By Hareem Gohar1, Faisal Iqbal Afridi2, Madeeha Fatima3, Ambreen Fatima1, Nayab Afzal4, Fatima Fasih1
AFFLIATIONS:
- Department of Microbiology, Dow University of Health Sciences, OJHA Campus, Karachi, Pakistan.
- Department of Microbiology, Dr. Ziauddin University Hospital, North Nazimabad Campus, Karachi, Pakistan.
- Indus Hospital and Health Network, Karachi, Pakistan.
- Department of Chemical Pathology, National Medical Centre, Karachi, Pakistan.
Background: Urinary tract infections (UTI) considered, as the most frequently diagnosed infections constitute Escherichia coli (E. coli) as the most common etiological agents isolated from urinary cultures. Fosfomycin is becoming the best treatment option for UTI because of its rapid absorption, good concentration in urine. The present study aimed to determine and compare the susceptibility of Fosfomycin, presented as a favorable choice against E. coli producing extended spectrum beta-lactamase (ESBL) in urinary cultures of patients.
Methods: This cross sectional study with non-probability consecutive sampling was held at Ziauddin University Hospital Microbiology Laboratory. A total of 222 urinary isolates of in and out patients yielding growth of ESBL positive E. coli were identified using standard microbiological technique. Susceptibility testing of antimicrobials was accomplished according to Clinical Laboratory Standard Institute (CLSI) guidelines. Detection of ESBL was done by double disk diffusion technique. Independent sample t-test was used to compare mean ages and Chi-squared test for the ESBL positivity in various age groups. A p-value of less than 0.05 was considered as statistically significant.
Results: The mean age of the patients was 56.68±21.18 years. There were 59(26.58%) male and 163(73.42%) female. The sensitivity of ESBL producing E. coli to Fosfomycin was 94.59 % (210/222) which was much higher as compared to other antimicrobials, Meropenem (89%), Amikacin (83%) and Nitrofurantoin (78%). There was no statistically significant variance among the age groups with respect to fosfomycin susceptibility (p=0.601).
Conclusion: Fosfomycin have high antimicrobial activity against ESBL positive E. coli in urinary samples. It could be a good treatment choice for urinary tract infections.
Keywords: Urinary Tract Infections; Fosfomycin; Escherichia coli; Beta-Lactamases.
The most frequent infections found in a hospital setting are urinary tract infections (UTIs). It can influence all age groups but because of many clinical variables, including physiological variations, hormonal impacts, and behavioral habits, women are more susceptible than men1. Escherichia coli (E. coli) is the most widespread UTI causative microorganism. It is assessed to account for more than 50% of both uncomplicated and complicated UTI 2. Fluoroquinolones, penicillins, cephalosporins, co–trimoxazole, and nitrofurantoin are the common antibiotics used to treat these infections. The appearance of multidrug resistant organisms due to unreasonable use of antimicrobials has made UTI difficult to manage3.
coli producing enzymes extended spectrum beta-lactamases (ESBLs) has appeared as a significant reason for UTI. ESBLs are the enzymes, which hydrolyze all penicillins, cephalosporins and monobactams and cause cross-resistance to co-trimoxazole, fluoroquinolones and amino glycosides, all of which are commonly favored in UTI management4.
Several studies showed the increasing ubiquity of ESBL positive E. coli in both community and hospital settings. A study held in Pakistan on urine samples showed 40% ESBL positive E. coli 5. The increasing resistance pattern of ESBL producing E. coli to other classes of antibiotics has led to extended use of carbapenems that further contributes to selection pressure and spread to carbapenem resistant Enterobacteriaceae (CRE) 6. Therefore, alternatives to carbapenems for the treatment of ESBL-producing Enterobacteriaceae are urgently required.
