By Khalid Mustafa1, Uzma Azmatullah2, Sara Zafar3
AFFLIATIONS:
- Department of Vascular Intervention Radiology, Liaquat National Hospital, Karachi, Pakistan.
- Department of Radiology, Memon Medical Institute Hospital, Karachi, Pakistan.
- Department of Radiology, Ziauddin University Hospital, Karachi, Pakistan.
Background: Acute appendicitis, when the appendiceal lumen is obstructed, leads to development of inflammation and eventually perforation. Pre-operative identification of ruptured appendix could help determine therapy, including consideration for a non-surgical approach towards management. Although, no doubt exists in the reliability of Computed tomography (CT) in detecting acute appendicitis (AA), however, its efficiency in discriminating the non perforated appendicitis from ruptured one still needs clarification. This study aimed to establish the diagnostic accuracy, sensitivity and specificity of CT scan in acute appendicitis in terms of the presence or absence of perforation.
Methods: A cross sectional study was conducted in the Department of Radiology, Dr. Ziauddin University Hospital, Karachi, for 6 months. Patients (171) clinically suspected of appendicitis were included in this study. CT was performed with oral and intravenous contrast administration and findings were documented. The final diagnosis was based on post-appendectomy histopathological analysis.
Results: In the current study, computed tomography used for the detection of perforated appendicitis had 79.07% sensitivity, 89.06% specificity, 70.8% positive predictive value and 92.7% negative predictive value along with 86.5% accuracy, respectively. The precision of CT in the detection of ruptured appendicitis was 90.9% for female cases and 83.8% for male cases. Similarly, with respect to age, furthermore, CT precision was 85.59% for ≤ 30 years of age and 88.68% for > 30 years of age (p=0.0005).
Conclusion: The computed tomography (CT) scan is a non-invasive investigation with high precision and can be used confidently to select cases with non-perforated appendicitis for initial non-operative management.
Keywords: Perforated Appendicitis; Computed Tomography; Appendectomy.
An acutely inflamed appendix is a quite frequent cause of acute abdomen, the incidence being 33.8 cases /100,000/ year with a lifetime probability of 9% 1. More recently the incidence of AA has risen, being at an average rate of 0.5 cases /100,000/ year 1. Incidence of perforation is more marked in developing nations like Pakistan figuring to about 20% of all cases of acute appendicitis (AA) 2. It is commonly the second or third decade of one’s life when appendiceal inflammation is experienced3. Its incidence being nearly 233/100,000 population, the peak age group affected is between10 to 19 years. Data shows higher probability for men with an incidence of 8.6% in comparison to women having 6.7% incidence rate (male to female ratio 1.4:1) 4.
Identifying ruptured AA from a non-ruptured one is important when selecting an adequate therapeutic approach that defines prognosis. Post-operative sequelae are far more frequent in patients with ruptured appendicitis in contrast to non-perforated appendectomy, recorded to be 28.4% and 4.7% respectively5. A prior study documented an average 6.3 days mean hospital stay in the ruptured group and only 2.9 days in non-perforated one6. Being non-invasive, Computed tomography (CT) scan has gained significant popularity in investigating AA, contrary to invasive approaches like diagnostic laparoscopy7,8. An earlier study recorded sensitivity and specificity of 69% and 97% respectively for CT scan in identifying ruptured appendicitis9.
A retrospective review included 2283 patients who underwent CT evaluation for possible appendicitis: 516 (23 percent) had evidence of probable or definite appendicitis. Thirteen (3 percent) of these patients had improved or resolved pain and were discharged without surgery9,10. Five of the 13 patients subsequently underwent an appendectomy for a diagnosis of appendicitis after a mean of 118 days (range, 5 to 443 days). The histologic evaluation identified acute inflammation in two specimens, chronic inflammation in one, and acute and chronic inflammation in two therefore; perforation was detected in three patients.
