By Ambreen Shahnaz1, Madiha Bashir2, Baseera Khan3
AFFILIATIONS:
- Surgery and Allied Department, Rawalpindi Medical University, Rawalpindi, Pakistan.
ABSTRACT
Background: Peripheral intravenous cannulation (PIVC) is a routine invasive procedure being done on both medical and surgical patients. Phlebitis is its most widespread complication. The objective of this study was to determine the incidence of phlebitis with PIVC in surgical patients post-operatively.
Methods: This cross-sectional study was conducted in surgical units of Benazir Bhutto Hospital and Holy Family Hospital, Rawalpindi from 19th Feb 2018 to 1st April 2018. A total of 222 postoperative patients, with a PIVC in situ, were inspected. Patients who had elective surgical procedures were included, while patients with emergency surgeries, minor surgical procedures or active bloodstream infections were excluded from this study. Twenty-two entries were discarded because of incomplete documentation. Data was analyzed using SPSS, Chi-squared test was applied, and p ≤0.05 was considered statistically significant.
Results: Median age (years) of the samples was 35, 110(55%) were males and 90(45%) females. The upper limb veins were more frequently cannulized 197(98.5%), with the dorsum of the hand being the most common site. Most of the cannulas were being used for the administration of intravenous fluids and medications 136(68%). Only 12(6%) of the inspected cannula sites showed signs of phlebitis and were treated by removal only.
Conclusion: In our study, post-operative rate of cannula site phlebitis discovered was 6%. This is marginally more than global principles of 5%, set up by Infusion Nursing Society (INS) for any given population. Although, this has been lessened from a reference range of 21.9% – 51.49% in the course for the last few decades.
Keywords: Cannula; Surgery; Phlebitis; Elective Surgical Procedures; Peripheral Venous Catheterization.
Corresponding Author:
Dr. Ambreen Shahnaz
Surgery and Allied Department,
Rawalpindi Medical University,
Rawalpindi, Pakistan.
Email: [email protected]
Peripheral intravenous cannulation (PIVC) is a routine invasive procedure being done to both medical and surgical patients for administering fluids, drugs, blood products and nutrition through the venous route1. A global audit done in 2015 showed that over 59% of hospitalized patients had a PIVC in place2. Despite such widespread use intravenous cannulation has its fair share of complications, phlebitis (i.e. inflammation of the walls of the vein) being the most common one2,3. An infected cannula site causes remarkable distress to the patient and requires repositioning of cannula in a different peripheral vein.
Literature available regarding infusion related phlebitis shows an incidence ranging from 3.7% to 80% 4 . The factors responsible for cannula site phlebitis, in general, can be chemical agents like the drugs5 or fluids6 being administered, physical elements like the material of the intravascular device or the position or duration of cannulation7 or an interplay of all these. Also, the level of skill and knowledge of the personnel involved in the process of catheterization plays an important role8. These factors can be considered for all sorts of patients and not specifically in surgical patients. Literature however suggests that surgical patients might be at greater risk for phlebitis, Cui and Fang state that the surgical trauma inflicted on the body might itself be a causative factor in reduced body defenses and hence the increased propensity for infection9. Therefore, this study aimed to determine the incidence of cannula site phlebitis in surgical patients postoperatively and to see if there is an increased risk of phlebitis or not.
A cross sectional study was conducted in 2018 at the surgical units of Benazir Bhutto hospital and Holy Family Hospital Rawalpindi. Two hundred cases were collected after securing the permission of the Research Committee of Rawalpindi Medical University for Undergraduate Research. A structured observational protocol using a data collection performa was employed to figure out the incidence of cannula site phlebitis in the given setting and to record information like age and gender of the patient, the location and usage of the PIVC, time since cannulation and the qualification of the personnel who cannulated the patient. The Visual Infusion Phlebitis Scale5 (Figure 1) was used.

Figure 1: Visual Infusion Phlebitis (VIP) scale.
