By Aleena Ehsan1, Rimsha Sarki1, Sumbul Sohail2
AFFLIATIONS:
- Student, Ziauddin University, Karachi, Pakistan.
- Department of Obstetrics and Gynecology, Dr. Ziauddin Hospitals, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-2/014
ORCID iD: 0000-0001-7172-4661
How to cite: Ehsan A, Sarki R, Sohail S. An Atypical Presentation of Spontaneous Infarction of Uterus and Appendages. Pak J Med Dent. 2022;11(2): 91-94. doi: 10.36283/PJMD11-2/014
Spontaneous infarction of the uterus is an extremely rare condition with unknown etiology. Uterine fibroids are benign mesenchymal tumors and sometimes infarction can occur after uterine artery embolization or torsion in the fibroid. We report a delayed and neglected case of uterine fibroid, which caused spontaneous infarction of the whole uterus and its appendages in a 39-year-old unmarried woman. She was presented with severe pallor and dyspnea for which she was kept in the intensive care unit to stabilize her condition. The patient had a history of an abdominal mass for 10 years which was first diagnosed as fibroid of 7cm. The patient was planned for laparotomy, bilateral salpingo-oophorectomy, total abdominal hysterectomy and omentectomy. The intra-operative finding showed a huge infarcted uterine mass with congested and massively necrosed ovaries and tubes. Histopathological examination reported polyp presence in hemorrhagic infarction. Sections from mass, tubes and ovaries showed extensive hemorrhagic infarction with congested vessels. The patient was discharged satisfactorily with no post-operative complications.
Keywords: Infarction; Uterus; Leiomyoma.
Spontaneous rupture of degenerated leiomyoma is a rare consequence in peri-menopausal life1. Infarction of leiomyoma is common in high-intensity focused ultrasound and uterine artery embolization. In the present case, the patient underwent no such procedure. This was a rare case of spontaneous infarction including the whole uterus and adnexa and could be because of heavy menstrual blood loss. Leiomyoma of the uterus arises from smooth muscles and is the most common benign tumor. On enlargement leiomyoma, outgrow their blood supplies, leading to inflammatory reactions and ischemic changes giving rise to several kinds of degeneration2.
A 39-year-old unmarried woman was brought to an emergency on 5th July 2021 with severe pallor and dyspnoea. The patient’s sister gave a history of severe back pain radiating to the groin 3 days ago which was reported as a right kidney stone for which she was satisfactorily treated and discharged. She remained dyspnoeic and severely pallor and was referred to a tertiary care hospital from a small city for treatment of clinical symptoms where she was kept in ICU and managed by a multidisciplinary team to stabilize her condition.
On complete blood count haemoglobin was 3.4g/dl, total leucocyte count was 20×10^9/L and C-reactive protein was >192mg/l for which piperacillin Tazobactam was prescribed. She has transfused 2 units of packed cell volume. After transfusions with packed cells and iron, infusion hemoglobin was raised to 10.9g/dl, TLC was 13.8g/dl while platelets were 314×10^9/L. Chest X-ray revealed neutrophilic exudative lung effusion and CT chest showed right-sided loculated effusion and was treated as lower respiratory tract infection.
The patient’s menarche was at the age of 12 since her menarche, cycles were of abnormal uterine bleeding pattern, which was heavy. She had an abdominal mass for the last 10 years, which was first diagnosed as fibroid and at that time measured around 7cm. Due to prolonged delay in referral, mass gradually increased in size with a rapid increase since last year. She also had a family history of fibroids in her mother and sister. On per-abdominal examination, soft non-tender 32-34 weeks palpable mass reaching up to xiphisternum was dull on percussion with no shifting dullness. CT reported pelvic mass extending up to xiphisternum, which was inseparable from the left ovary and uterine fundus, measuring 25cm in transverse diameter. Omental fats were stranded and suggestive of the possible spread of disease. CT suggested a left ovarian neoplastic lesion. Tumour marker estimations showed normal CA-125.
