By Javeria Junaid, Saddam Mazar, Shahzaib Riaz Baloch, Fatima Bashir, Mohammed Sohail Rafi, Imtiaz Ahmed Hashmi
AFFLIATIONS:
- Department of Orthopedics and Spine Surgery, Dr. Ziauddin University Hospital, Karachi, Pakistan.
Background: Scoliosis is defined as a three-dimensional deformity of spine. Surgical treatment is indicated for curves equal to/or more than 40 degrees in magnitude. Curve flexibility is determined preoperatively through bending films, which help in the selection of fusion levels. Surgical treatment for fully-grown spine is a spinal fusion use to inhibit the progress of deformity which further helps in balancing of both sagittal and coronal planes. Therefore, this study aimed to find out the association between predicted via bending films after correction and final surgical correction of skeletally mature patients with Adolescent Idiopathic Scoliosis (AIS).
Methods: Thirty-three patients with Adolescent Idiopathic Scoliosis (AIS) were recruited for the study. Those patients were operated at Dr. Ziauddin University Hospital, Karachi from June 2016 to June 2020. Using Pre- and post-operative radiographs of the spine, Cobb values were used to calculate the percentage of correction achieved. Percentage correction (surgical) was then compared to correction possible (predicted) to find association via an independent t-test with p<0.05 considered as statistically significant.
Results: Out of total 33 patients, 24 (72.7%) were females and 9 (27.2%) were males. The mean age of the patients was 17.2±3.0 years. Using bending films, correction of the scoliotic deformity was predicted through measured angles with 78±18°. The corrections’ difference was 84.5±11°. This difference was found to be statistically insignificant (p=0.0769) which showed no difference in predicted and actual correction achieved.
Conclusion: In skeletally mature patients with AIS, bending films have been shown to accurately predict the amount of postoperative correction of Cobb’s angle which is possible.
Keywords: Age Determination by Skeleton; Scoliosis; X-Ray Film; Spinal Curvatures.
Scoliosis is defined as an abnormal lateral curvature of the spine. This is a much more complex and a three-dimensional spinal deformity1,2. There are multiple reasons for this deformity and they have been classified according to cause and the age of onset2. Adolescent Idiopathic Scoliosis (AIS) is a deformity that becomes apparent when it coincides with the adolescent growth spurt normally experienced by children between the ages of 9 and 14 years2. In Adolescent Idiopathic Scoliosis (AIS), curves of equal to and greater than 40 degrees, measured with Cobb’s method3 are treated surgically as they tend to keep progressing at a rate of one degree per year even after skeletal maturity has been acheived4,5. This is the sign for fusion when skeletal maturity has been reached to the extent in such children.
Surgical treatment options for a fully-grown spine are Posterior and/or Anterior spinal fusion with a primary goal to stop the deformity and achieve balance in both sagittal and coronal planes. This comes with a secondary goal of achieving deformity correction. Added benefits of deformity correction are better psychosocial profile and a straighter spine is acceptable to both the patient and their family2.
In order to know when the spine has grown to maturity, Risser Staging System6 is used. The Risser stage is used in concurrence with chronologic age, skeletal age and time of achievement of menarche in females to assess the optimal time for fusion. In particular, vertebral growth is unlikely to persist after Risser Stage 46-9. Skeletal maturity is generally achieved at 11 to 13 years of age. In particular, clinicians should remain aware that vertebral growth is unlikely to persist after Risser Stage 46. This is the time when the spine is mature and spinal fusion is going on. A fundamental step in the surgical plan is to determine the flexibility of the curve; this is done via bending films. Bending films are used to direct the selection for the levels of fusion4 and help to determine the apical, neutral and the end vertebrae for posterior spinal fusion.
Furthermore, supplementary radiography helps to plan more supplementary procedures, like osteotomy, anterior release or use of multiple implants which may be required during surgery10-12. It would be interesting to see if we can use any preoperative modality to predict the amount of intra and postoperatively correction. The ideal outcome for a scoliosis patient would be to achieve zero degrees Cobb’s angle with perfect sagittal balance; this is rarely possible in reality12.
