By Danial Arshad, Nazish Fatima, Salman Zafar, Paras Naseem, Sana Lodhi
AFFLIATIONS:
Medident Clinics, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-2/006
ORCID iD: 0000-0003-3416-3396
How to cite: Arshad D, Fatima N, Hosein M, Zafar S, Naseem P, Lodhi S. Effect of 635nm Diode Laser on Radiation Induced Xerostomia Patients. Pak J Med Dent. 2022;11(2): 29-35. doi: 10.36283/PJMD11-2/006
Background: Xerostomia, one of the most major side effects of radiotherapy in patients with oropharyngeal cancer, has a compromising effect on the quality of life. The aim of this study was to evaluate the effect of 635nm low-level laser on salivary flow rate and quality of life (QoL) in post-radiotherapy oropharyngeal cancer patients.
Methods: A prospective study was conducted on patients (n=34) with persistent post-radiotherapy xerostomia received low level laser therapy (LLLT) (635nm) on the three major salivary glands twice a week for 12 weeks. For each point, dose was 18.75 J/cm2, irradiation time was 15 s, energy was 1.5 J. Energy for each session was 33 J and laser tip diameter was 0.08cm2. Extra oral points were marked over the parotid gland (6 points), submandibular (3points) and sublingual gland (2 points). Unstimulated and stimulated salivary flow rate (SFR) and quality of life (QoL) using University of Washington (UW) QoL questionnaire were assessed. Unstimulated SFR and QOL scores were normally distributed and hence paired t-test was used. A p-value ≤0.05 was considered as statistically significant.
Results: The mean unstimulated SFR was significantly increased by 0.16 units after LLLT (p=0.001). Similarly, the median stimulated SFR significantly increased by 0.45 units post LLLT respectively (p=0.001). The mean QoL was significantly increased by 591.32 units after LLLT (p≤0.05).
Conclusion: Low level laser therapy (LLLT) demonstrates to be effective in increasing salivary flow rate and the QoL scores hence mitigating salivary hypofunction and improving overall quality of life of patients.
Keywords: Low-Level Laser Therapy; Xerostomia.
Oropharyngeal cancers are malignant tumors arising from the upper aerodigestive tract that include the lip, mouth, nose, tongue, and structures adjacent to the oral cavity such as sinuses, pharynx, vocal cords (larynx), etc1. Three different treatment techniques have been established for oropharyngeal cancer which include radiotherapy (RT), chemotherapy and surgery. Surgery is considered the standard treatment option since its purpose is to remove the tumor with slight impairment of surrounding healthy tissues; although in advanced stages, RT is used as an adjunct to surgery or chemotherapy2.
Whenever radiation therapy is included in the treatment of oropharyngeal cancers, healthy tissues that fall in the zone of radiation are also adversely affected. The degree of damage to healthy tissues depends on the dose of radiation per segment, total radiation dosage, volume irradiated, and dose distribution in the tissues2. Oro-pharyngeal cancer patients receiving radiotherapy with doses of 50-70 Gy in cervicofacial fields show radiation-induced atrophy of salivary tissue present in the area of radiation and therefore such patients present with long-term oral complications3. The oral complications may manifest during the radiotherapy (acute) or post-radiotherapy (chronic) period and may impair basic oral functions of the patient, including diminished salivary flow rate, sticky, dry or burning of the oral tissues, difficulty in chewing and swallowing, altered taste, sore throat, increased dental caries, hoarseness of voice, halitosis and difficulty in retention of dentures. These complication in turn affect their quality of life, (QoL) as they are supposedly long term or even permanent4-6.
Xerostomia is a prevalent problem, compelling many patients to visit specialists such as gastroenterologists, dentists and internal medicine physicians since xerostomia may also be a manifestation of an underlying local or systemic disease7. The normal range of salivary volume falls between 0.5L to 1.0L per day and is maintained by masticatory and gustatory reflexes8. Salivary gland hypofunction is established when the flow rate falls below 0.20mL/min 9,10.