Elbanna et al. in their study reported 20% perforation rate developing in less than 24 hours after symptom onset10. Appendicectomy rate in perforated cases of AA has declined since 1995 11. If perforation is diagnosed pre-operatively, patient management is altered, initially; percutaneous drainage is performed pursued by interval appendectomy12,13. While routine laparoscopic appendicectomy is obtained in non-perforated AA. Thus, it is crucial to identify ruptured AA pre-surgically14. Since not sufficient Pakistani data is available on this subject, we, therefore, aimed to establish CT scan precision in discriminating perforated from non-perforated appendicitis with defining its sensitivity and specificity taking histopathology as a gold standard.
A cross sectional study was carried out at Ziauddin University Hospital, Karachi, for a 6-month duration dated 01 January 2016 until 30 June 2016. After approval from the ethical review committee, informed written consent was obtained from patients referred to the department requesting CT scan abdomen with a clinical suspicion of acute appendicitis. Sampling size calculated by the statistics department considering disease prevalence from literature using the WHO software1. The total number of patients was n=171, sampling done by non-probability consecutive method.
We included suspicious cases between the ages of 15 to 50 years who had right iliac fossa pain of 12 or more hours with or without associated nausea and fever and those who were planned for surgery within 2 days of CT scan. All those patients who refused surgery, those unfit for surgery or patients with iatrogenic perforation of the appendix during surgery were excluded from this study. Computed tomography was performed on Toshiba Alexion 16 slice CT scanner. Scanning protocol included acquisition of axial helical sections before and after administration of intravenous contrast with Sagittal and coronal reconstructions at 120kVp and 220mA. At the time of scanning intravenous contrast was administered using power injector at a rate of 3 ml per sec followed by the acquisition of axial cuts at 5 mm slice thickness in porto-venous phase.
Findings obtained on CT scan including age, gender and duration of symptoms were documented in a pre-drafted Proforma and the final diagnosis was based on post-appendicectomy histopathology. Data analysis was u done by using a statistical package for social sciences (SPSS-17). Relevant descriptive statistics, frequency and percentage were computed for gender, CT scan findings and histopathology findings. Mean +/- SD for age, duration of symptoms were calculated. Sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy of perforated appendicitis on CT scan were calculated taking histopathology as a gold standard. Stratification was done to control effect modifiers like age, gender and duration of symptoms to observe the effect of these modifiers on the accuracy through chi-squared test and p<0.05 was considered statistically significant.
Patients n=171with suspected inflamed appendix were included in this study. The average patient age was 29.9 years with the age range of 15 to 50 years as presented in Table 1. Out of 171 cases, 105(61.40%) were male and 66(38.59%) females (Table 2). As per CT findings, 28.1% (48/171) cases had perforated and 71.9% (123/171) had non-perforated appendicitis while histopathology documented 25.1% (43/171) perforated and 74.9% (128/171) non-perforated appendicitis as presented in Table 1. The sensitivity, specificity, positive and negative predictive value as well as accuracy of computed tomography in the detection of perforated appendicitis (see Figure 1) was 79.07%, 89.06%, 70.8%, 92.7% and 86.5% respectively.
Table 1: Diagnostic accuracy of computed accuracy for appendicitis keeping histopathology as a gold standard.
| Clinical Findings | Perforated Appendicitis | Non-Perforated Appendicitis | CT Scan/Histopathology
n (%) |
| CT Scan | 34 (TP) | 14(FP) | 48 (28.1%) |
| Histopathology | 9 (FN) | 114 (TN) | 123 (71.9%) |
| Total n (%) | 43 (25.1%) | 128 (74.9%) | 171(100%) |
n=Total number =171, TP= True positive, FP= False positive, FN= False negative, TN= True negative.
Precision of CT in detection of ruptured appendicitis was 90.9% for female cases and 83.8% in male cases (Table 2). Similarly, with respect to age category, CT precision was 85.59% for below and equal to 30 years of age and 88.68% for above 30 years of age, also presented in Table 2.