There are various varieties of methods of bending radiographs utilized to determine the flexibility of curves in scoliosis such as; active lateral oblique views9, views under traction in dorsal decubitus and views with a fulcrum at the apex of the deformity in lateral decubitus13,14. In our clinical facilities, we use the fulcrum or stress-bending radiographs for this purpose and this is done in the presence of a surgeon from the primary operating team. It has been seen as easy to perform and inexpensive practice. The question we then ask is: can these bending views then also be used to accurately predict, the final correction achievable in Adolescent Idiopathic Scoliosis in a mature spine? The objective of this study was to find out any association between predicted correction in lateral bending radiographs and final correction achieved, in surgical correction of skeletally mature patients with Adolescent Idiopathic Scoliosis (AIS).
In this study, thirty-three patients were recruited with Adolescent Idiopathic Scoliosis (AIS) and had undergone surgical correction at Dr. Ziauddin University Hospital Karachi from June 2016 to December 2020. Their files were retrospectively analyzed after ERC approval (Ref: 1611119JJORT). The inclusion criteria considered as the following: both genders, diagnosed and operated for Adolescent Idiopathic Scoliosis (AIS), the age range between 11-21 years; presenting with scoliotic deformity of equal to and more than 40 degrees, measured utilizing was Cobb’s method 3; further classified by Lenke et al 6.
The Exclusion criteria was formulated as patients with secondary scoliosis due to any other cause, patients with surgeries including implants other than only pedicle screws, and cases involving the inclusion of vertebras above T2 or below L3 in the arthrodesis. Based on these, only two patients were subsequently excluded from the study. The operative technique for insertion of the pedicle screws was “freehand”, based on anatomical markers15,16. All surgical interventions utilized same brand and model of Titanium implants (Universal Spine System 1, Synthes) 17. Cantilever technique for surgical correction of the spinal deformity was adapted in all surgeries. All the patients, preoperatively and at immediate postoperative stage, were documented using panoramic radiographs in upright standing position in the antero-posterior and lateral views as seen in the Figure 1 below.
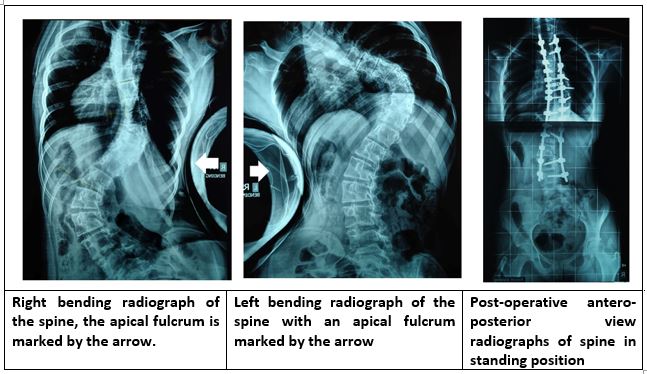
Figure 1: Demonstration of pre-operative bending and post-operative radiographs.
A right and left bending radiograph in supine position with the apex of the curves opposed with a fulcrum were obtained preoperatively and documented in two films. The fulcrum is formed by having the patient lie on a plastic tube so, that the body weight of the patient acts as a force to correct the deformity as much as possible. Knowing what percentage of the deformity can be reversed in a matter of speaking is a good indication of the flexibility of the spine. Next, we determined the pre-operative Cobb angles and the predicted pre-operative correction of the curves which was estimated via the bending films and documented by the same team. Subsequently, the primary team also then determined post-operative Cobb’s angles (after final correction).
The preoperative and postoperative Cobb values of the curves were used in obtaining the percentage of correction achieved. Percentage correction (surgical) was then compared to correction possible on radiographs (predicted) to find out any association via an independent sample t-test and it was run on SPSS.
Out of total 33 patients, only 31 fulfilled the inclusion criteria for this study, 24 (72.7%) were females and 9 (27.2%) were males. At presentation and after workup, it was found that 28.5% of the patients presented with Risser stage type 4 and 71.4% could be classified as being Risser stage 5 at preoperative diagnosis. Out of 31 patients the most common patterns of deformity (Chart 1) classified according to Lenke were 3CN and 2B+, next most common were 2BN, 3BN, and 1B+ (Figure 2).