Low-level laser therapy (LLLT) has been recommended as a possible beneficial treatment as there is no definitively approved therapy modality for the reduction of RT-induced xerostomia and hyposalivation2. Previous studies that focused on higher wavelengths of laser such as 808, 810, 980nm showed LLLT to increase salivary flow rate (SFR) and reduce xerostomia by improving the function of damaged, but viable, residual, salivary gland tissue2,13-16. Laser energy through biochemical and photophysical techniques provides energy to the cell. Chromophores present in the mitochondria soak up visible laser energy which results in increased Adenosine triphosphate (ATP) production, followed by an elevated cellular proliferation and protein synthesis, which assist in tissue repair as well as having a palliative and anti-inflammatory effect (Figure 1)13. Therefore, purpose of this study was to explore the effect of LLLT at 635nm as no such research has been conducted at this wavelength and utilizing this method in the Indo-Pak/Asian region. This method is cost effective and has the potential to give long term relief to patients suffering from the debilitating side effects of radiation induced xerostomia.
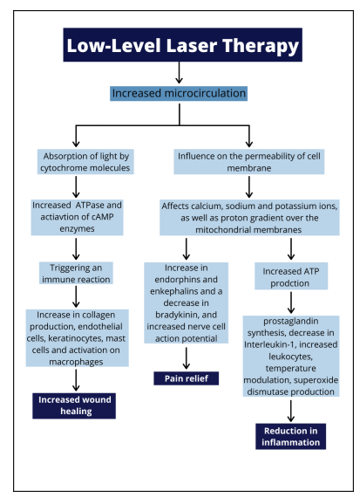
Figure 1. Effect of Low-Level Laser Therapy (LLLT) on the body.
A prospective study was conducted with n=34 post radiation treated and recovered oropharyngeal cancer patients. The study was conducted at a clinic with the facilities of low-level lasers and patients were recruited. The research was approved by the Ethics Review Committee Reference code 2480820DAOM.
All patients that were recruited complained of persistent xerostomia after receiving megavoltage radiation therapy with fields that included all the major salivary glands. The total radiation dose received by all the patients was between 50 – 70 Gy. All patients were above or equal to 18 years and read and signed the informed consent. The patients received their last radiation dose 3-36 months prior to inclusion in the study protocol. Patients with other determined causes of xerostomia. Patients who are undergoing active RT. Patients who could not provide informed consent or who had head and neck tumors originating outside the oropharyngeal area including salivary gland tumors were excluded from the study.
This laser therapy was performed with a continuous wave diode laser device (Lasotronix Smart M Pro, Lasotronix® Poland) previously calibrated by the manufacturer. Parameters employed were included wavelength – 635nm (visible spectrum), power 100mW, dose for each point – 18.75J/cm2, irradiation time for each point 15s, energy for point 1.5J, energy for each session 33J, and laser tip diameter was 0.08cm2.
A total number of 24 laser sessions were conducted: every week two laser sessions were performed over the course of 12 weeks. The tip of the laser hand-piece was positioned in 1mm away from patients’ soft tissues superficial to the major salivary glands. The LLLT was applied at specific points on each salivary gland: 6 points over the parotid gland, 3 over the submandibular gland and 2 intraorally over the sublingual gland. Altogether, a total of 22 points received LLLT in each session (Figure 2; A and B)
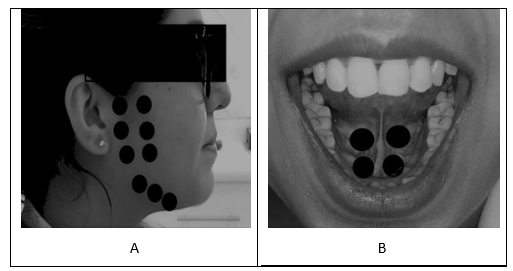
Figure 2: (A) representing the extra-oral low-level laser therapy (LLLT) points while (B) showing the intra-oral low-level laser therapy (LLLT) points.