Table 2: Stratification of diagnostic accuracy of computed tomography (CT) in acute appendicitis taking histopathology as the gold standard by age, gender and perforation.
| Variables | Number
Detected |
Sensitivity | Specificity | PPV | NPV | Diagnostic
Accuracy |
p-Value |
| Age >30 years | 53 | 83.33% | 90.24% | 71.43% | 94.87% | 88.68% | 0.0005 |
| Age < 30
Years |
118 | 77.42% | 88.5% | 70.59% | 91.67% | 85.59% | 0.0005 |
| Total Acute Appendicitis | 171 | 79.07% | 89.06% | 70.83% | 92.68% | 86.55% | 0.0005 |
| Perforated Appendicitis Males
(n =105) |
35 | 80.00% | 85.33% | 68.57% | 91.43% | 83.81% | 0.0005 |
| Perforated Appendicitis Females (n=66) | 13 | 76.92% | 94.34% | 76.9% | 94.3% | 90.91% | 0.0005 |
PPV=positive predictive value, NPP=negative predictive value

Figure 1: CT demonstrates dilated appendix with wall defect medially (arrowhead) and extraluminal air was appreciated suggesting appendiceal perforation as well.
In the present study, we found sensitivity, specificity, positive and negative predictive and accuracy of computed tomography in the detection of perforated appendicitis (79.07%, 89.06%, 70.8%, 92.7%, 86.5%). Perforated appendicitis is an emergency condition that can be promptly managed non-operatively, based on timely and accurate interpretation of radiological imaging findings15. The most popular tool of investigation nowadays is a contrast enhanced CT scan, which has proved its reliability to identify acute appendicitis correctly. Data recorded shows sensitivities and specificities of up to 90% 16. Meanwhile a simultaneous decline has also been observed in the negative surgical appendectomies from the earlier reported 15-20% to 2-12% by utilizing contrast CT scan in patients with an inflamed appendix17. A large multicenter study has demonstrated negative appendectomy rates of 4.5% in patients who had CT scan compared to a rate of 10% in those who had not performed any prior imaging18. This has led to the prevention of unnecessary surgeries with better patient outcomes in terms of both prognosis and cost effectiveness. Though it seems quite obvious that a contrast enhanced CT scan abdomen is an efficient imaging tool to detect and diagnose non-ruptured appendicitis, the demarcation of a perforated from a non-ruptured one however still appears to be less precise, leaving an opportunity for an under evaluated subject to be further explored scientifically.
Reasons for the difficulty to distinguish a perforated from a non-perforated appendicitis are due to the complex imaging features of rupture on CT. For example, when perforated, extraluminal air, colonic mural edema, enhancing ileal walls, extra-bowel appendicolith, abscess, phlegmon, peri appendiceal fluid and mesenteric stranding of varying severity can be detected on CT scans19,20. This rich spectrum of imaging presentations at times renders diagnosing a perforation less reliable. Other studies have observed the role of CT scan in perforation; however, the accuracy of diagnosis is established on histopathology or per-operative findings only21. However, these earlier studies have paved a model for future researches, but they still lack clarification on diagnostic criteria of perforation. The average patient age was detected to be 26.9 years, ranging between 15 and 50 years22. In another study, the mean age was 31.4 years, which is comparable to that of the current study. Out of 171 cases, 105(61.4%) were found to be male and 66(38.6%) females. The present study showed a higher number of males affected by this disease entity as compared to females, indicating an obvious male predilection in the current region for the inflammation of the appendix. Petroianu’s study also recorded a greater number of males than females23.
In the present study, 25.1% of patients were found to have perforated appendix on histopathology. However, in another study perforated appendicitis rate was somewhat higher with 31.3% having perforation24. Omari et al. showed a ruptured appendix in 41% of elderly patients. As the patients selected in the study were younger, the number of perforated cases was lower as compared to mentioned study25. The sensitivity, specificity, positive and negative predictive value of study results including the diagnostic accuracy of contrast enhanced computed tomography abdomen in detecting perforated appendicitis was 79.07%, 89.06%, 70.8%, 92.7% and 86.5% respectively. This was in accordance to a study with, sensitivity and specificity of detecting ruptured appendicitis is 69% and 97% respectively6. Fraser’s study reports a CT sensitivity of 62% with a specificity of 81% in predicting appendiceal rupture26.