Fosfomycin has been regarded for many years as an old broad-spectrum bactericidal antibiotic. Recently, it has gained prominence due to growing resistance to conventionally used antibiotics. It is a derivative of phosphonic acid and inhibits the initial step in the production of the cell wall of both Gram-positive and Gram-negative bacteria. It inhibits the synthesis of peptidoglycan by blocking formation of N-acetyl muramic acid from N-acetyl glucosamine. It also shows synergism with other antibiotics7. Fosfomycin has unique pharmacological features making it attractive for the management of UTI. These include rapid oral bioavailability, less adverse effects, biofilm activity, and its efficacy against many multi-drug resistant strains including ESBL and AmpC-producing Enterobacteriaceae 8.
It shows very low resistance worldwide among E. coli. In one study conducted in 2015 in Pakistan, the sensitivity of ESBL producing E. coli to fosfomycin was 94.5% 9. Fosfomycin has been shown to exhibit synergy with meropenem, colistin, gentamicin and plazomicin against several strains of E. coli 10.
This study assessed the effectiveness of fosfomycin in comparison with other antimicrobials against ESBL positive E. coli in UTIs and raise awareness in the use of fosfomycin in general practice as it is cheaper, easily available and has fewer side effects. Through this study, we will also be able to extract data that will help clinicians to decide on better empirical options.
The study was held at the Microbiology section, Ziauddin Medical University Hospital, Karachi from June 1, 2017 to February 1, 2018. Written approval was taken from the institutional ethical committee (ERC Reference Code: 0160617 HZMB). All E. coli identified from urine samples of inpatients and outpatients were incorporated in the study and studied for Fosfomycin susceptibility along with other common antimicrobials used for UTIs. Urine cultures yielding growth other than E. coli were excluded from the study. Either informed consent was taken from the patient or any other patient’s relative. A total of 222 urinary samples were collected of inpatients and outpatients. All urinary samples were inoculated on Cystine Lactose Electrolyte Deficient (CLED) medium according to standard microbiological protocols and incubated at 37°C in ambient air for 24 hours. Plates were noticed for any bacterial growth of colonies and gram stain was performed. To identify the suspected bacterial colonies of Gram negative rods, few biochemical tests were performed like Oxidase test, Triple sugar iron (TSI), Sulphide Indole motility (SIM), Citrate utilization and Urease tests. Analytical profile index 20 Enterobacteriaceae (API 20E) was used to further confirm the identification11. Antimicrobial susceptibility testing of isolated organisms was achieved on Mueller Hinton agar (MHA) (Oxoid Limited, England) by disk diffusion method according to CLSI standards12. After 24-hours incubation, isolated colonies were suspended in normal saline to make a suspension of 0.5 McFarland turbidity. The bacterial lawns used sterile swabs over the MHA plates. The detection of ESBL was achieved by placing discs containing ceftazidime-clavulanate (30+10µg) and ceftazidime (30µg) 10mm apart. A ≥ 5mm increase in zone diameter for ceftazidime-clavulanate the zone diameter of the ceftazidime alone is considered ESBL positive. All ESBL positive isolates were now tested with a disc of 200µg of Fosfomycin along with other common antimicrobials to assess the susceptibility pattern against ESBL positive E. coli and the growth inhibition zone was estimated according to Clinical and Laboratory Standards Institute (CLSI) criteria13. Using Statistical Package for Social Sciences (SPSS) version-20 data analysis was carried out. Frequency and percentages were computed for presentation of all categorical variables like microorganisms, gender and ESBL positivity. For quantitative variables like patient’s age, mean values and standard deviation were measured. Test of significance was calculated using independent sample t-test to compare mean ages and chi-square test for the ESBL positivity in various age groups. A p-value of less than 0.05 was measured as statistically significant.
A total of 222 urinary isolates of in and out patients with yielding growth of ESBL positive E. coli were included. There was no statistically significant variance among the age groups for fosfomycin susceptibility (p=0.601) as shown in Figure 1.
