By Hira Batool1, Mervyn Hosein1, Saima Akram Butt2, Akhtar Ali3, Shafaq Saeed Roghay1, Fizza Abidi2
AFFLIATIONS:
- Department of Oral Biology, Ziauddin College of Dentistry, Ziauddin University, Karachi, Pakistan.
- Department of Oral Pathology, Ziauddin College of Dentistry, Ziauddin University, Karachi, Pakistan.
- Department of Pharmacology, Ziauddin Medical University, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-2/008
ORCID iD: 0000-0002-8232-4767
How to cite: Batool H, Hosein M, Butt SA, Ali A, Roghay SS, Abidi F. Nigella sativa in Comparison to Steroids in Managing Oral Submucous Fibrosis. Pak J Med Dent. 2022;11(2): 44-49. doi: 10.36283/PJMD11-2/008
Background: Nigella sativa (N. sativa), a natural herb, commonly known as Black seed or Kalonji, has a prolonged medicinal history of more than 2000 years. Oral submucous fibrosis (OSMF) is a chronic inflammatory disorder, which is mostly treated with steroids. This clinical trial was conducted to assess the effectiveness of N. sativa oil in comparison to steroids for treating OSMF.
Methods: This randomized clinical trial consisted of n=39 clinically diagnosed OSMF patients aged 18 years and above. Patients were divided through randomization into two groups. Group 1 was prescribed steroid lotion while Group 2 was given N. sativa oil (Cold-pressed) to be applied on the buccal mucosa for three months along with physiotherapy. Mann-Whitney U Test while the Wilcoxon Rank sum test were applied. A p-value of less than 0.05 was considered statistically significant.
Results: Thirty patients (aged 35.33±2.07) completed the trial in which the majority were males (n=28, 93.30%) and were from Urdu-speaking communities [22 (73.30%)]. Most of the patients (n= 18, 60%) were consuming a combination of Pan and Areca Nut (Chaliya), 04 (13.3%) were consuming only areca nut while 03 (10%) used Gutkha as a habit. In this trial, N. sativa was found to be equally effective as compared to steroids in reducing pain and improving the interincisal mouth opening (IIMO) (p-value >0.05%).
Conclusion: N. sativa can be used as an effective treatment option for reducing pain or burning and increasing interincisal mouth opening in patients with OSMF without producing any side effects.
Keywords: Nigella sativa; Oral Submucous Fibrosis; Steroids; Head and Neck Squamous Cell Carcinoma.
Nigella sativa (N. sativa) commonly known as Black seed or Kalonji, is a natural herb that belongs to the family Ranunculaceae1. It is mainly cultivated in Pakistan, India, Iran, Turkey, Saudi Arabia, Southern Europe and the Middle East region. Seeds and oil of N. sativa have a prolonged history of consumption in food and medicine in India2. Various studies have been carried out to establish the antioxidant, anti-inflammatory, antihypertensive, anticancer and immunomodulatory properties of N. sativa3,4 (Figure 1).

Figure 1: Nigella sativa oil and seeds5.
Oral submucous fibrosis (OSMF) is described as a premalignant, chronic inflammatory disorder, which can affect any region of the oral cavity6. It has a prevalence of about 0.03% – 6.42% and a malignant transformation rate of 7-30% 7. Epidemiological studies have shown an increase in the number of cases from 2 million to 5 million cases worldwide with a maximum number of cases being reported in the second and third decades of life8,9. There is no definitive treatment available for treating OSMF due to its complex etiology10. Steroids are most commonly used in managing OSMF but their prolonged use is not advised11. Hence, this trial aimed to assess the effect of N. sativa oil in improving the pain and limited mouth opening in OSMF.
This was a randomized clinical trial comprising of n=39 clinically diagnosed OSMF patients recruited from the Department of Oral Medicine, Ziauddin College of Dentistry, using a non-probability consecutive sampling technique. Calculation of Sample size was done using sealed envelope considering 5% significance level and 90% power of the test12,13. The overall sample size calculated was 12 per group which was increased to 20, to account for the dropouts, loss of follow up and other reasons. Ethical Approval for this study was taken from the Ethics Review Committee of Ziauddin University (Reference code: 2130520HBOM). This trial was also registered on the website www.clinicaltrials.gov (NCT04476420). Clinically diagnosed OSMF patients aged 18 years and above who were willing to quit the habit, those who have not received any treatment for Oral submucous fibrosis in the last three months and were willing to come for the follow-up visits were included in the research. Patients with a history of using corticosteroids and pain medications, those who had a history of malignancy or any other oral lesion and are allergic to the drugs used in this trial were excluded. The study data was collected in the form of a proforma.