The patient was planned for laparotomy+ bilateral salpingoophorectomy+ total abdominal hysterectomy+ omentectomy. Intraoperative findings were consistent with a huge mass arising from the pelvis up to the xiphisternum not separated from the uterus. The whole mass with ovaries and tubes looked completely gangrenous as shown in Figure 1 (A, B). Ovaries were enlarged, congested and blackish-grey in colour. Mass was mobile except few fibrous strands that were attached posteriorly to the sigmoid colon and separated easily. No ascites were present and 10 ml of blood-stained fluid was sent for cytology and DR. Uterovesical and parietal peritoneum was found congested and edematous. The estimated blood loss was 200ml. Rectus was closed with vicryl-polydioxanone suture loop while skin with staples. The specimen measured 24x20x11 cm and weighed 5.405 kg and was sent for histopathology and rest of the surgery was uneventful.
Histopathological examination showed mass arising from uterus other than mass there was a polyp as well. Sections of polyp showed haemorrhagic infarction with numerous thick-walled ectatic vessels and a few irregular dilated glands. Lining epithelium was detached and shedding due to poor fixation. Sections from mass and both ovaries showed extensive hemorrhagic infarction with congested and dilated vessels. Patchy viable areas showed sheets and fascicles of spindle cells with uniform round to oval nuclei, moderate eosinophilic cytoplasm and vague cell borders. No marked atypia or significantly raised mitosis was seen.
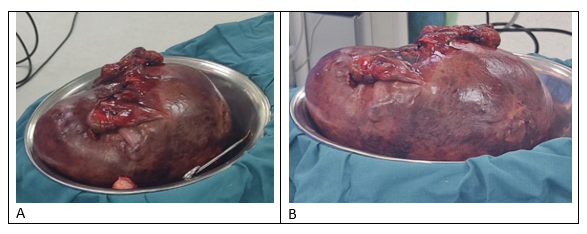
Figure 1 (A, B): Showing fresh operative specimen of uterus containing infarcted fibroid with ischemic ovaries and fallopian tubes. The specimen measured 24x20x11 cm and weighed 5.405 kg.
Uterine leiomyoma has varying rates of growth that reduce with the age along with a decline in leiomyoma-related symptoms. Moreover, spontaneous rupture of leiomyoma is exceedingly unusual. Spontaneous infarction may also occur in leiomyoma. Infarction of myoma could be because of high intensity focused ultrasound and uterine artery embolization which demonstrates enlarging mass on post-procedure MRI. Tumors may be liquefied forming cystic cavities containing gelatinous material or clear liquid after infarction. However, spontaneous infarction of the uterus, ovaries and tubes had not been reported yet. Typical cases of leiomyoma are simple to distinguish radiologically. However, uterine leiomyoma modified by degenerative changes could be incorrectly diagnosed. Different modalities such as ultrasonography, MRI and computed tomography may be helpful to diagnose and isolate a leiomyoma. On Ultrasonography, leiomyoma was characterized by heterogeneous or homogeneous hypoechoic masses.
Leiomyoma may degenerate in various patterns. Most common is hyaline degeneration, which demonstrates T2 hypointensity and diminished enhancement. Myxoid and cystic degeneration show the internal area of T2 hyperintensity and lack of contrast enhancement1. On enlargement leiomyoma can outgo their blood supplies, producing a series of ischemic changes and inflammatory responses resulting in different types of degeneration, The foremost differential diagnosis of huge cystic mass with irregular septae and solid components filling pelvis is ovarian malignancy. This can be eliminated by visualizing normal ovaries or continuity of mass with uterus upon imaging. Elevated tumor marker and absence of ascites may support diagnosis for leiomyoma. The ovarian vascular pedicle sign observed on computed tomography could be an alternative way to ensure the ovarian origin of pelvic mass and for distinguishing the mass from sub-serosal leiomyoma. Pedunculated sub-serosal leiomyoma can compromise its blood supply and can be incorporated into the pathogenesis of cystic degeneration. Uterine fibroid can imitate an ovarian cyst, endometrioma, or abscess.