Tsuboi et al. retrospective study stated that if any mural defects were found in an enhancing inflamed appendix as the only CT scan feature to establish rupture, this itself will raise the sensitivity, specificity, and diagnostic accuracy to 95.0%, 96.8%, and 96.1%, respectively27. Comparison of the validity of study findings with other studies was reviewed and shown with current study having a sensitivity of 79.07% and a specificity of 89.06% (see Figure 2).
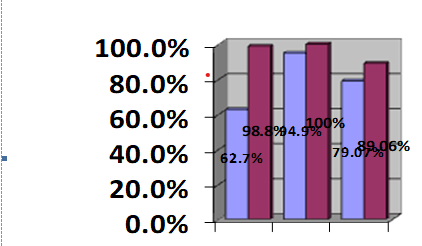
Figure 2: Comparison of validity findings with other studies.
This study reports CT scan accuracy in detecting perforated appendicitis of 83.8% in men and 90.9% for women. Likewise, for the age categorization, CT scan accuracy was more than 88.7% for above 30 years of age and 85.6% for those below and equal to 30 years.
Horrow et al. included Helical CT scan in their study by applying numerous scanning protocols including those with oral contrast, others with both oral and intravenous contrast and by keeping the slice thickness from 5mm to 10mm28. It was recorded that mural defects seen in the enhancing appendix with abscess formation, phlegmon, extra-bowel gas and extraluminal appendicolith had a sensitivity of 94.9% for perforated appendicitis and a specificity of 100%. On the other hand, Kim et al. in their data reported a sensitivity of 62.7% and a specificity of 98.8% 29.
A limitation to the current study was that it was a single center based study, which was performed in an urban setting, not covering a significant number of patient populations. Also of note is to acknowledge the burden of ionizing radiation exposure while performing these CT scan in patients with acute appendicitis, which usually targets the youthful population. This could be addressed by obtaining a contrast enhanced low dose CT scan instead of a contrast enhanced standard CT scan which fulfills the criterion of ‘as low as reasonably achievable (ALARA), thus reducing the exposure of patients to harmful radiations. Few drawbacks to standard abdominal CT however exist including nearly two hours required for oral contrast administration, ionizing radiation exposure and intravenous contrast side effects.
CT scan was found to be 79.07% sensitive and 89.06% specific in accurately diagnosing perforated appendicitis. This could be utilized in patient selection with ruptured Acute Appendixes to initiate non-surgical treatment.
We are thankful to Dr Haider who helped design the study and Dr. Afaque who reviewed this paper before submission.
The authors declare no conflict of interest.
This study was conducted after approval from the Ethical Board and Medical Superintendent of Dr. Ziauddin Hospital, North Nazimabad.
The manuscript was written after the informed consent of the included patients.
MK was responsible for documenting and analyzing all the patient data. AU and ZS wrote the manuscript.
- Ferris M, Quan S, Kaplan BS, Molodecky N. The global incidence of appendicitis: a systematic review of population-based studies. Ann Surg. 2017;266:237-241.
- Ali M, Iqbal J, Sayani R. Accuracy of computed tomography in differentiating perforated from nonperforated appendicitis, taking histopathology as the gold standard. Cureus. 2018;10(12):1-7.
- Salminen P. Acute appendicitis incidence—predisposing factors, from microbiota to socioeconomic status? JAMA Surg. 2020;155(4):338-339.
- Alvarado A. Clinical approach in the diagnosis of acute appendicitis. Garbuzenko D. Current issues in the diagnostics and treatment of acute appendicitis. Intech Open. 2018:13-42.
- Ali MT, Nabil DM. The role of 256-slice CT in differentiation between non-perforated and perforated appendicitis. Egypt J Radiol Nucl Med. 2017;48(1):15-21.
- Siddiqui AH, Afzal S. Perforated appendicitis: Accuracy of CT diagnosis and correlation of CT findings with length of hospital stay. J Coll Physicians Surg Pak. 2007;17(12):721-725.
- GlobalSurg Collaborative. Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a multicenter, prospective, cohort study. Surg Endosc. 2018; 32: 3450-3466.
- Song X, Shi M, Liu W, Ge Y, Wang P. Relative CT number of periappendiceal fat stranding may be an applicable index for estimating the severity of acute appendicitis. Br J Radiol. 2021;94(1120):e20200437.