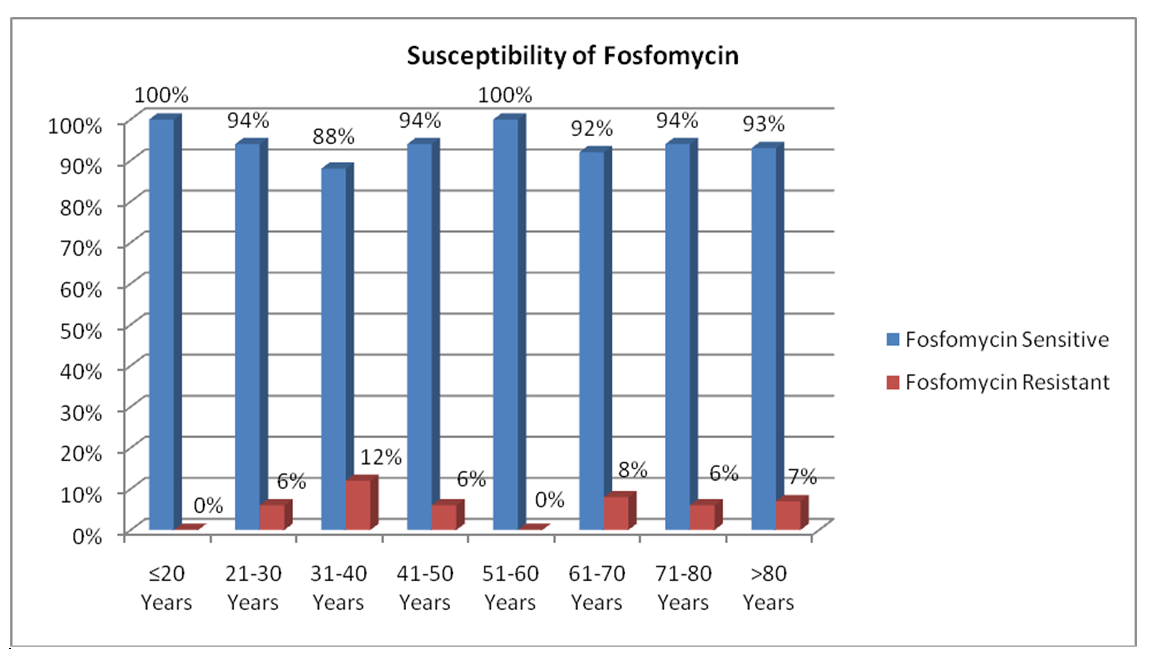
Chi-squared= 5.48 p=0.601
Figure 1: Susceptibility of fosfomycin against Escherichia coli producing extended spectrum beta-lactamase by age groups.
The selective culture medium and colonies of E. coli isolated on CLED medium are shown in Figure 2.
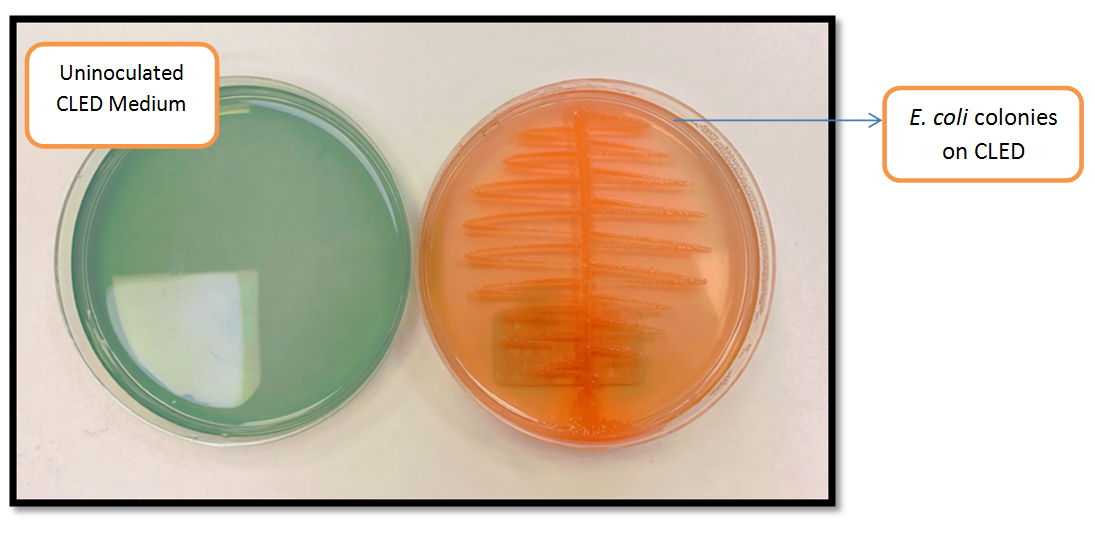
Figure 2: Selective culture medium (CLED) for detection and isolation of E. coli in urinary isolates.