As a safety precaution, both the laser operator as well as the patients wore protective eyewear with special lenses to block any hazardous rays. Proper standard operating procedures were followed during clinical trials of this study due to the COVID-19 pandemic. The operator also wore personal protective equipment (PPE) with a respirator mask to minimize exposure. Clear plastic wrappings were used on the laser handpiece as a protective barrier, which were disposed of and replaced after each patient. 80% alcohol-based disinfectant was used to disinfect instruments that could not be autoclaved. Disposable items were discarded.
Unstimulated and stimulated sialometry to measure salivary flow rate was recorded at two intervals: baseline (T0) and once the 24th LLLT session (TF) was completed. Patients were given appointments for before noon on designated days. Two hours before each session, the patients were instructed to refrain from eating, drinking and brushing their teeth. The patients were seated with their eyes open and their heads bent slightly forward throughout the collection of saliva.
In unstimulated sialometry, participants were asked to empty the contents of their mouth (including saliva or mucous) prior to the sample collection. Once this was achieved, the patients were requested to gather as much saliva as possible in the floor of their mouth and not swallow for 60 seconds. Using a glass funnel, the gathered saliva was then expelled in a millimeter-marked tube and this task was repeated a minimum of four times. After the tubes were shaken vigorously, the SFR per minute was calculated and the volume of saliva measured.
In stimulated sialometry, a cotton applicator was used to apply 2% citrate solution on the dorsolateral surface of the tongue. The method of salivary collection and its assessment were carried out in the same manner mentioned above. The UW-QOL (version 4) is a tool used to determine the health-related quality of life of patients who have received treatment for oropharyngeal cancer. The UW-QOL is a validated tool focused mainly on assessing quality of life focusing on the saliva and its presence and quality. The questionnaire had 12 close ended questions with scores ranging from 0-100. Total scores were assessed with a higher score indicative of improvement in QoL. The scores were assessed at baseline (T0) and after the final LLLT session (TF). An Urdu version of the QoL was translated by a certified translator and was then verified by another translator as well was also used. SPSS version 25 was used for statistical analysis. Normality was checked using the Shapiro-Wilks test. Unstimulated SFR and QOL scores were normally distributed and hence paired t-test was used. Stimulated SFR was non-normally distributed and later Wilcoxon signed-ranks test was used. A p-value ≤0.05 was considered as statistically significant.
The subjects (n=37) were recruited out of which 3 dropped out due to COVID-19 infections. The demographics of the patients and their clinical history is mentioned in Table 1. The mean unstimulated saliva flow rate (SFR) was significantly increased by 0.16 units after LLLT (p≤0.05).
Table 1: Descriptive analysis of tumors and treatments.
| Characteristics | Frequency (n) (%) | Frequency (n) (%) | ||
| Gender | Male | Female | ||
| 32(94.1) | 2(5.9) | |||
| Tobacco Users | Previous | Current | ||
| 13(38.2) | 21(61.8) | |||
| Alcohol Consumption | Alcoholic | Non-alcoholic | ||
| 6(17.6) | 28(82.4) | |||
| Stage of Tumor | I | II | III | IV |
| 4(11.7) | 16(47.1) | 12(35.3) | 2(5.9) | |
| Chemotherapy | Yes | No | ||
| 24(29.4) | 10(70.6) | |||
Similarly, the median stimulated SFR significantly increased by 0.45 units post LLLT respectively (p≤0.05) and the mean QOL was significantly increased by 591.32 units after LLLT (p≤0.05) (Table 2).
Table 2: Comparison between pre and post low-level laser therapy (LLLT) unstimulated and stimulated saliva flow rate (SFR) along with comparison between pre and post LLLT quality of life (QoL).
| Evaluation | Mean±SD (ml/min) | p-Value | |
| Baseline (T0) | Final (TF) | ||
| Unstimulated Sialometry | 0.05±0.025 | 0.21±0.082 | *0.001 |
| Stimulated Sialometry | 0.300 (0.200-0.400) | 0.750 (0.630-0.930) | **0.001 |
| Average and Standard Deviation (Scores) | |||
| Quality of Life (QoL) | 695.88±190.73 | 1287.20±123.57 | *0.001 |
Paired t-test* for unstimulated SFR and Wilcoxon signed-ranks test** for stimulated SFR along with paired t-test for QoL scores showing statistically significant results.