Data collection was done over six weeks (February 19, 2018 – April 1, 2018). The sample included surgical patients with a peripheral intravenous cannula in situ, who were hospitalized post operatively and had been cannulized either at the time of surgery or post surgically. A total of 222 cannula sites were inspected cross-sectionally. Twenty-two entries were discarded because of incomplete documentation. Finally, we were left with a total of 200 cases. Patients who had elective surgical procedures were included in this study, while patients who had emergency surgeries or minor surgical procedures or had active bloodstream infections were not included in this study. Informed consent was also obtained from the patients or their attendants. Incidence of cannula site phlebitis was determined, based on the number of cannulas observed in the given period.
Data was analyzed using SPSS (Version 22). Multivariate analysis was done by applying Chi-squared test, for a level of significance of p ≤0.05 on the dependent variable of ‘Incidence of Phlebitis’ and multiple independent variables which were included in this study.
The majority of the patients examined were adults; 55% were males and 45% females. Nurses catheterized all the patients (Table 1). The upper limb veins were preferentially canalized (98.5%), with dorsum of hand being the most common site (61%) followed by forearm (31%) and the antecubital fossa (5%) as shown in Table 1.
Table 1: Descriptive data of patient characteristics, surgical procedures, cannulation and phlebitis grading.
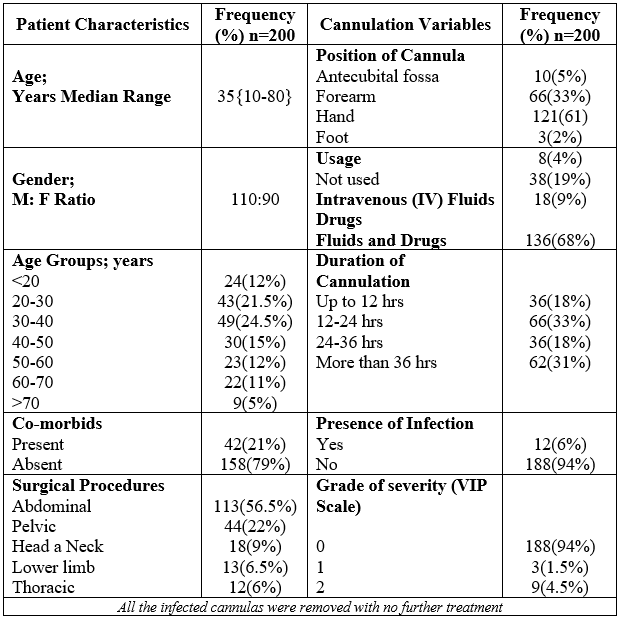
Most of the cannulas were being used for the administration of intravenous fluids and medications (68%), 19% for IV fluids only, 9% for drugs and 4% were not being used at all. Only 6% (12/200) of the inspected cannula sites were infected (Table 1) With 3 being detected at grade 1 and 9 out of the infected 12 being observed at grade 2 of phlebitis (Table 1).
All of these infected cannulas were removed and no additional treatment was required. In view of the fact that, 8/12 cannulas were infected after more than 36 hours had elapsed since their insertion, two were infected within 24-36 hours and two in less than 24 hours (Figure 2).
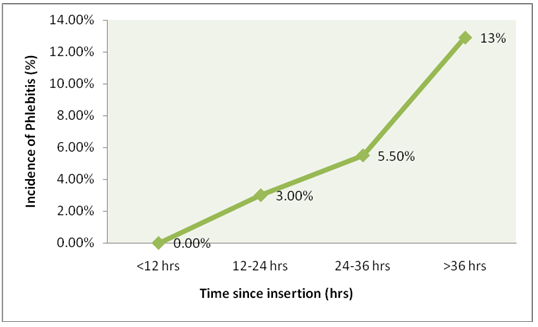
Figure 2: Incidence of phlebitis in relation to time since insertion.