There were 59(26.58%) male and 163(73.42%) female. Out of 222 cases, only 73(32.68%) were taking other antibiotics before drug fosfomycin. In total E. coli isolates, most of the patients 51(23.9%) reporting UTIs were between 61-70 years age. E. coli showed very good susceptibility against fosfomycin (94.59%), meropenem (89%), amikacin (83%) and nitrofurantoin (78%) but susceptibility against other common antibiotics like co-trimoxazole (35%) and ciprofloxacin (25%) were lesser. Table 1 represents susceptibility to various antibiotics tested against ESBL positive E. coli.
Table 1: The comparison of overall antibiotic susceptibility pattern of ESBL positive E. coli.
| Antibiotic | Sensitive | Resistant |
| Ampicillin | 33(15%) | 189(85%) |
| Amoxicillin-clavulanate | 122 (55%) | 100 (45%) |
| Amikacin | 185 (83%) | 37 (17%) |
| Cefixime | 39 (18%) | 183 (82%) |
| Ceftriaxone | 47 (21%) | 175 (79%) |
| Ciprofloxacin | 55 (25%) | 167 (75%) |
| Fosfomycin | 210 (94.59%) | 12 (5.41) |
| Gentamicin | 118 (53%) | 104 (47%) |
| Levofloxacin | 62 (28%) | 160 (72%) |
| Meropenem | 198 (89%) | 24 (21%) |
| Nitrofurantoin | 173 (78%) | 49 (22%) |
| Piperacillin-Tazobactam | 115 (52%) | 107(48%) |
| Sulfamethoxazole-Trimethoprim | 78 (35%) | 144 (65) |
| Tobramycin | 100 (45%) | 122 (55%) |
There was also no difference among groups that had taken prior antibiotics (p=0.219) as shown in Table 2.
Table 2: Susceptibility of fosfomycin against Escherichia coli producing extended spectrum beta-lactamase by gender and by prior antibiotic.
| Gender | Fosfomycin | Total | Prior Antibiotic | Fosfomycin |
Total |
||
| Sensitive | Resistant | Sensitive | Resistant | ||||
| Male | 56(94.9%) | 3(5.1%) | 59 | Yes |
71(97.3%) |
2(2.7%) |
73 |
| Female | 154(94.5%) | 9(5.5%) | 163 | No |
139(93.3%) |
10(6.7%) |
149
|
| p-Value | p=0.899 | p-Value | p=0.219 | ||||
| Chi square | 0.016 | Chi square | 1.51 | ||||
This study revealed a high degree of E. coli resistance to various antibiotics. In this study, E. coli showed the highest sensitivity to Fosfomycin 94.59% followed by Meropenem (89%), Amikacin (83%) and nitrofurantoin (78%). The most common causative agent for both uncomplicated and complicated UTIs is uropathogenic E. coli (UPEC)12. It is considered the predominant pathogen in both community and hospital. One study conducted in Saudi Arabia on 116 urinary isolates showed E. coli as the most common causative agent (78.45%).14Antibiotic agents such as beta-lactams, co-trimoxazole and fluoroquinolones were used for the treatment of UTI15,16.
