients with time duration ≤ 3 months, the sensitivity, specificity and diagnostic accuracy of USG lesion was 69.44%, 80.65% 74.63%, respectively, similarly in patients with time duration >3 months, the sensitivity, specificity and diagnostic accuracy of USG lesion was 70%, 93.31% 78.79%, respectively taking histopathology as a gold standard (Table 2).
Table 2: Diagnostic accuracy of mammography and ultrasound concerning age and time duration.
| Variables | Sensitivity | Specificity | Positive Predicted Value | Negative Predicted Value | Diagnostic Accuracy | ||||||
| Comparison of Ultrasonography (USG) lesion with histopathology stratified by age | |||||||||||
| Age ≤ 50 | Malignant | 75% | 81.82% | 88.24% | 64.29% | 77.42% | |||||
| Benign | |||||||||||
| > 50 | Malignant | 66.67% | 84.85% | 82.76% | 70% | 75.36% | |||||
| Benign | |||||||||||
| Comparison of mammography lesion with histopathology stratified by age | |||||||||||
| Age ≤ 50 | Malignant | 70% | 72.73% | 82.35% | 57.14% | 70.97% | |||||
| Benign | |||||||||||
| > 50 | Malignant | 55.56% | 69.7% | 66.67% | 58.97% | 62.32% | |||||
| Benign | |||||||||||
| Comparison of USG lesion with histopathology stratified by time duration | |||||||||||
| Time Duration ≤ 3 | Malignant | 69.44% | 80.65% | 80.65% | 69.44% | 74.63% | |||||
| Benign | |||||||||||
| > 3 | Malignant | 70% | 93.31% | 93.33% | 66.67% | 78.79% | |||||
| Benign | |||||||||||
| Comparison of mammography lesion with histopathology stratified by time duration | |||||||||||
| Time Duration ≤ 3 | Malignant | 63.89% | 70.97% | 71.88% | 62.86% | 67.16% | |||||
| Benign | |||||||||||
| > 3 | Malignant | 55% | 69.23% | 73.33% | 50.00% | 60.61% | |||||
| Benign | |||||||||||
This cross-sectional study was done to compare the diagnostic accuracy of mammography versus USG imaging in the prediction of malignancy in females presenting with palpable breast lesions taking histopathology as the gold standard. In this study the sensitivity, specificity, and diagnostic accuracy of USG were 69.64%, 84.09% and 76%, respectively taking histopathology as a gold standard. Whereas, the sensitivity, specificity and diagnostic accuracy of mammography were 60.71%, 70.45% and 65%, respectively, highlighting that USG is more accurate than mammography in breast malignancy prediction.
A study by Keune et al. showed that following neoadjuvant chemotherapy, breast USG was more precise in predicting remaining tumor size as compared to mammography. There was an 80% probability of complete pathological response when both the imaging techniques portrayed no remaining disease11. In another study, the frequency of breast malignancy was reported to be 25% in females screened on mammography for palpable breast lesions12. The sensitivity, specificity, PPV and NPV for USG was 86.84%, 99.6%, 94.29% and 99.01% compared to mammography which were 80.47%, 73.07%, 64.79% and 85.86% for mammogram6.
The study by Shen et al. described that in high-risk Chinese women ultrasound as a breast cancer screening tool is superior to mammography. All the 14 cancers were detected by USG, whereas only 8 cases were detected by mammography, making USG a more sensitive (p=0.04, 100 vs 57.1%,) imaging tool with better diagnostic accuracy (p=0.01, 0.999 vs 0.766) 13. Several studies have revealed that in determining primary tumor size, breast USG is superior to physical examination and mammography14-16. However, other studies have shown that USG, mammography and physical examination achieve equally well in detecting primary tumor size17,18. Nonetheless, few studies support that mammography is superior to both physical examination and breast ultrasound14, 19.
Herrada et al. found that in evaluating the remaining tumor size physical examination is the most accurate method when compared to both the imaging techniques. Moreover, the physical examination and mammography together were superior to physical examination and ultrasound in evaluating the remaining tumor size20. In a similar study by Fiorentino et al., it was established that physical examination was better than both the imaging techniques and that the pathology results were not enhanced by combining either of the imaging modality. In crux, mammography as a diagnostic tool was more precise in assessing tumor size than USG21.