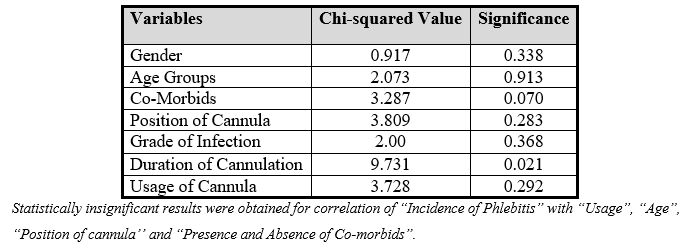
Bivariate analysis demonstrated statistically significant “Likelihood ratio” in Chi-squared tests for correlation (Table 2) between “incidence of phlebitis” and “time since insertion” (p = 0.021) but no association was found between “grade of phlebitis” and “time since insertion”.
Table 2: Statistical relation of incidence of phlebitis with observed variables.
Infusion Nursing Society (INS) in 2006 established that for any given population a phlebitis rate of 5% is acceptable. The current study found an incidence of 6% for the surgical populace in the postoperative period. Although slightly greater than the INS guidelines this is considerably less than the discoveries of past examinations for incidence of phlebitis only for the postoperative period (21.49%-51.9%) 10-14. The results are consistent with the incidences determined in previous studies including all sorts of medical, surgical and other patients (3.7%- 80%) 4,15-17. It can be seen here that phlebitis rates have always been more than the standard values in the post-operative period. The study by Cui and Fang supports this finding by stating that the trauma that an operative insult causes to the tissues might evoke an acute nonspecific inflammatory response, which further leads to clearance of tissue debris from the surgical site. However paradoxically, this inflammatory response may lead to a reduction in the body’s defense against an invasion of pathogens9. Insertion of an intravascular catheter causes endothelial damage as well which as suggested by the Virchow’s triad is involved in thrombus formation, and may lead to thrombophlebitis in cannula sites.
However, this decline in phlebitis rates over the years is multifactorial. Preoperative antibiotic prophylaxis with broad spectrum agents although done for preventing surgical site infection also provides some degree of safety against cannula site phlebitis and thus has become the standard of practice globally18. Careful observation of the SOPs at the time of catheterization along with good patient education enables us to detect phlebitis at earlier grades mostly grade 1 and 2 (25% and 75% respectively in this study) 17,19 with previous similar studies also showing that only few of the cases progress to thrombophlebitis4,20. This also means that cannula site phlebitis can be treated with removal only and does not require additional treatment for this complication of cannulation. Extremes of age (below 10 and above 60) are related to decreased cognitive ability hence reduced self care21. This can be one of the reasons that earlier studies indicate a greater predisposition to cannula site phlebitis at these extremes of age. Reduced immunity in these age groups can also be a contributing factor22.
Our rates may have been lowered due to excluding the patients who had emergency surgeries or minor surgical procedures and including only the elective postoperative patients. As for elective surgical procedures pre-op optimization of the patients is done which leads to a lower level of morbidity in the post operative period23.
The Infusion Nursing Society (INS) in 2011 has abolished the practice of replacing catheters after every 72 hours24 and similarly, recent guidelines also suggest that catheters should only be removed or replaced when they are no more required or have impaired function. Still, the practice of removal and replacement around 72 hours lives on because several studies like this one have established a significant statistical relationship between time since insertion of cannula and incidence of phlebitis4,20,25,26. Center for Disease Control and Prevention (CDC) in its guidelines for the prevention of intravascular catheter related infection has labeled this as an unresolved issue, and suggested that there is no need to resite cannulas to reduce the risk of phlebitis27. Another important recommendation by CDC is to use a midline catheter or peripherally inserted central catheter when IV access is required for more than six days27. Despite the statistically significant relation between dwell time and phlebitis, it is still not advised to resite the cannulas every 72-96 hours, as this only increases the patient agony, the cost of care and the workload of the healthcare providers.
As observed by Dillon et al., placement of intravenous cannula at forearm/hand shows greater sustainability28, CDC also advocates for a preferential use of upper extremities in adults27. Our study also indirectly supports this finding as most of the Peripheral intravenous catheters (PIVCs) were placed at forearm and no relationship was established between phlebitis and location of cannula in the present study28,29.