- Topel Ç, Onur MR, Akpınar E, Karaosmanoğlu AD, Akata D, Karçaaltıncaba M. Low tube voltage increases the diagnostic performance of dual-energy computed tomography in patients with acute appendicitis. Diagn Interv Radiol. 2019;25(4):257-264.
- Elbanna KY, Mohammed MF, Chahal T, Khosa F, Ali IT, Berger FH, et al. Dual-energy CT in differentiating nonperforated gangrenous appendicitis from uncomplicated appendicitis. AJR Am J Roentgenol. 2018;211(4):776-778.
- Tankel J, Keinan A, Blich O, Koussa M, Helou B, Shay S, et al. The decreasing incidence of acute appendicitis during COVID-19: a retrospective multi-centre study. World Journal of Surgery. 2020;44:2458-2463.
- Hong W, Kim MJ, Lee SM, Ha HI, Park HC, Yeo SG. Computed tomography findings associated with treatment failure after antibiotic therapy for acute appendicitis. Korean J Radiol. 2021;22(1):63-71.
- Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):1-42.
- Haijanen J, Sula S, Salminen P. Optimizing the gold standard-low dose computed tomography modalities as a part of clinical practice in acute appendicitis imaging. JAMA Surg. 2021;156(4):351-352.
- Debnath J, George RA, Ravikumar R. Imaging in acute appendicitis: What, when, and why? Med J Armed Forces India. 2017;73(1):74-79.
- Jha P, Espinoza N, Webb E, Kohli M, Poder L, Morgan T. Single institutional experience with initial ultrasound followed by computed tomography or magnetic resonance imaging for acute appendicitis in adults. Abdom Radiol. 2019;44(7):2357-2365.
- Wagner M, Tubre DJ, Asensio JA. Evolution and current trends in the management of acute appendicitis. Surg Clin North Am. 2018;98(5):1005-1023.
- Sammalkorpi HE, Leppäniemi A, Lantto E, Mentula P. Performance of imaging studies in patients with suspected appendicitis after stratification with adult appendicitis score. World J Emerg Surg. 2017;12(1):1-8.
- Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology. 2018;288(3):717-727.
- Podda M, Gerardi C, Cillara N, Fearnhead N, Gomes CA, Birindelli A, et al. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg. 2019;270(6):1028-1040.
- Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, Ansaloni L, et al. Prospective observational study on acute appendicitis worldwide (POSAW). World J Emerg Surg. 2018;13(1):1-10.
- Vanhatalo S, Munukka E, Sippola S, Jalkanen S, Grönroos J, Marttila H, et al. Prospective multicentre cohort trial on acute appendicitis and microbiota, aetiology and effects of antimicrobial treatment: study protocol for the MAPPAC (Microbiology APPendicitis ACuta) trial. BMJ Open. 2019;9(9):1-8.
- Petroianu A. Diagnosis of acute appendicitis. Int J Surg. 2012;10(3):115-119.
- Dian A, Ali A, Azam UF, Khan MM. Perforated appendix-our local experience. Rawal Med J. 2011;36(2):97-99.
- Omari AH, Khammash MR, Qasaimeh GR, Shammari AK, Yaseen MK, Hammori SK. Acute appendicitis in the elderly: risk factors for perforation. World J Emerg Surg. 2014;9(1):1-6.
- Fraser JD, Aguayo P, Sharp SW, Snyder CL, Rivard DC, Cully BE, et al. Accuracy of computed tomography in predicting appendiceal perforation. J Pedia Surg. 2010;45(1):231-234.
- Tsuboi M, Takase K, Kaneda I, Ishibashi T, Yamada T, Kitami M, et al. Perforated and nonperforated appendicitis: defect in enhancing appendiceal wall—depiction with multi–detector row CT. Radiology. 2008;246(1):142-147.
- Horrow MM, White DS, Horrow JC. Differentiation of perforated from nonperforated appendicitis at CT. Radiology. 2003;227(1):46-51.
- Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology. 2018;287(1):104-115.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