Furthermore, the rise of uropathogens, mainly E. coli producing extended-spectrum beta-lactamases (ESBLs) is troublesome, confers resistance to third and fourth generation cephalosporins, monobactams, and causes cross-resistance to other antimicrobial classes such as fluoroquinolones, co-trimoxazole, tetracyclines and aminoglycosides17. This has led to the increased use of carbapenems, which are considered as the treatment of choice for ESBLs18. This furthers led to the emergence of carbapenem resistant Enterobacteriaceae (CRE) which further made the treatment difficult. The current study which is held to determine the susceptibility of Fosfomycin and other antimicrobials against Extended Spectrum Beta-Lactamase positive E .coli in urinary isolates of patients, clinical samples of urine of 222 patients, aged between 20-80 years, with yielding growth of ESBL producing E. coli were included. These findings coincided with other studies wherein E. coli showed the highest sensitivity to amikacin, fosfomycin, meropenem and nitrofurantoin3,19.
Interestingly the fluoroquinolones group showed only 25-28% sensitivity, which further declines its use. The sensitivity pattern of other oral antibiotics was amoxicillin-clavulanate (55%), sulfamethoxazole-trimethoprim (35%) and cefixime (18%) which explains the failure of response to treatment on empirical basis. Similar susceptibility pattern were found in study conducted in Pakistan3. The highest resistance was with ampicillin (15%) which is also seen in other studies20. This high resistance pattern of these antimicrobials in our setup could be due to over the counter use of these antibiotics and incomplete treatment. The presence of resistant pathogens has restricted the availability of alternative antibiotic options. Fosfomycin has shown well in vitro effectiveness against extended spectrum β-lactamase positive Gram-negative bacteria when compared to other first line antibiotics. This is consistent with the findings of studies carried in Pakistan21,22. Worldwide, many studies were conducted with similar results, which showed very low resistance to Fosfomycin23,24. The sensitivity of fosfomycin was high in all age groups, all gender, and those who used other antibiotic (94.59%, 210/222). Cho et al. in their retrospective analysis on 217 ESBL positive E. coli isolate and 60 ESBL-Klebsiella Pneumoniae isolates reported fosfomycin showing higher activity against ESBL E. coli isolates i.e. 94.9% 25. Another study conducted for one year showed fosfomycin with higher susceptibility pattern against the ESBL-producing isolates of the most common Enterobacteriaceae than the other antibiotics26. In this study, there were 26.58% male and 73.42% female which showed that overall there was a female preponderance of urinary tract infection occurrence (the male to female ratio was 1:3). Women are more susceptible to urinary tract infection due to their shorter urethra and the area around the urethral opening is inhabited heavily with potential pathogens. In terms of age, it was found that E. coli was more frequently isolated from age groups of 61–70 (23.9%) and 71–80 (20.7%) years old. These patients are at increased risk of developing chronic UTI so they must be managed with a better antimicrobial with fewer side effects. These outcomes agree with previous studies, which showed the incidence of UTI low in middle age but high in older adults with frequency more common in adult women than men27.
The current study might help in the empirical selection of antibiotic, which should be based on the knowledge of the local frequency of bacterial organisms, and antibiotic susceptibility patterns according to geographical location instead of international recommendations. Fosfomycin is a good option for complicated and uncomplicated UTIs as it is available in both oral and intravenous formulations although resistance to this drug has been documented during treatment28. In our setup, we found the sensitivity of ESBL producing E. coli to fosfomycin was 94.59% (210/222) which is very much higher compared to other oral options. This high sensitivity of Fosfomycin has backed up its use. It should be considered as a favorable alternative for the management of ESBL-positive E. coli strains infections due to its high efficacy, better tissue penetration, and favorable safety profile including pregnancy patients and low impact on promoting antibiotic resistance29,30. Further research is required on the use of fosfomycin for complicated urinary tract infections and non-urinary tract infections, which has not been widely assessed in our setup. The data presented in this study shows that Fosfomycin proved to be the most effective antimicrobial agent when compared with other antibiotics against ESBL positive E. coli in urinary isolates.