Phlebitis cannot be labeled as a gender specific complication as some studies show greater risk associated with the female gender7,30 while others with the male gender. However, some show no correlation between these variables and this is consistent with the findings in this study. Multiple studies have established a significant relationship between usage of various drugs and fluids and the occurrence of phlebitis4,8,9 but this study fails to establish any such relationship, this could be due to a lack of detailed information about the medications and fluids being administered through the cannula.
As this study was dedicated to determine the incidence and not the etiology of phlebitis, the authors were unable to establish a causal relationship with most of the variables studied. The small sample size was also a limitation in this study.
Our data has shown an incidence of phlebitis of 6% in elective post-operative patients. Pre-operative optimization and perioperative surgical prophylaxis in elective surgical procedures had better equipped these patients to counter the increased risk of infection that surgical trauma poses to their body. Regular daily examination of the cannula site while maintaining asepsis and improved patient education can lead to even better results. In addition, further studies should be done to establish the various risk factors responsible for phlebitis in our setting.
Authors are grateful to Professor Muhammad Idrees Anwar (Dean of Surgery, Rawalpindi Medical University) for his guidance.
The authors declare no conflict of interest.
The Research Committee of Rawalpindi Medical University for Undergraduate Research has approved the study (1/2018).
Informed consents were taken from the participants of the study.
AS had given the conception of research work and design, performed the literature review and formulated research questionnaire for data analysis, interpretation and manuscript writing. MB had also searched the literature and assisted in data collection and entry. BK had proofread the article and helped the authors in conceptual research work, design, and data collection.
- Ronan P, Sullivan O. Guideline for clinical staff on intravenous cannulation [Internet]. Department of Nursing; 2016 [cited 2018 Jun 19]. 5p. Available from: https://www.olchc.ie/Healthcare-Professionals/Nursing-Practice-Guidelines/Intravenous-Cannulation-.pdf
- Alexandrou E, Ray-Barruel G, Carr PJ, Frost S, Inwood S, Higgins N, et al. International prevalence of the use of peripheral intravenous catheters. J Hosp Med. 2015;10(8):530-533.
- Suliman M, Saleh W, Al-Shiekh H, Taan W, AlBashtawy M. The incidence of peripheral intravenous catheter phlebitis and risk factors among pediatric patients. J Pediatr Nurs. 2020;50:89-93.
- Salgueiro-Oliveira A, Parreira P, Veiga P. Incidence of phlebitis in patients with peripheral intravenous catheters: The influence of some risk factors. Aust J Adv Nurs. 2012;30(2):32-39.
- Yeesin A, Rojanaworarit C, Chansatitporn N. Incidence of peripheral phlebitis and its predictive characteristics infemale inpatients hospitalized at a public hospital in thailand : A prospective cohort study. Int J Adv Comput Theory Eng. 2017;27-33.
- Infusion Nurses Society. Supplement to infusion therapy standards of practice [Internet]. Infusion Nurses Society; 2016 [cited 2019 Feb 15]. 169p. Available from: https://journals.lww.com/journalofinfusionnursing/pages/currenttoc.aspx
- Maki DG, Ringer M. Risk factors for infusion-related phlebitis with small peripheral venous catheters: a randomized controlled trial. Ann Intern Med. 1991;114(10):845-854.
- Braga LM, Parreira PM, Oliveira AD, Mónico LD, Arreguy-Sena C, Henriques MA. Phlebitis and infiltration: vascular trauma associated with the peripheral venous catheter. Latin American Journal of Nursing. 2018;26:e3002.
- Cui P, Fang X. Pathogenesis of infection in surgical patients. Curr Opin Crit Care. 2015;21(4):343-350.
- Abolfotouh MA, Salam M, Ala’a Bani-Mustafa DW, Balkhy HH. Prospective study of incidence and predictors of peripheral intravenous catheter-induced complications. Ther Clin Risk Manag. 2014;10:993-1001.