There was insignificant difference seen in stimulated and unstimulated SFR with respect to gender and those who received chemotherapy (Table 3).
Table 3: Stratification of mean difference in unstimulated and stimulated saliva flow rate (SFR) with respect to gender and chemotherapy.
| Gender | Change in Unstimulated SFR | p-Value | Change in Stimulated SFR | p-Value |
| Mean±SD (ml / min) | Mean±SD (ml / min) | |||
| Male | 0.1569±0.08771 | 0.35 | 0.4975±0.25108 | 0.361 |
| Female | 0.2200±0.16971 | 0.3300±0.11314 | ||
| Chemotherapy | ||||
| Yes | 0.1310±0.06999 | 0.228 | 0.4430±0.27321 | 0.505 |
| No | 0.1729±0.09742 | 0.5063±0.23954 | ||
The mean change in unstimulated and stimulated SFR were compared between males and females, as well as chemotherapy exposure as yes/no. There was insignificant difference with respect to the gender and chemotherapy status (p>0.05).
Thirty-seven subjects were selected to take part in this prospective study. However, due to COVID-19, 3 of 37 participants had to withdraw from the study, making a final count of 34 participants. This study involved the use of a laser of 635nm wavelength, which was the first time this wavelength was used for salivary stimulation. Wavelength laser (635 nm) was used over the duration of 12 weeks, by the end of which a significant increase in salivary flow and improved quality of life was observed. Other studies that utilized different wavelengths also reported showing similar results14-16.
Among other complications, persistent xerostomia is a common complaint of cancer patients who have undergone radiotherapy. This in turn adversely affects their functionality leading to poor quality of life. The aim of this research was to highlight the use of LLLT as a method of increasing the diminished salivary flow rate, by stimulating the residual damaged but surviving salivary gland cells, which sequentially improves quality of life. Low level laser therapy enhances microcirculation as well as influences other cellular functions including stimulating glandular cell proliferation, accelerating cellular respiration, protein synthesis, increases intracellular calcium levels and increases production of reactive oxygen species (ROS)13,14,17. Additionally, LLLT has proven to be beneficial in terms of being conservative and well-tolerated15. The 635 nm wavelength was chosen to reduce the photothermal effects on the superficial tissues and to penetrate to deeper tissues15. do Nascimento et al. and Kanehira et al., in their respective studies noted significant improvements in salivary flow of patients undergoing RT by inducing remaining functioning salivary gland cells using LLLT of higher wavelengths. The study results also show that LLLT has noticeably increased salivary, making the hypothesis credible16, 9.
The UW-QoL is a concise measurement tool that helps in the evaluation of the physical, functional, social and emotional aspects of a patient. In current study, this tool was used to determine how hindrances in basic functions such as speech, mastication, movement etc. negatively impact a patient’s QoL18. Four versions of this questionnaire have been introduced. For this study, the latest version i.e., version 4 was used. The v4 was preferred as this questionnaire analyzes the following 12 domains using close-ended questions: pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder, taste, saliva, mood, anxiety. The UW-QoL v4 is unique in the sense that it also includes importance ratings, which are scored from numbers 1 to 5 (1 being the least important and 5 being extremely important). This feature allows a better assessment of the patient’s subjective response to the questionnaire. Furthermore, the patient is also asked 3 global health-related quality of life questions as well as a supplementary open-ended entry field, where patients are free to add any other relevant details19,20. Patients with oropharyngeal cancers are reported to have poor scores on the QoL questionnaire. Symptoms that arise due to radiation including xerostomia tend to reduce physical, emotional and social functioning leading to an unsatisfactory QoL21, 22.