Fosfomycin showed more than 90% sensitivity against ESBL positive E. coli in urinary cultures, which at the same time show high rates of antimicrobial resistance to the conventionally used antibiotics for UTIs. Therefore, Fosfomycin is being reconsidered for use against multiple drug resistance (MDR) pathogens including ESBLs due to its low resistance rate, safety profile and oral administration. The results of this study might help to rationalize the management of urinary tract infections by fosfomycin in our country.
The authors would like to acknowledge the Ziauddin Laboratory staff and the supervisor for their immense contribution.
There is no conflict of interest to be declared.
The study approval was obtained from the Ethics Review Committee of the Ziauddin University Hospital (ERC Reference Code: 0160617 HZMB).
Verbal and written signed consents were taken from the patients.
HG conceived the idea, collected data and did manuscript writing. MF did the editing and literature review. NA performed statistics and critical review. AF and FF reviewed the manuscript. All the authors read and approved the submitted manuscript. FIA did the final approval.
- Ganesh R, Shrestha D, Bhattachan B, Rai G. Epidemiology of urinary tract infection and antimicrobial resistance in a pediatric hospital in Nepal. BMC Infect Dis. 2019;19(1):1-5.
- Karlowsky JA, Adam HJ, Baxter MR, Denisuik AJ, Lagacé-Wiens PR, Walkty AJ, et al. In vitro activity of sulopenem, an oral penem, against urinary isolates of Escherichia coli. AntimicrobAgents Chemother. 2018;63(1):1-7.
- Jadoon SA, Ahmed A, Irshad R. Spectrum of bacterial culture and drug sensitivity vs resistance in uncomplicated urinary tract infection. J Ayub Med Coll Abbottabad. 2018;30(3):432-438.
- Kim YH, Yang EM, Kim CJ. Urinary tract infection caused by community-acquired extended-spectrum β-lactamase-producing bacteria in infants. J Pediatr. 2017;93(3):260-266.
- Ali I, Rafaque Z, Ahmed S, Malik S, Dasti JI. Prevalence of multi-drug resistant uropathogenic Escherichia coli in Potohar region of Pakistan. Asian Pac J Trop Biomed. 2016;6(1):60-66.
- Rosso-Fernández C, Sojo-Dorado J, Barriga A, Lavín-Alconero L, Palacios Z, López-Hernández I, et al. Fosfomycin versus meropenem in bacteraemic urinary tract infections caused by extended-spectrum β-lactamase-producing Escherichia coli (FOREST): study protocol for an investigator-driven randomised controlled trial. BMJ Open. 2015;5(3):1-10.
- Dijkmans AC, Zacarías NV, Burggraaf J, Mouton JW, Wilms EB, Van Nieuwkoop C, et al. Fosfomycin: pharmacological, clinical and future perspectives. Antibiotics. 2017;6(4):1-17.
- Matthews PC, Barrett LK, Warren S, Stoesser N, Snelling M, Scarborough M, et al. Oral fosfomycin for treatment of urinary tract infection: a retrospective cohort study. BMC Infect Dis. 2016;16(1):1-11.
- Ahmed I, Sajed M, Sultan A, Murtaza I, Yousaf S, Maqsood B, et al. The erratic antibiotic susceptibility patterns of bacterial pathogens causing urinary tract infections. EXCLI J. 2015; 14: 916-925.
- López-Montesinos I, Horcajada JP. Oral and intravenous fosfomycin in complicated urinary tract infections. Rev Esp Quimioter. 2019; 32(Suppl 1): 37-44.
- Procop GW, Church DL, Hall GS, Janda WM. Koneman’s color atlas and textbook of diagnostic microbiology. 7th Jones & Bartlett Publishers; 2020. 67 p.
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269-284.
- Clinical and Laboratory Standards Institute. 2015. M100-S25: Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Fifth Informational Supplement; M100-S25. Wayne, PA: Clinical and Laboratory Standards Institute; 2015.
- Al-Mijalli SH. Bacterial uropathogens in urinary tract infection and antibiotic susceptibility pattern in Riyadh Hospital, Saudi Arabia. Cell Mol Med. 2017;3(1):1-6.