After enrollment, patients were randomly divided into two groups i.e., Group 1 (Steroid group) and Group 2 (N. sativa group). Randomization was done using sealed envelope. Group 1 Participants were prescribed steroid lotion (Betamethasone valerate 0.1%) and were asked to apply 1 ml of it buccally for 1 minute along with physiotherapy exercise using the same technique as discussed by Vijayakumar et al. Group 2 patients were given cold-pressed N. sativa oil and were asked to apply it in the same quantity and duration as described for Group1 along with physiotherapy14,15.
Pretreatment measurement of pain/burning sensation and interincisal mouth opening (IIMO) was done using the Visual analog scale (VAS) and Vernier caliperrespectively13,16. The treatment was given for three months. Analysis was done using SPSS version 20. Numerical data were presented as mean and standard deviation. Frequency and percentages were calculated for categorical data. The mean difference in values between the two groups was measured using Mann-Whitney U Test while the Wilcoxon Rank sum test was used to measure the difference between the baseline value and value recorded at the end of the trial and a p-value of less than 0.05 was considered statistically significant.
Total 39 OSMF patients were included while only 30 patients completed the trial. The results showed a mean age of 35.33±2.07 among which 28(93.30%) were males and 02(6.70%) were females (Figure 2). Participants 10(33.3%) had completed matriculation followed by 08 (26.7%) participants who were illiterate. Most of the participants were Urdu speaking [22 (73.30%)] followed by 04 (13.30%) participants from the Sindhi community. The majority (n= 18, 60%) of the participants were consuming a combination of habits (especially Pan and Chaliya) while 04 (13.3%) were consuming Chaliya (areca nut) as a single habit followed by 03 (10%) patients who were taking Gutkha (Figure 3).
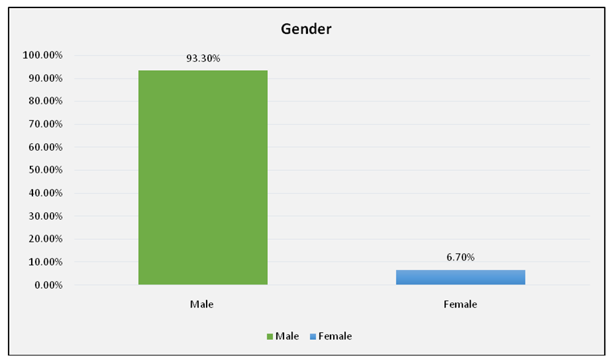
Figure 2: Gender distribution of the study.
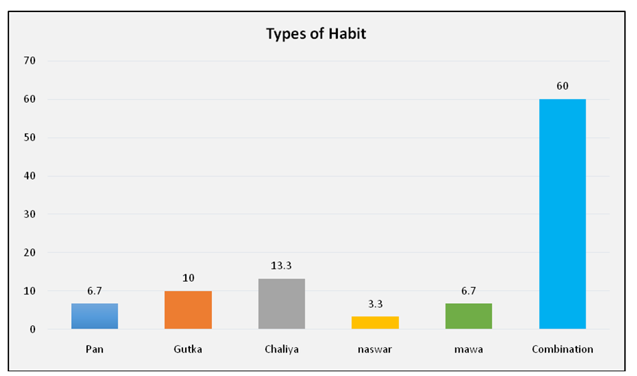
Figure 3: Type of habit consumption.
The results for reduction of pain or burning sensation and increase in IIMO showed a non-significant p-value between the two groups suggesting that both the treatments were equally effective in reducing the pain/burning sensation and improving IIMO (Table 1).
Table 1: Evaluation of pain/burning sensation and interincisal mouth opening between the two groups.
| Visits | Steroid group | Nigella group | p-Value |
| Pain or burning sensation | |||
| Baseline | 24.67±8.040 | 34.67±7.61 | 0.374 |
| 1st | 19.33±7.33 | 26.67±6.22 | 0.452 |
| 2nd | 14.00±6.60 | 17.67±4.54 | 0.651 |
| 3rd | 8.67±6.00 | 10.67±3.58 | 0.777 |
| Interincisal mouth opening | |||
| Baseline | 24.67±2.79 | 22.67±2.21 | 0.580 |
| 1st | 26.87±2.76 | 25.13±2.28 | 0.633 |
| 2nd | 28.33±2.76 | 27.60±2.21 | 0.838 |
| 3rd | 30.60±2.69 | 30.53±2.00 | 0.984 |
*p-value of less than 0.05 was considered statistically significant, *Mann-Whitney U Test was applied.