Chart 1: Radiographic parameters for female patients.
| AIS Lenke Classification | Curve at presentation (degrees) | Left bending (degrees) | Flexibility rate | Percentage improvement | Levels of Instrumentation |
| 1B+ | 80 | 58 | 27.5 | 95.0 | T2-L4 |
| 3CN | 101 | 60 | 40.5 | 88.1 | T3-L1 |
| 3BN | 70 | 40 | 42.8 | 84.2 | T2-L3 |
| 3BN | 112 | 80 | 28.5 | 82.1 | T4-L4 |
| 2BN | 68 | 42 | 38.2 | 82.3 | T2-L4 |
| 2B+ | 101 | 68 | 32.6 | 88.1 | T2-L4 |
| 3CN | 110 | 50 | 54.5 | 69.0 | T4-L1 |
| 1B+ | 54 | 42 | 22.2 | 81.4 | T2-L4 |
| 3BN | 80 | 68 | 15.0 | 93.7 | T4-L2 |
| 2BN | 92 | 56 | 39.1 | 90.2 | T4-L2 |
| 2B+ | 78 | 48 | 38.4 | 80.7 | T4-L2 |
| 1B+ | 80 | 58 | 27.5 | 95.0 | T2-L4 |
| 3CN | 101 | 60 | 40.5 | 88.1 | T3-L1 |
| 3BN | 70 | 40 | 42.8 | 84.2 | T3-L3 |
| 3BN | 112 | 80 | 28.5 | 82.1 | T4-L4 |
| 2BN | 68 | 42 | 38.2 | 82.3 | T2-L4 |
| 2B+ | 101 | 68 | 32.6 | 88.1 | T2-L4 |
| 3CN | 110 | 50 | 54.5 | 69.0 | T4-L1 |
| 1B+ | 54 | 42 | 22.2 | 81.4 | T2-L4 |
| 3BN | 80 | 68 | 15.0 | 93.7 | T4-L2 |
| 2BN | 92 | 56 | 39.1 | 90.2 | T4-L2 |
| 2B+ | 78 | 48 | 38.4 | 80.7 | T4-L2 |
| 1BN | 60 | 40 | 34.9 | 90.5 | T4-L4 |
AIS = Adolescent Idiopathic Scoliosis
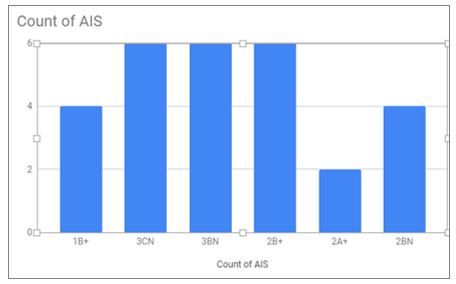
Figure 2: Count of Adolescent Idiopathic Scoliosis (AIS) according to Lenke classification.
The mean age of the patients in our study was 15.2±4 years. The mean values for the pre-operative and post-operative Cobb angles are represented in Table 1; these have been measured on standard radiographs via the Cobb method.
Table 1: Radiographic parameters for male patients.
| AIS Lenke Classification | Curve at presentation (degrees) | Left bending (degrees) | Flexibility rate | Percentage improvement | Levels of Instrumentation |
| 2B+ | 52 | 42 | 19.2 | 100.0 | T2-L2 |
| 2A+ | 84 | 56 | 33.3 | 95.2 | T4-L2 |
| 3CN | 94 | 70 | 25.5 | 89.3 | T2-L2 |
| 2B+ | 52 | 42 | 19.2 | 100.0 | T2-L2 |
| 2A+ | 84 | 56 | 33.3 | 95.2 | T4-L2 |
| 3CN | 94 | 70 | 25.5 | 89.3 | T2-L2 |
| 1CN | 113 | 70 | 29.8 | 89.3 | T4-L2 |
AIS = Adolescent Idiopathic Scoliosis
Using bending films, we were able to predict that we may be successful in achieving 78%±18 correction of the scoliotic deformity in the above-mentioned patients. In reality, we were able to achieve 84.5%±11 correction. The difference between these sets of values were tested using independent sample t-test and it was found to be statistically insignificant at 95% CI (p=0.0769).
Table 2: Mean values for the pre-post-operative Cobb’s angles with reference to predicted correction and final correction percentages.
| Parameters | Mean±SD | Change | p-Value |
| Pre-operative Cobb’s Angle | 86.4± 18 | 69.3% | – |
| Post-operative Cobb’s Angle | 17.1± 13 | ||
| Predicted Correction percentage | 78%± 18 |
6.5% |
p = 0.0769 |
| Final Correction percentage | 84.5%± 11 |
Table 2 shows that there is no statistically significant difference between the predicted correction achievable based on bending films and the actual surgical correction achieved in these patients. Therefore, positive correlation between these two can be established. This proves that fulcrum bending films as done under our care. Therefore, we infer that pre-operative stress bending radiographs are predictive of final surgical correction in patients with Adolescent Idiopathic Scoliosis (AIS) in skeletally mature spines.