There are some case reports of degenerative fibroids, which are mimicked as ovarian neoplasia. Clinical symptoms, labs and other investigations mimicked ovarian neoplasia and diagnoses were made intraoperatively. In the present case too, it posed as an ovarian neoplasm both clinically and radiologically. However, it turned out to be a case of huge spontaneously infarcted uterine leiomyoma. Prabhu et al. reported a case in which ultrasonographic features aided the diagnosis of ovarian neoplasia however, MRI supported the preoperative diagnosis of cystic degeneration of fibroids. MRI should be done in all cases where the masses are huge cystic and appendages are not visualized2. Sometimes, fibroids may adhere to their adjacent structures like the omentum, broad ligament, develop an additional blood supply and lose their actual connection to the uterus. Clinically, these lesions may present as extrauterine pelvic masses compressing the urethra, ureter or neck of the bladder developing symptoms of different degrees of urinary outflow obstruction or secondary hydroureteronephrosis. MRI is a noninvasive technique having better sensitivity and specificity as compared to ultrasound in analyzing leiomyoma with uncommon manifestations3.
Uterine leiomyoma can even be fatal, as it could lead to severe pulmonary hypertension and respiratory failure making an emergency surgery necessary. Leiomyoma of the uterus are common benign tumors in adult females, but rare in adolescents. Abnormal bleeding as menorrhagia, dysmenorrhea, and enlargement of the abdomen are the major symptoms in adolescents having giant uterine leiomyoma4. Fibroids have unremarkable potential to grow to an incredibly extreme size before debilitating the patient or producing marked clinical symptoms. Giant uterine leiomyoma is atypical benign neoplasms and usually are those weighing more than 11.4 kg or having a diameter, which is more than 17 cm or dimension 33x28x22 cm. The largest uterine fibroid ever reported weighed 63.3 kg, which was removed postmortem in the year 1888. On the other hand, the largest fibroid ever removed from a patient who survived the surgical technique weighed around 45.4 kg.
Giant uterine fibroids frequently cause abnormal periods and produce pressure effects on the urinary bladder, ureters, lungs and other surrounding organs leading to further complications like lower-limb thrombosis as well as renal and respiratory failure. Treatment options include expectant management, medical management, surgery, interventional procedures like uterine artery embolization and ablative procedures. Expectant management with observation is done in cases of women presenting with small and large asymptomatic fibroids, since rarely uterine leiomyoma may undergo sarcomatous transformation. The removal of giant uterine leiomyoma by total abdominal hysterectomy with or without salpingo-oophorectomy is a traditional treatment of choice. Vaginal and laparoscopic hysterectomies are associated with fewer postoperative complications and quicker recovery of patients as compared to laparotomy or abdominal approach5. Giant uterine fibroids can result in causing pain, pressure symptoms and AUB. These fibroids can also impinge reproduction by causing infertility, premature labor or miscarriage6.
Uterine fibroids or leiomyoma are composed of smooth muscle encircled by pseudocapsule. Ultrasonography is the most preferred imaging technique as it is non-invasive and cost-effective. CT scan cannot differentiate between healthy myometrium and leiomyoma, except that they are necrotic or calcified. MRI can interpret the normal anatomy of ovaries and the uterus clearly but its use is limited due to its cost7. MRI is very helpful in determining anatomical characteristics such as the locations, sizes, and numbers of pelvic masses.
In addition, MRI may give diagnostic information supporting the preoperative assumption of leiomyoma; nevertheless, it is not entirely correct8. Based on the location of the fibroid, leiomyoma is classified as submucosal and subserosal. The latter may be pedunculated and mimics as an ovarian neoplasm. On enlargement, leiomyoma can outgrow their blood supply, resulting in different kinds of degeneration such as hyaline, cystic, red or myxoid degeneration and dystrophic calcification or infarction. The most common pattern of degeneration is hyalinization, which occurs in about 60% of the cases. Cystic degeneration is up to 4%. Large fibroids may also cause constipation, increase urinary frequency and increase menstrual bleeding9. Red degeneration which is a hemorrhagic infarction of the uterine fibroid, is a well-recognized complication, particularly in pregnancy. The occurrence of red degeneration is in 8% of tumors complicating pregnancy, whereas its prevalence is around 3% among all uterine fibroids10. Incidence for sarcomas in patients treated for leiomyoma is about 0.23 %, with leiomyosarcoma being rarer approximated to be in between 0.13 and 0.29 % 11.