In addition, the results of present study showed statistically significant improvement in pain or burning sensation and IIMO in both groups when the baseline values were compared with the values recorded on the last visit (Table 2).
Table 2: Comparison of baseline and last visit values in both groups.
| Groups | Intervention | Clinical Parameters
|
p-Value |
| Pain/ Burning | |||
| Steroid | Before | 24.67±8.040 | 0.009* |
| After | 8.67±6.00 | ||
| N. sativa | Before | 34.67±7.61 | <0.001* |
| After | 10.67±3.58 | ||
| Interincisal Mouth Opening | |||
| Steroid | Before | 24.67±2.79 | <0.001* |
| After | 30.60±2.69 | ||
| N. sativa | Before | 22.67±2.21 | <0.001* |
| After | 30.53±2.00 | ||
*p-value of less than 0.05 was considered statistically significant, *Wilcoxon Rank sum test.
Two important clinical parameters were assessed in this trial; pain/burning and IIMO. It was observed that N. sativa was as effective as steroids in improving these parameters in patients with OSMF. This finding is comparable to a study conducted by Pipalia et al. in 2016 however; they have used N. sativa oil capsules (500mg) in their research while we have given N. sativa oil to be used topically over the buccal mucosa10. In addition, the analysis showed no significant difference in the reduction of pain or burning or IIMO when the two groups were compared. This finding of the investigation is following a study conducted by Deepak et al., in which turmeric is used in comparison to steroids, however, they also used curcumin tablets (500mg) and compared it with topical steroids17.
N.sativa is an inexpensive, easily available herb with many beneficial properties. The important constituents present in N. sativa seeds include thymoquinone (TQ), carvacrol, t-anethol, thymol, a variety of alkaloids and Alpha-hederin (α-HN) 18. TQ is the most active pharmacological component, which is responsible for most of the activities exhibited by N. sativa19. It has been used in various clinical trials for decades. A prospective open-label trial was conducted in 2019 to treat oral mucositis in head and neck squamous cell carcinoma patients (n= 40). In this trial, N. sativa oil mouthwash and Magic mouthwash were given to the research participants. Results of this trial indicated a significant reduction in the severity of oral mucositis after 3-4 weeks of radiotherapy20. Another clinical trial was conducted to treat oral mucositis in patients with acute myeloid leukemia (n=54) using N. sativa oil mouth rinse and magic mouthwash respectively. The result of this trial reported improvement in the severity of oral mucositis in N. sativa group with a significant reduction in the pain score. This suggests that N. sativa has strong anti-inflammatory properties and can be used beneficially to treat OSMF21.
The results of present trial showed a mean age of 35.33±2.07 that is comparable to studies conducted by Raffat et al., Shakunthala et al. and Srivastava et al. reported in literature22-24. The results for gender distribution showed male predilection (n=28, 93.30%) in current study. Roghay et al. and Ray et al. have also shown a similar increase in the frequency of cases in males as compared to females25,26. In contrast, research outcome reported by Mohiuddin et al. has shown an increased prevalence of OSMF in females [370(78.4%)] as compared to males [102 (21.6%)] 27.
Jain et al. and Tariq et al. have shown an increase in the number of cases in people who were illiterate28,29. Their finding is slightly different from the results because most of the study participants had completed matriculation followed by those who had no education at all. The reason for this increased prevalence in less-educated people could be that people with low education levels are less aware of the damage caused by Pan, Gutkha and Chaliya. Hence, OSMF is more common in people with low education.
The results regarding ethnicity showed an increase in the number of cases being reported from Urdu-speaking communities. Muhammad et al. and Akhlaq et al. have also reported that most of their research participants belong to the Urdu-speaking community30,31. It has been reported that Urdu speaking possesses a strong Indian culture of using Pan, Gutkha and Chaliya which results in increased prevalence of OSMF in this ethnicity32.
Most of the study participants were consuming a combination of pan and Chaliya. A study reported increased consumption of Gutkha followed by Naswar, which contrasts with the findings. In another research conducted by Rubab et al. it has been observed that Gutkha consumption was more in stage II OSMF patients as compared to stage I followed by pan consumption in stage II OSMF patients32. Short duration and use of non-probability consecutive sampling techniques are the two possible limitations of this trial. Research with a longer duration would help to find results that are more effective and would allow finding out the long-term effects of using N. sativa oil in OSMF.
N. sativa can be used as an effective treatment option for reducing pain or burning and increasing IIMO in patients with OSMF.
The authors are thankful to the Ziauddin University for providing financial assistance for this research. We would also like to acknowledge Prof. Saeeda Baig for providing her expert opinion in improving this manuscript.
The authors have no conflict of interest to declare.