Previous studies have attempted to predict percentage correction in spinal deformity using separate formulas, to the best of our knowledge no one has done a simple comparison of correction percentage in bending films to actual surgical correction. The treatment of the deformities in the vertebral spine is formed by evaluating the flexibility of all scoliotic curves (proximal thoracic, main thoracic and lumbar) 6. Many methods of radiography by different authors have been formulated for this purpose. It is important to evaluate primary and secondary curves, as the basic concept is that the compensatory curves have a propensity of spontaneous correction and thus routine arthrodesis should not be performed for those4. In our hospital, we use lateral bending stress views with a fulcrum at the apex to evaluate major curves, this method is safe to perform patient friendly and is a cost effective method17. It also helps to predict which curves are major and which are minor as per definition like any curve that is able to improve to less than 25 degrees is a minor curve, this can be seen in the Lenke classification as well18,19.
Older patients with Adolescent Idiopathic Scoliosis (AIS) pose a unique clinical challenge as achievement of skeletal maturity reduces spine flexibility20. Thus, correction goals must be tailored for personal and individual goals after the age of 13-14 years. Many times, surgical intervention is undertaken only to halt curve progression and complete correction is not possible as bending views show very little spinal flexibility21, 22. In older patients, the Risser stage is used in concurrence among other tools, like chronologic age, skeletal age, and time since menarche in females to predict curve progression23-24. It is universally accepted that vertebral growth and spinal flexibility is unlikely to persist after Risser Stage 4. After 4 months of the peak of the adolescent growth spurt, the apophysis appear on the iliac crest (age 12-15 years), which coincides with the achievement of menarche in females. Thus, Risser stage is based on how much of the apophysis has fused till a certain time. The Risser stage 5 when the adolescent growth spurt is completed and by then the iliac apophysis has fused with the iliac crest. After this stage, only 1-2 cm of longitudinal spinal growth is added to children’s growth25,26.
This study was assumed to assess whether if bending films can be used to accurately predict percentage of deformity correction possible in patients who have already achieved skeletal maturity, as defined by the late stages of Risser. Depending on the classification of scoliosis, comparative studies have shown that, the selection of which curve or curves to fuse is best determined by a combination of standing posteroanterior, lateral films and the supine bending films9. They showed bending films to be better predictors of flexibility, especially for curves more than 60 degrees9. Another retrospective study showed that the degree of postoperative correction achieved, and it highly correlates with the age of the patient, the Cobb angle in fulcrum bending radiographs, and the fulcrum flexibility rate, could be accurately calculated with a predictive equation. This allows the surgeon to go ahead and plan the addition of any further surgical release or osteotomies if required 10.
It has been reported that the predictability of flexibility and correctability of fulcrum bending radiographs are more significant than lateral-bending radiographs in Adolescent Idiopathic Scoliosis (AIS) group of patients having undergone posterior spinal arthrodesis with segmental spinal instrumentation14. This supports our findings as the present study results show no significant statistical difference between the values predicted via bending views and the real post-operative values. Therefore, it is establishing the validity of bending films to predict final achievable correction in AIS of older and skeletally matured patients.
Exclusive use of pedicle screws for surgical interventions of AIS attained popularity after the publication of the paper by Suk et al.5, 24 and now, it is the gold standard surgical procedure for the correction of adolescent idiopathic scoliosis21. These implants lay out support in all the three spinal columns and bear biomechanical characteristics superior to other types of materials such as hooks and sub-laminar wires 23, 24.
The limitations to the study were the smaller sample size as this is a rare disorder. In addition, there is no long-term follow up included in this study as we only used the Cobb angles from the immediate pre- and post-operative period for assessments. Other surgeons even at two years’ follow-up with exclusive use of pedicle screws have only reported a minimal mean loss of correction and this was deemed statistically insignificant25,27. We recommend that any analyses in the future should be aimed towards applying a similar method of prediction on larger samples and with a long-term follow-up.
Using pre-operative radiographs with an apical fulcrum for two sided bending views, it is possible to predict postoperative correction using pedicle screw fixation for skeletally matured patients with Adolescent Idiopathic Scoliosis (AIS).
The authors would like to extend their gratitude to the staff of the hospital their help in patient management during research work.
The authors declare no conflict of interest.
The Ziauddin University Hospital approved the study with the ERC approval Ref: 1611119JJORT.