Although fibroids are usually benign and are not life-threatening if left untreated or neglected, they can grow into abnormally large sizes, which can lead to heavy menstrual blood loss that can result in infarction of fibroid along the whole of the uterus and appendages. Moreover, in this case, prolonged delay in treatment lead to heavy menstrual bleeding which resulted in severe pallor and critical condition of the patient. Thus, women diagnosed with fibroids should take timely treatment for this as it could preserve the uterus, ovaries and tubes by only removing the fibroid and can also prevent any life-threatening complication to occur.
The authors would like to acknowledge the Dr. Ziauddin Hospital staff for their support.
The authors declare no conflict of interest.
Consent of the patient was taken before writing the case report.
All authors contributed equally in this case report write-up.
- Huang YT, Wu RC, Chao A, Chao AS. Spontaneous rupture of infarcted leiomyoma into endometrial cavity in a perimenopausal woman. Arch Gynecol Obstet. 2017;296(3):609-611. doi: 10.1007/s00404-017-4454-1
- Prabhu JK, Samal S, Chandrasekar S, Subramani D, Rajamanickam S. A massive degenerative leiomyoma mimicking an ovarian tumor: A diagnostic dilemma. J Gynecol Surg. 2021;37(1):67-69. doi: 10.1089/gyn.2020.0118
- Rajanna DK, Pandey V, Janardhan S, Datti SN. Broad ligament fibroid mimicking as ovarian tumor on ultrasonography and computed tomography scan. J Clin Imaging Sci. 2013; 3:1-4. doi: 10.4103/2156-7514.107912
- Mülayim B. Unaware of a large leiomyoma: A case report with respect to unusual symptoms of large leiomyomas. Ann Med Surg. 2015;4(4):431-433. doi: 10.1016/j.amsu.2015.09.002
- Kalyan S, Sharma S. Giant uterine leiomyoma: a case report with literature review. Int J Reprod Contracept Obstet Gynecol. 2018;7:4779-4785. doi: 10.18203/2320-1770.ijrcog20184548
- Sambath S, Balasubramanian T. A giant pedunculated leiomyoma with cystic degeneration mimicking an ovarian malignancy. Int J Reprod Contracept Obstet Gynecol. 2016;5(1):252-255. doi: 10.18203/2320-1770.ijrcog20151638
- Bhuyar S, Sontakke B, Rajbhara PM. Degenerated fibroid–a diagnostic challenge. Int J Reprod Contracept Obstet Gynecol. 2017;6(1):292-295. doi: 10.18203/2320-1770.ijrcog20164677
- Suh DS, Kim YH, Yun KY, Lee NK, Choi KU, Kim KH, et al. An unusual case of pedunculated subserosal leiomyosarcoma of the uterus mimicking ovarian carcinoma. J Ovarian Res. 2016;9(1):1-5. doi: 10.1186/s13048-016-0212-4
- Aydin C, Eriş S, Yalçin Y, Selim HŞ. A giant cystic leiomyoma mimicking an ovarian malignancy. Int J Surg Case Rep. 2013;4(11):1010-1012. doi: 10.1016/j.ijscr.2013.08.018
- Han SC, Kim MD, Jung DC, Lee M, Lee MS, Park SI, et al. Degeneration of leiomyoma in patients referred for uterine fibroid embolization: incidence, imaging features and clinical characteristics. Yonsei Med J. 2013;54(1):215-219. doi: 10.3349/ymj.2013.54.1.215
- Bharambe BM, Deshpande KA, Surase SG, Ajmera AP. Malignant transformation of leiomyoma of uterus to leiomyosarcoma with metastasis to ovary. J Obstet Gynaecol India. 2014;64(1):68-69. doi: 10.1007/s13224-012-0202-4
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