Ethics approval was taken from the Ethics Review Committee of Ziauddin University (Reference code: 2130520HBOM). This trial was also registered on the website www.clinicaltrials.gov (NCT04476420).
This research was funded by Ziauddin University, Clifton Campus (Karachi).
Informed consent was taken from patients. Patient identity was not disclosed at any point during the research.
HB conceptualized and conducted the whole trial and wrote the manuscript, SA helped in writing the manuscript, AA helped in statistical analysis of the data, SS and FA helped in writing the results, MH overall supervised and proofread the manuscript.
- Amin B, Hosseinzadeh H. Black cumin (Nigella sativa) and its active constituent, thymoquinone: an overview on the analgesic and anti-inflammatory effects. Planta Med. 2016;82(01/02):8-16. doi: 10.1055/s-0035-1557838
- Srinivasan K. Cumin (Cuminum cyminum) and black cumin (Nigella sativa) seeds: traditional uses, chemical constituents, and nutraceutical effects. Food Qual Saf. 2018;2(1):1-16. doi: 10.1093/fqsafe/fyx031
- Kotowski U, Heiduschka G, Kadletz L, Fahim T, Seemann R, Schmid R, et al. Effect of thymoquinone on head and neck squamous cell carcinoma cells in vitro: Synergism with radiation. Oncol Lett. 2017;14(1):1147-1151. doi: 10.3892/ol.2017.6189
- Goyal SN, Prajapati CP, Gore PR, Patil CR, Mahajan UB, Sharma C, et al. Therapeutic potential and pharmaceutical development of thymoquinone: a multitargeted molecule of natural origin. Front Pharmacol. 2017;8:1-19. doi: 10.3389/fphar.2017.00656
- Medikonda; 2022 [cited 2022 Jan 6]. Available from: https://medikonda.com/products/black-seed-nigella-sativa-oi.
- Patil S, Santosh BS, Maheshwari S, Deoghare A, Chhugani S, Rajesh PR. Efficacy of oxitard capsules in the treatment of oral submucous fibrosis. J Cancer Res Ther. 2015;11(2):291-294. doi: 10.4103/0973-1482.136023
- Bari S, Metgud R, Vyas Z, Tak A. An update on studies on etiological factors, disease progression, and malignant transformation in oral submucous fibrosis. J Cancer Res Ther. 2017;13(3):399-405. doi: 10.4103/0973-1482.179524
- Shih YH, Wang TH, Shieh TM, Tseng YH. Oral submucous fibrosis: a review on etiopathogenesis, diagnosis, and therapy. Int J Mol Sci. 2019;20(12):1-22. doi: 10.3390/ijms20122940
- Hosein M, Mohiuddin S, Fatima N. Association between grading of oral submucous fibrosis with frequency and consumption of areca nut and its derivatives in a wide age group: A multi-centric cross sectional study from Karachi, Pakistan. J Cancer Prev. 2015; 20(3): 216-222. doi: 10.15430/JCP.2015.20.3.216
- Pipalia PR, Annigeri RG, Mehta R. Clinicobiochemical evaluation of turmeric with black pepper and Nigella sativa in management of oral submucous fibrosis—a double-blind, randomized preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(6):705-712. doi: 10.1016/j.oooo.2016.07.023
- Beeraka SS, Natarajan K, Patil R, Manne RK, Prathi VS, Kolaparthi VSK. Clinical and radiological assessment of effects of long-term corticosteroid therapy on oral health. Dent Res J (Isfahan). 2013; 10(5): 666-673.
- Sealed envelope. ; 2022 [cited 2022 Jan 6]. Available from: https://sealedenvelope.com/
- Hazarey VK, Sakrikar AR, Ganvir SM. Efficacy of curcumin in the treatment for oral submucous fibrosis-A randomized clinical trial. J Oral Maxillofac Pathol. 2015; 19(2): 145-152. doi: 10.4103/0973-029X.164524
- Vijayakumar M, Priya D. Physiotherapy for improving mouth opening & tongue protrusion in patients with Oral submucous fibrosis (OSMF)–case series. Int J Pharm Sci Health Care. 2013;3(2):50-58.
