By Uzma Ghori1, Sana Ansari2, Erum Memon3, Muhammad Osama Rehman Khalid3, Shumaila Shabbir4
AFFILIATIONS:
- Department of Medicine and Allied, Dr. Ziauddin Hospital, Clifton Campus.
- Department of Quality Assurance, Dr. Ziauddin Hospital, Clifton Campus.
- Department of Medicine, Dr. Ziauddin Hospital, Clifton Campus.
- Department Community Health Sciences (CHS), Dr. Ziauddin Hospital, Clifton Campus, Karachi, Pakistan.
ABSTRACT
Background: Healthcare workers all over the world are suffering physically, mentally and emotionally due to the Covid-19 pandemic. While psychological effects may be more pronounced in a country like Pakistan where such disorders are still considered taboo and remain unattended. The study aimed to identify the prevalence and association of anxiety and depression in healthcare workers in a tertiary care hospital in Karachi during COVID-19 pandemic.
Methods: A descriptive, cross sectional study was performed from 1st June-31stAugust 2020 on n=361 healthcare staff. General Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) tools were used to assess for anxiety and depression respectively. Association between demographic variables age, gender, education, designation, work experience, Covid-19 exposure with anxiety and depression was assessed using the Chi-squared test with p ≤ 0.05 was considered statistically significant.
Results: Anxiety 221(61.5%) and depression 276(76.9%) were more common in doctors compared to other health care workers. The prevalence of severe anxiety 248(69.2%) and severe depression 276(76.9%) was significantly higher in males. Both anxiety and depression were more common with less than 2 years of work experience (p=0.00). Association between years of work experience was similar, with people having less than 2 years of work experience feeling more anxiety (p=0.012) and depression (p=0.003).
Conclusion: Doctors working with Covid-19 patients are more prone to severe anxiety and depression. Early identification and supportive care are essential to ensure that the clinical and para medical staff members assigned to patient care has access to both physical and mental health services.
Keywords: Covid-19; SARS CoV-2; Anxiety; Depression; Generalized Anxiety Disorder; Patient Health Questionnaire.
Healthcare professionals caring for Covid-19 patients have globally been awarded the title “Healthcare Heroes”. While the term was meant to acknowledge the efforts of healthcare workers, it also unintentionally instills expectations of continuous sacrifice and strength. In her study on the media focus of healthcare heroes, Coxstates that the term “hero” is damaging as it fails to acknowledge the limits of duty and the importance of reciprocity, which may have a negative psychological impact on the healthcare workers themselves1.
Even before the Covid-19 pandemic, healthcare workers have been known to suffer from a range of mental disorders due to the psychological and emotional burden resulting from constant exposure to human pain, suffering and death. Compassion Fatigue is commonly defined as a state of exhaustion and dysfunction biologically, psychologically, and socially because of prolonged exposure to compassion stress and all it invokes. It is linked with secondary traumatic stress, burnout, and results in frequent sickness absence, psychological injury claims, job turnover, and negative impact on productivity2.
Apart from the physically long working hours, burn-out in medical professionals is also attributed to lack of control over admissions, out-patient visits, procedures, infection control measures, the false notion of safety precautions, poor communication, lack of preparedness and emotional support, inadequate personal protective equipment (PPE), and perceived fatality3. In a country like Pakistan, psychological problems are rampant for a myriad of causes including less education, financial limitations, frequent severe social difficulties4 and low mental health literacy5. In 2015, a study conducted on doctors, dentists and nurses showed that their mental well-being, diet and exercise patterns are not up to the mark 6, which leaves them vulnerable to other disorders.
The suddenness and severity of the Covid-19 pandemic were such that healthcare workers all over the world were affected in some way or the other. Apart from the viral infection itself, anxiety and depression were amplified by social media paranoia, hoarding and stigmatization, which led to the term corona phobia being, used commonly7. Another study from China showed the overall prevalence of anxiety was 12.5% with most cases being mild8. In a multicenter study in Singapore and India, 5.3% of clinical staff screened positive for moderate to very-severe depression, 8.7% for moderate to extremely severe anxiety, 2.2% for moderate to extremely severe stress, and 3.8% for moderate to severe levels of psychological distress. The commonest reported symptom was headache 32.3% 9.