According to Chagpar et al., after neoadjuvant chemotherapy, USG and mammography were just moderately helpful in foreseeing the remaining tumor size, with a precision of + 1 cm in 66% of cases assessed by physical examination, 70% by mammography and 75% by USG. Kappa values of (0.24 to 0.35) showed inadequate concordance amongst clinical and pathological measurements22. The two analytic imaging techniques, Breast USG and mammography are universally used in assessing the size of the tumor at the time of diagnosis.
Despite clear evidence regarding the precision of these imaging strategies in measuring primary tumor size at diagnosis time, there are apprehensions concerning their accuracy in measuring the remaining tumor size after neoadjuvant chemotherapy. Noteworthy are the concerns that the response of the primary tumor to chemotherapy may show a discrepancy, due to subsequent fragmentation, fibrosis or density change in the cancerous tissue. All these discrepancies may provide a hindrance in the residual tumor size estimation11. Therefore, a more efficient method for screening breast lesions should be recommended by implementing the use of ultrasonography for breast lesions in local settings.
In this study, ultrasonography showed more accuracy in determining the type of palpable breast lesion compared to mammography. Thus, in the future, healthcare facilities can apply and recommend ultrasonography for the prediction of the type of lesions found in breast lumps instead of going for mammography or other interventional procedure directly.
The authors would especially like to the hospital staff for their assistance and facilitation in the data collection process.
There was no conflict of interest among the authors.
The study approval was obtained by the institutional ethics and scientific review board.
Informed consent was taken from patients. Patient identity was not disclosed at any point during the research.
MS did the analysis and interpretation of data, drafted the manuscript, and finally approved the version to be published. A and L gave the concept and study design performed the acquisition analysis and interpretation of data and drafted the manuscript. N, SSU, R, S, MA did the critical revision and manuscript drafting. Authors agreed to be accountable for all aspects of the work.
- Asif HM, Sultana S, Akhtar N, Rehman JU, Rehman RU. Prevalence, risk factors and disease knowledge of breast cancer in Pakistan. Asian Pac J Cancer Prev 2014;15(11):4411-4416. doi: 10.7314/APJCP.2014.15.11.4411
- Moy L, Slanetz PJ, Moore R, Satija S, Yeh ED, McCarthy KA, et al. Specificity of mammography and US in the evaluation of a palpable abnormality: retrospective review. Radiology. 2002;225(1):176-181. doi: 10.1148/radiol.2251010999
- Lehman CD, Lee AY, Lee CI. Imaging management of palpable breast abnormalities. Am J Roentgenol. 2014;203(5):1142-1153. doi: 10.2214/AJR.14.12725
- Barclay L. Palpable Breast cancers more common in women not having annual mammography [Internet]; 2010. Available from: https://www.medscape.com/viewarticle/719311#:~:text=Palpable%20Breast%20Cancers%20More%20Common%20in%20Women%20Not%20Having%20Annual%20Mammography,Laurie%20Barclay%2C%20MD&text=March%2026%2C%202010%20%E2%80%94%20Palpable%20breast,the%20American%20College%20of%20Surgeons.
- Menhas R, Shumaila UM. Breast cancer among Pakistani women. Iran J Public Health. 2015; 44(4): 586-587.