Another factor that we wanted to asses was if LLLT had any difference on gender and on patients who had received chemotherapy. There was insignificant difference in the results and we can conclude that LLLT has no effect based on gender and has the same effects on whether patients received chemotherapy or not. The present study showed significant positive results even during the COVID-19 pandemic. It should be taken into consideration when interpreting the outcome of the research as the immune-compromised status of these patients with xerostomia made sampling quite difficult. During this time patients had restricted access to health care services due to the closure of hospitals and OPDs. However, to minimize risk and ensure the safety of the patients, proper protocols and measures were implemented when conducting LLLT. Due to the ongoing pandemic, a randomized double-blind control trial (which would have produced more significant results) was not possible. Therefore, the pre- and post-approach was the best possible option.
This prospective study has determined that LLLT enormous potential to treat post-radiation xerostomia. Patients who received LLLT showed significant elevation in their salivary flow rates, which in turn had substantial improvements on their quality of life.
The authors would like to acknowledge the hard work and support of Ms. Hannah Farrukh and Ms. Rameen Faisal for their contributions to this research.
The authors declared no conflict of interest.
The study was approved by the Ethics Review Committee (Reference Code: 2480820DAOM) (ClinicalTrials.gov Identifier: NCT04738227).
Informed consent was taken from all subjects participating in the study before the commencement of clinical procedures.
DA did the conceptualization of study, literature search and data collection. DA and SL wrote the manuscript. MH, NF, SZ and PN did the proof reading and overall evaluation.
- Akhtar A, Hussain I, Talha M, Shakeel M, Faisal M, Ameen M, et al. Prevalence and diagnostic of head and neck cancer in Pakistan. Pak J Pharm Sci. 2016;29(5 Suppl):1839-1846.
- Palma LF, Gonnelli FA, Marcucci M, Dias RS, Giordani AJ, Segreto RA, et al. Impact of low-level laser therapy on hyposalivation, salivary pH, and quality of life in head and neck cancer patients post-radiotherapy. Laser Med Sci. 2017;32(4):827-832. doi: 10.1007/s10103-017-2180-3
- Gonnelli FA, Palma LF, Giordani AJ, Deboni AL, Dias RS, Segreto RA, et al. Low-level laser for mitigation of low salivary flow rate in head and neck cancer patients undergoing radiochemotherapy: a prospective longitudinal study. Photomed Laser Surg. 2016;34(8):326-330. doi: 10.1089/pho.2016.4104
- Jellema AP, Slotman BJ, Doornaert P, Leemans CR, Langendijk JA. Impact of radiation-induced xerostomia on quality of life after primary radiotherapy among patients with head and neck cancer. Int J Radiat Oncol Biol Phys. 2007;69(3):751-760. doi: 10.1016/j.ijrobp.2007.04.021
- Abel E, Silander E, Nyman J, Björk-Eriksson T, Hammerlid E. Long-term aspects of quality of life in head and neck cancer patients treated with intensity modulated radiation therapy: a 5-year longitudinal follow-up and comparison with a normal population cohort. Adv Radiat Oncol. 2020;5(1):101-110. doi: 10.1016/j.adro.2019.07.015
- Jensen SB, Vissink A, Limesand KH, Reyland ME. Salivary gland hypofunction and xerostomia in head and neck radiation patients. J Natl Cancer Inst Monogr. 2019;2019(53):95-106. doi: 10.1093/jncimonographs/lgz016
- Alkhateeb AA, Mancl LA, Presland RB, Rothen ML, Chi DL. Unstimulated saliva-related caries risk factors in individuals with cystic fibrosis: A cross-sectional analysis of unstimulated salivary flow, pH, and buffering capacity. Caries Res. 2017;51(1):1-6. doi: 10.1159/000450658
- Jensen S, Pedersen A, Reibel J, Nauntofte B. Xerostomia and hypofunction of the salivary glands in cancer therapy. Support Care Cancer. 2003;11(4):207-225. doi 10.1007/s00520-002-0407-7