- Lv L, Zhang J. The incidence and risk of infusion phlebitis with peripheral intravenous catheters: A meta-analysis. J Vasc Access. 2020;21(3):342-349.
- Mandal A, Raghu K. Study on incidence of phlebitis following the use of pherpheral intravenous catheter. J Family Med Prim Care. 2019;8(9): 2827-2831.
- Washington GT, Barrett R. Peripheral phlebitis: a point-prevalence study. J Infus Nurs. 2012;35(4):252-258.
- Saji J, Korula D, Mathew DA, Mohan L. The incidence of thrombophlebitis following the use of peripheral intravenous cannula in post-operative patients A Prospective observational study. J Dent Med Sci. 2015; 14(6):1-4.
- Arias-Fernández L, Suérez-Mier B, del Carmen Martínez-Ortega M, Lana A. Incidence and risk factors of phlebitis associated with peripheral venous catheters. Clin Nurs. 2017;27 (2):79-86.
- Palese A, Ambrosi E, Fabris F, Guarnier A, Barelli P, Zambiasi P, et al. Nursing care as a predictor of phlebitis related to insertion of a peripheral venous cannula in emergency departments: Findings from a prospective study. J Hosp Infect. 2016;92(3):280-286.
- Atay SE, Şen S, Cukurlu D. Phlebitis-related peripheral venous catheterization and the associated risk factors. Niger J Clin Pract. 2018;21(7):827-831.
- Crader MF, Varacallo M. Preoperative Antibiotic Prophylaxis. [Updated 2020 Mar 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK442032/
- Urbanetto JD, Peixoto CG, May TA. Incidence of phlebitis during use and removal of peripheral intravenous catheter. Latin Am J Nurs. 2016; 24: e2746.
- Panadero A, Iohom G, Taj J, Mackay N, Shorten G. A dedicated intravenous cannula for postoperative use: Effect on incidence and severity of phlebitis. Anaesth. 2002;57(9):921-925.
- Murman DL. The impact of age on cognition. Semin Hear. 2015; 36(3):111-121.
- Montecino-Rodriguez E, Berent-Maoz B, Dorshkind K. Causes, consequences, and reversal of immune system aging. Journal Clini Invest. 2013;123(3):958-965.
- Levy N, Grocott MPW, Carli F. Patient optimisation before surgery: a clear and present challenge in peri-operative care. Anaesth. 2019;74:3-6.
- Spiering M. Peripheral amiodarone-related phlebitis: an institutional nursing guideline to reduce patient harm. J Infus Nurs. 2014;37(6):453-460.
- Webster J, McGrail M, Marsh N, Wallis MC, Ray-Barruel G, Rickard CM. Postinfusion phlebitis: Incidence and risk factors. Nurs Res Pract. 2015;2015:1-3.
- Nyström B, Olesen Larsen S, Dankert J, Daschner F, Greco D, Grönroos P, et al. Bacteraemia in surgical patients with intravenous devices: A European multicentre incidence study. J Hosp Infect. 1983;4(4):338-349.
- Recommendations | BSI | Guidelines Library | Infection Control | CDC [Internet]. 2017 [cited 2020 Nov 24]. Available from: https://www.cdc.gov/infectioncontrol/guidelines/bsi/recommendations.html
- Dillon MF, Curran J, Martos R, Walsh C, Walsh J, Al-Azawi D, et al. Factors that affect longevity of intravenous cannulas: A prospective study. Q J Med. 2008;101(9):731-735.
- Benaya A, Schwartz Y, Kory R, Yinnon AM, Ben-Chetrit E. Relative incidence of phlebitis associated with peripheral intravenous catheters in the lower versus upper extremities. Eur J Clin Microbiol Infect Dis. 2015;34(5):913-916.
- Cicolini G, Bonghi AP, Di Labio L, Di Mascio R. Position of peripheral venous cannulae and the incidence of thrombophlebitis: an observational study. J Adv Nurs. 2009;65(6):1268-1273.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