- Zaman MU. Accuracy of mammography and ultrasound for detecting breast cancer at a breast care clinic in Karachi, Pakistan. J Biomed Graph Comput. 2011;1(1):44-50. doi: https://doi.org/10.5430/jbgc.v1n1p44
- Checka CM, Chun JE, Schnabel FR, Lee J, Toth H. The relationship of mammographic density and age: implications for breast cancer screening. Am J Roentgenol. 2012;198(3):W292-W295. doi: 10.2214/AJR.10.6049
- Pinsky RW, Helvie MA. Mammographic breast density: effect on imaging and breast cancer risk. J Natl Compr Canc Netw. 2010;8(10):1157-1165. doi: 10.6004/jnccn.2010.0085
- Smith RA, Saslow D, Sawyer KA, Burke W, Costanza ME, Evans III WP, et al. American Cancer Society guidelines for breast cancer screening: update 2003. CA Cancer J Clin. 2003;53(3):141-169. doi: 10.3322/canjclin.53.3.141
- Chalasani P. Breast Cancer. 2017 [cited 2022 Mar 15]. Available from: http://emedicine.medscape.com/article/1947145-overview#a6
- Keune JD, Jeffe DB, Schootman M, Hoffman A, Gillanders WE, Aft RL. Accuracy of ultrasonography and mammography in predicting pathologic response after neoadjuvant chemotherapy for breast cancer. Am J Surg. 2010;199(4):477-484. doi: 10.1016/j.amjsurg.2009.03.012
- McKenna Sr RJ. The abnormal mammogram radiographic findings, diagnostic options, pathology, and stage of cancer diagnosis. Cancer. 1994;74(S1):244-255. doi: 10.1002/cncr.2820741308
- Shen S, Zhou Y, Xu Y, Zhang B, Duan X, Huang R, et al. A multi-centre randomised trial comparing ultrasound vs mammography for screening breast cancer in high-risk Chinese women. Br J Cancer. 2015;112(6):998-1004. doi: 10.1038/bjc.2015.33
- Berg WA, Gutierrez L, NessAiver MS, Carter WB, Bhargavan M, Lewis RS, et al. Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology. 2004;233(3):830-849. doi: 10.1148/radiol.2333031484
- Bosch AM, Kessels AG, Beets GL, Rupa JD, Koster D, van Engelshoven JM, et al. Preoperative estimation of the pathological breast tumour size by physical examination, mammography and ultrasound: a prospective study on 105 invasive tumours. Eur J Radiol. 2003;48(3):285-392. doi: 10.1016/S0720-048X(03)00081-0
- Madjar H, Ladner HA, Sauerbrei W, Oberstein A, Prömpeler H, Pfleiderer A. Preoperative staging of breast cancer by palpation, mammography and high‐resolution ultrasound. Ultrasound Obstet Gynecol. 1993;3(3):185-190. doi: 10.1046/j.1469-0705.1993.03030185.x
- Kald BA, Boiesen P, Ronnow K, Jonsson PE, Bisgaard T. Preoperative assessment of small tumours in women with breast cancer. Scand J Surg. 2005;94(1):15-20. doi: 10.1177/145749690509400105
- Pain JA, Ebbs SR, Hern RP, Lowe S, Bradbeer JW. Assessment of breast cancer size: a comparison of methods. Eur J Surg Oncol. 1992;18(1):44-48.
- Golshan M, Fung BB, Wiley E, Wolfman J, Rademaker A, Morrow M. Prediction of breast cancer size by ultrasound, mammography and core biopsy. Breast. 2004;13(4):265-271. doi: 10.1016/j.breast.2004.05.005
- Herrada J, Iyer RB, Atkinson EN, Sneige N, Buzdar AU, Hortobagyi GN. Relative value of physical examination, mammography, and breast sonography in evaluating the size of the primary tumor and regional lymph node metastases in women receiving neoadjuvant chemotherapy for locally advanced breast carcinoma. Clin Cancer Res. 1997;3(9):1565-1569.
- Fiorentino C, Berruti A, Bottini A, Bodini M, Brizzi MP, Brunelli A, et al. Accuracy of mammography and echography versus clinical palpation in the assessment of response to primary chemotherapy in breast cancer patients with operable disease. Breast Cancer Res Treat. 2001;69(2):143-151. doi: 10.1023/A:1012277325168
- Chagpar AB, Middleton LP, Sahin AA, Dempsey P, Buzdar AU, Mirza AN, et al. Accuracy of physical examination, ultrasonography, and mammography in predicting residual pathologic tumor size in patients treated with neoadjuvant chemotherapy. Ann Surg. 2006; 243(2): 257-264. doi: 10.1097/01.sla.0000197714.14318.6f
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