- Kanehira T, Hongou H, Asano K, Morita M, Maeshima E, Matsuda A, et al. A simple test for salivary gland function measuring resting and stimulated submandibular and sublingual secretions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(2):197-203. doi: 10.1016/j.oooo.2013.10.001
- Pedersen AM, Sørensen CE, Proctor GB, Carpenter GH, Ekström J. Salivary secretion in health and disease. J Oral Rehabil. 2018;45(9):730-746. doi: 10.1111/joor.12664
- Botelho J, Machado V, Proença L, Oliveira MJ, Cavacas MA, Amaro L, et al. Perceived xerostomia, stress and periodontal status impact on elderly oral health-related quality of life: Findings from a cross-sectional survey. BMC Oral Health. 2020;20(1):1-9. doi: 10.1186/s12903-020-01183-7
- Thomson WM, Ibrahim H, Lyons KM, Foster Page LA, Hanlin SM. Personality, xerostomia and OHRQoL among 35–54-year-olds. Biomater Investig Dent. 2019;77(2):114-118. Doi: 10.1080/00016357.2018.1510138
- Peralta-Mamani M, da Silva BM, da Silva Pinto AC, Rubira-Bullen IR, Honório HM, Rubira CM, et al. Low-level laser therapy dosimetry most used for oral mucositis due to radiotherapy for head and neck cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2019;138:14-23. doi: 10.1016/j.critrevonc.2019.03.009
- Lončar B, Mravak Stipetić M, Baričević M, Risović D. The effect of low-level laser therapy on salivary glands in patients with xerostomia. Photomed Laser Surg. 2011;29(3):171-175. doi: 10.1089/pho.2010.2792
- Gonnelli FA, Palma LF, Giordani AJ, Deboni AL, Dias RS, Segreto RA, et al. Low-level laser therapy for the prevention of low salivary flow rate after radiotherapy and chemotherapy in patients with head and neck cancer. Radiol Bras. 2016;49:86-91. doi: 10.1590/0100-3984.2014.0144
- do Nascimento ML, de Farias AB, Carvalho AT, de Albuquerque RF, Ribeiro LN, Leão JC, Silva IH. Impact of xerostomia on the quality of life of patients submitted to head and neck radiotherapy. Med Oral Patol Oral Cir Bucal. 2019; 24(6): e770-e775. doi: 10.4317/medoral.23131
- Louzeiro GC, da Silveira Teixeira D, Cherubini K, de Figueiredo MA, Salum FG. Does laser photobiomodulation prevent hyposalivation in patients undergoing head and neck radiotherapy? A systematic review and meta-analysis of controlled trials. Crit Rev Oncol Hematol. 2020;156:1-13. doi: 10.1016/j.critrevonc.2020.103115
- Yue J, Zhuo S, Zhang H, Liu X, Zhang W. Long-term quality of life measured by the University of Washington QoL questionnaire (version 4) in patients with oral cancer treated with or without reconstruction with a microvascular free flap. Br J Oral Maxillofac Surg. 2018;56(6):475-481. doi: 10.1016/j.bjoms.2017.12.017
- Rogers SN, Laher SH, Overend L, Lowe D. Importance-rating using the University of Washington quality of life questionnaire in patients treated by primary surgery for oral and oro-pharyngeal cancer. J Craniomaxillofac Surg. 2002;30(2):125-132. doi: 10.1054/jcms.2001.0273
- Michaelsen SH, Grønhøj C, Michaelsen JH, Friborg J, von Buchwald C. Quality of life in survivors of oropharyngeal cancer: a systematic review and meta-analysis of 1366 patients. Eur J Cancer. 2017;78:91-102. doi: 10.1016/j.ejca.2017.03.006
- Ganesan S, Thulasingam M, Gunaseela K, Kalaiarasi R, Penumadu P, Ravichandran S, et al. Validity and reliability of tamil translated university of washington quality of life questionnaire for head and neck cancers. Asian Pac J Cancer Prev. 2019; 20(12): 3649-3654. doi: 10.31557/APJCP.2019.20.12.3649
- Terlević Dabić D, Jurišić S, Vučićević Boras V, Gabrić D, Bago I, Vrdoljak DV. The effectiveness of low-level laser therapy in patients with drug-induced hyposalivation: a pilot study. Photomed Laser Surg. 2016;34(9):389-393. doi: 10.1089/pho.2016.4109
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