The objective of our study was to identify the prevalence of anxiety and depression in healthcare workers of a tertiary care hospital in Pakistan and to evaluate the impact of Covid-19. A healthcare worker is one who delivers care and services to the sick and ailing either directly as doctors and nurses or indirectly as aides, helpers, laboratory technicians, or even medical waste handlers10. Therefore, study aimed to identify the prevalence and association of anxiety and depression in healthcare workers in a tertiary care hospital during COVID-19 pandemic.
A descriptive cross-sectional study was conducted at a tertiary care teaching hospital, from 1st June to 31stAugust 2020. The Ethics Review Committee of Dr. Ziauddin Hospital (ERC No. 2230520UGMED) approved the study. The study population consisted of n=361 volunteered health care workers included doctors, nurses, porters, laboratory staff, receptionists, technicians, housekeeping and pharmacists.
Data was collected through a self-administered two-page questionnaire prepared in English and translated into Urdu that included the validated tools of Generalized Anxiety Disorder score for anxiety (GAD-7) and Patient Health Questionnaire score for depression (PHQ-9). The authors distributed a questionnaire and respondents were requested to return the survey after completion. Time required to complete the survey was 20 minutes. Participant’s demographic details were kept anonymous. In addition to the validated questionnaire, participants were also asked regarding their perceptions about hospital preparedness.
Sampling was done using a simple random technique. Statistical analysis was performed using SPSS (Version 20.0). Qualitative data were reported as frequencies and percentages. Association of demographic variables with ordinal scale Depression and Anxiety scale was assessed using the Chi-squared test and p ≤ 0.05 was considered statistically significant.
A total number of 400 participants were approached in the study, of which 363 participants gave consent to participate. Of all the participants, 359 (98.8%) members filled the forms. A majority (57%) of the participants were between the ages of 19 to 29 years. One hundred and forty-one (38.5%) were between 30 and 45 years. There were 192 (52.9%) males and 167 (46%) females. Responses were received from 102 doctors (28.1%), 138 nurses (38%) and 123 (33.9%) other health care workers included staff from infection control, laboratory, radiology, nuclear medicine, pharmacy, operation theatre, rehabilitation sciences, OPD clinics, managers and housekeeping.
Regarding the education status 97 (26.7%) participants were postgraduate, 104 (28.7%) graduate and 162 (44.7%) were having an education level of intermediate or less. Work experience ranged from less than 2 years to more than 10 years. Because 122 (33.6%) participants had, the experience of less than two years. 156 (17.4%) participants had an experience of 2 to 10 years while 63 participants (43%) had a work experience of more than 10 years.
Of all the participants 156 (43%) were married and 97(26.7%) had two or more children, Majority (92%) of the participants had no health-related issues, however, 22(6.1%) had one or more co-morbidities. Around 135 (37.2%) participants reported that their friends and family members are avoiding them because of their Covid exposure. Majority i.e., 187 (51.5%) of the participants had been exposed to Covid-19 patients and 19(5.2%) of the participants were diagnosed with Covid-19.
In response to hospital arrangements, 151 (41.6%) respondents reported that they were satisfied with provision of PPE, 237 (65.3%) reported that they did not have any problems with their work shift. 54 (14.9%) participants were considering resigning due to the Covid-19 pandemic. Regarding anxiety score GAD-7, of all the participants 85 (23.4%) participants were found to have mild anxiety, 53(14.6%) had moderate while 26(7.2%) had severe anxiety. 191(52.6%) participants had no anxiety.
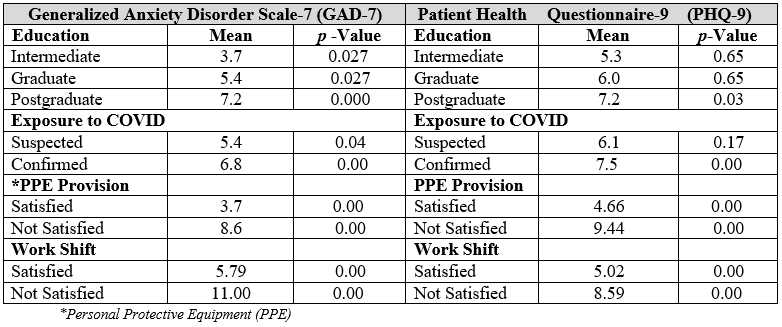
Furthermore, depression score PHQ-9 of participants showed (Table 1) that 96(26.4%) had minimal depression, 85(23.4%) had mild depression, 44(12.1%) had moderate, 29(8%) had moderately severe while 13(3.6%) had severe depression. 85(23.4%) participants had no depression. The GAD-7 score ranged from 0 to 21 with the mean score being 5.19±5.17 and PHQ-9 score ranged from 0 to 27 with a mean score of 6.05±6.03. Association between years of work experience was similar, with people having less than 2 years of work experience feeling more anxiety (p=0.012) and depression (p=0.003). Association of Anxiety and Depression scores with different variables e.g., COVID exposure, provision of PPE, working hours etc with significant p-values are shown in the Table 1.