Verbal and written informed consents were obtained from all patients.
All authors contributed equally in this clinical research study.
- Veldhuizen AG, Wever DJ, Webb PJ. The aetiology of idiopathic scoliosis: biomechanical and neuromuscular factors. Eur Spine J. 2000;9(3):178-184.
- Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Scoliosis: a review. Pediatr Surg Int. 2008;24(2):129-144.
- Cobb JR. Outline for the study of scoliosis. Instr Course Lect. 1948;5:261-275.
- Moe JH, Byrd JA. Idiopathic scoliosis. In: Lonsteins JE, Winter RB, Bradford DS RB, Olgivie JW, editors. Moe’s textbook of scoliosis and other spinal deformities. 2nd ed. Philadelphia: Saunders; 1987. p.191-232.
- Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20(12):1399-1405.
- Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg. 2001;83(8):1169-1181.
- Large DF, Doig WG, Dickens DR, Torode IP, Cole WG. Surgical treatment of double major scoliosis. Improvement of the lumbar curve after fusion of the thoracic curve. J Bone Joint Surg Br. 1991;73(1):121-124.
- McCall RE, Bronson W. Criteria for selective fusion in idiopathic scoliosis using Cotrel-Dubousset instrumentation. J Pediatr Orthop. 1992;12(4):475-479.
- Vaughan JJ, Winter RB, Lonstein JE. Comparison of the use of supine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine. 1996;21(21):2469-2473.
- Cheung WY, Lenke LG, Luk KD. Prediction of scoliosis correction with thoracic segmental pedicle screw constructs using fulcrum bending radiographs. Spine. 2010;35(5):557-561.
- Hamzaoglu A, Talu U, Tezer M, Mirzanl C, Domanic U, Goksan SB. Assessment of curve flexibility in adolescent idiopathic scoliosis. Spine. 2005;30(14):1637-1642.
- Watanabe K, Kawakami N, Nishiwaki Y, Goto M, Tsuji T, Obara T, et al. Traction versus supine side-bending radiographs in determining flexibility: what factors influence these techniques? Spine. 2007;32(23):2604-2609.
- Polly Jr DW, Sturm PF. Traction versus supine side bending: which technique best determines curve flexibility? Spine. 1998;23(7):804-808.
- Cheung KM, Luk KD. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg. 1997;79(8):1144-1150.
- Oh CH, Yoon SH, Kim YJ, Hyun D, Park HC. Technical report of free hand pedicle screw placement using the entry points with junction of proximal edge of transverse process and lamina in lumbar spine: analysis of 2601 consecutive screws. Korean J Spine. 2013; 10(1): 7-13.
- Avila MJ, Baaj AA. Freehand thoracic pedicle screw placement: review of existing strategies and a step-by-step guide using uniform landmarks for all levels. Cureus. 2016;8(2): 1-15.
- Synthes Spine. Universal Spinal System (USS) [Internet]. Synthes Canada Limited, 2006 [cited 2021 Apr 16]. Available from: http://synthes.vo.llnwd.net/o16/Mobile/Synthes%20North%20America/Product%20Support%20Materials/Technique%20Guides/SPINE/SPTGUSSJ4437A.pdf
- Chen ZQ, Zhao YF, Bai YS, Liu KP, He SS, Wang CF, et al. Factors affecting curve flexibility in skeletally immature and mature idiopathic scoliosis. J Orthop Sci. 2011;16(2):133-138.
- Sanders JO. Maturity indicators in spinal deformity. J Bone Joint Surg. 2007;89(1):14-20.
- Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. 2012;21(1):13-22.
- Lehman Jr RA, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine. 2008;33(14):1598-604.
- Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res.1984;189:65-76.
- Cheng I, Hay D, Iezza A, Lindsey D, Lenke LG. Biomechanical analysis of derotation of the thoracic spine using pedicle screws. Spine. 2010;35(10):1039-1043.
- Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel-Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18(6):341-346.
- Dobbs MB, Lenke LG, Kim YJ, Kamath G, Peelle MW, Bridwell KH. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine. 2006;31(20):2400-2404.
- Risser JC. The iliac apophysis: an invaluable sign in the management of scoliosis. Clin Orthop Relat Res. 1958;11:111-119.
- Cotrel Y, Dubousset J. A new technic for segmental spinal osteosynthesis using the posterior approach. Journal of orthopedic and reconstructive surgery of the motor system. 1984;70(6): 489-494.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