- Novelli A, Rosi E. Pharmacological properties of oral antibiotics for the treatment of uncomplicated urinary tract infections. J Chemother. 2017;29(sup1):10-18.
- Delpech G, Allende NG, Lissarrague S, Sparo M. Antimicrobial resistance of uropathogenic Escherichia coli from elderly patients at a general hospital, Argentina. Open Infect Dis J. 2018;10(1):79-87.
- Yeganeh-Sefidan F, Ghotaslou R, Akhi MT, Sadeghi MR, Mohammadzadeh-Asl Y, Baghi HB. Fosfomycin, interesting alternative drug for treatment of urinary tract infections created by multiple drug resistant and extended spectrum β-lactamase producing strains. Iran J Microbiol. 2016; 8(2): 125-131.
- Critchley IA, Cotroneo N, Pucci MJ, Mendes R. The burden of antimicrobial resistance among urinary tract isolates of Escherichia coli in the United States in 2017. PLoS One. 2019;14(12):1-11.
- Bano S, Tunio SA, Memon AA, Detho H, Bano R, Kumari K. Evaluation of antibiotic susceptibility patterns of uropathogens circulating in Hyderabad, Pakistan. Khyber Med Univ J. 2014;6(3):110-115.
- Alanazi MQ, Alqahtani FY, Aleanizy FS. An evaluation of coli in urinary tract infection in emergency department at KAMC in Riyadh, Saudi Arabia: retrospective study. Ann Clin Microbiol Antimicrob. 2018;17(1):1-7.
- Kidwai SS, Nageen A, Ghaznavi S, Bashir F, Ara J. Antibiotic susceptibility in commonly isolated pathogens from urinary tract infection in a cohort of subjects from low socioeconomic strata. Pak J Med Sci. 2017; 33(2): 254-259.
- Shah M, Wali N. Fosfomycin versus nitrofurantoin efficacy against multi-drug resistant gram negative urinary pathogens. J Rawalpindi Med Coll. 2016;20(4):265-268.
- Koshesh M, Mansouri S, Hashemizadeh Z, Kalantar-Neyestanaki D. Identification of extended-spectrum β-lactamase genes and ampc-β-lactamase in clinical isolates of escherichia coli recovered from patients with urinary tract infections in Kerman, Iran. Arch Pediatr Infect Dis. 2017;5(2):1-6.
- Fajfr M, Louda M, Paterová P, Ryšková L, Pacovský J, Košina J, et al. The susceptibility to fosfomycin of Gram-negative bacteria isolates from urinary tract infection in the Czech Republic: data from a unicentric study. BMC Urol. 2017;17(1):1-6.
- Cho YH, Jung SI, Chung HS, Yu HS, Hwang EC, Kim SO, et al. Antimicrobial susceptibilities of extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae in health care-associated urinary tract infection: focus on susceptibility to fosfomycin. Int Urol Nephrol. 2015;47(7):1059-1066.
- Aris P, Boroumand MA, Rahbar M, Douraghi M. The activity of fosfomycin against extended-spectrum beta-lactamase-producing isolates of Enterobacteriaceae recovered from urinary tract infections: a single-center study over a period of 12 years. Microb Drug Resist. 2018;24(5):607-612.
- Gharbi M, Drysdale JH, Lishman H, Goudie R, Molokhia M, Johnson AP, et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all-cause mortality: population based cohort study. BMJ. 2019;1-12.
- Tan CW, Chlebicki MP. Urinary tract infections in adults. Singapore Med J. 2016; 57(9): 485-490.
- Falagas ME, Vouloumanou EK, Samonis G, Vardakas KZ. Fosfomycin. Clin Microbiol Rev. 2016:1;29:321-347.
- Bielen L, Likic R. Experience with fosfomycin in the treatment of complicated urinary tract infections caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae. Ther Adv Infect Dis. 2019;6:1-11.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