- Fallah Huseini H, Amini M, Mohtashami R, Ghamarchehre M, Sadeqhi Z, Kianbakht S, et al. Blood pressure lowering effect of Nigella sativa seed oil in healthy volunteers: A randomized, double‐blind, placebo‐controlled clinical trial. Phytother Res. 2013;27(12):1849-1853. doi: 10.1002/ptr.4944
- Fatima J, Kaul R, Jain P, Saha S, Halder S, Sarkar S. Clinical measurement of maximum mouth opening in children of Kolkata and its relation with different facial types. J Clin Diagn Res. 2016; 10(8): ZC01-ZC05. doi: 10.7860/JCDR/2016/21232.8217
- Deepak T, Manjunath M, Thakur H. Efficacy of curcumin and topical steroids in the treatment for oral submucous fibrosis: A comparative study. J Pharm Bioallied Sci. 2021; 13(Suppl 1): S542-S548. doi: 10.4103/jpbs.JPBS_687_20
- Ahmad A, Husain A, Mujeeb M, Khan SA, Najmi AK, Siddique NA, et al. A review on therapeutic potential of Nigella sativa: A miracle herb. Asian Pac J Trop Biomed. 2013;3(5):337-352. doi: 10.1016/S2221-1691(13)60075-1
- Kooti W, Hasanzadeh-Noohi Z, Sharafi-Ahvazi N, Asadi-Samani M, Ashtary-Larky D. Phytochemistry, pharmacology, and therapeutic uses of black seed (Nigella sativa). Chin J Nat Med. 2016;14(10):732-745. doi: 10.1016/S1875-5364(16)30088-7
- Ameen HA, Mohammed MO, Ahmed KM, Ali RH, Saeed KA, Hussain SA. Anti-inflammatory effect of Nigella sativa oil on chemoradiation-induced oral mucositis in patients with head and neck cancers. Int J Curr Pharm Res. 2019;11(5):58-64. doi:10.22159/ijcpr.2019v11i5.35704
- Hussain SA, Mohammed Ameen HA, Mohammed MO, Ahmed KM, Hama-Gareb Ali R, Safar BM,et al. Nigella sativa oil mouth rinse improves chemotherapy-induced oral mucositis in patients with acute myeloid leukemia. BioMed Res Int. 2019 Oct 30;2019:1-11.doi: 10.1155/2019/3619357
- Raffat MA, Hadi NI, Hosein M, Zubairi AM, Ikram S, Akram Z. Differential expression of salivary S100A7 in oral submucous fibrosis. Saudi Dent J. 2019;31(1):39-44. doi: 10.1016/j.sdentj.2018.09.007
- Shakunthala G, Annigeri RG, Arunkumar S. Role of oxidative stress in the pathogenesis of oral submucous fibrosis: A preliminary prospective study. Contemp Clin Dent. 2015; 6(Suppl 1): S172-S174. doi: 10.4103/0976-237X.166823
- Srivastava R, Jyoti B, Pradhan D, Siddiqui Z. Prevalence of oral submucous fibrosis in patients visiting dental OPD of a dental college in Kanpur: A demographic study. J Family Med Prim Care. 2019; 8(8): 2612-2617. doi: 10.4103/jfmpc.jfmpc_465_19
- Roghay SS, Razi A, Hosein M, Shahid M, Butt S, Batool H. Expression of salivary resistin in oral premalignant individuals. J Adv Med Med Res. 2020:127-133. doi: 10.9734/JAMMR/2020/v32i230376
- Ray JG, Chatterjee R, Chaudhuri K. Oral submucous fibrosis: a global challenge. Rising incidence, risk factors, management, and research priorities. Periodontol 2000. 2019;80(1):200-212. doi: 10.1111/prd.12277
- Mohiuddin S, Fatima N, Hosein S, Hosein M. High risk of malignant transformation of oral submucous fibrosis in Pakistani females: A potential national disaster. J Pak Med Assoc. 2016;66(11):1362-1366.
- Jain A, Taneja S. Oral submucous fibrosis in pediatric patients: a systematic review and protocol for management. Int J Surg Oncol. 2019;2019:1-6. doi: 10.1155/2019/3497136
- Tariq H, Ahmed S, Naz M, Naureen A. Frequency of oral sub mucous fibrosis and its correlation with the level of education in patients coming to a tertiary care hospital of Karachi from January 2018 to December 2018. Asian Pac J Cancer Care. 2020;5(3):157-160. doi: 10.31557/APJCC.2020.5.3.157-160
- Mohammad H, Hadi NI, Ahmed F, Younus S. Comparison of frequency of habits among different stages of oral submucous fibrosis. Pak J Med Dent. 2016;5(1):15-20.
- Akhlaq H, Jamal Q, Ismail MO. Risk factors associated with decreased mouth opening among patients with oral submucous fibrosis (OSMF). Ann ASH KMDC. 2014;19(1):3-9.
- Rubab Z, Mughal AM, Baig S, Lucky MH, Azeem M. Relationship of human papilloma virus with trismus in chewable tobacco users. Pak J Med Dent. 2013;2(1):3-11.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