Table 1: Generalized Anxiety Disorder Scale-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9) association with different variables.
Chi-square analysis showed that the association between designation and generalized anxiety disorder was significant (p=0.000). Anxiety and depression both were found more severe among doctors (61.5% of all cases of severe anxiety and 76.9% of all cases of severe depression) (Figure 1 and 2). Association between gender and depression and anxiety was also significant with p-value (p=0.000). Mild to moderate anxiety and depression were found more in females while severe anxiety and depression was found more in males (69.2% of all cases of severe anxiety and 76.9% of all cases of severe depression).
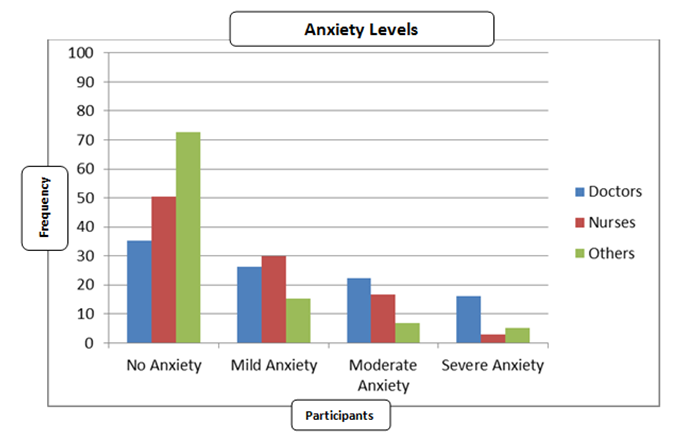
Figure 1: Severity of anxiety amongst doctors, nurses and other health care workers.
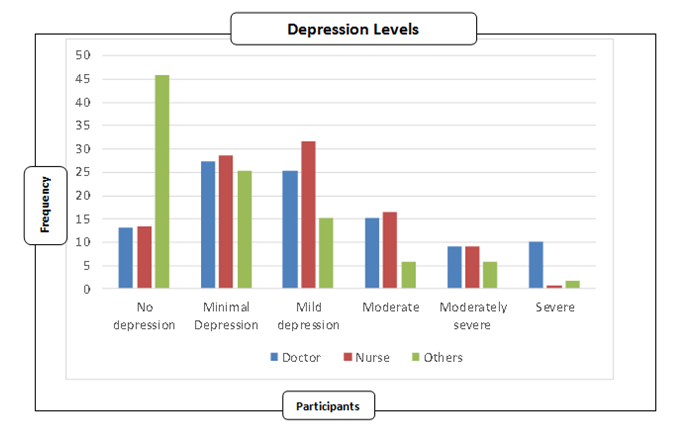
Figure 2: Severity of depression in doctors, nurses and other health care workers.
According to our research, by virtue of their job, clinical staffs are subject to a high level of physical and mental stress. Earlier pre-Covid-19 studies conducted in Pakistan have proven a strong positive correlation between anxiety and depression scores among doctors11 and the inclusion of a global pandemic has worsened the situation. As expected, severe psychological impact was significantly higher in healthcare workers who had much direct exposure to confirmed Covid-19 patients and directly involved with decision making than those who had pre-existing medical conditions.
On the other hand, an interesting finding in our study was that both anxiety and depression were significantly lower in female healthcare workers compared to their male counterparts. This result is contradictory to previous studies, which show female healthcare professionals exhibit higher rates of affective symptoms12. Similarly, the results of our study indicate that the prevalence of anxiety and depression in doctors is significantly higher (p=0.000) than that in nurses and other allied staff. This finding is in contrast to a recent study conducted on the mental health status of emergency room (ER) staff during corona outbreak in China, which concluded that being a nurse was associated with a higher risk of post-traumatic stress disorder13.
The higher psychological impact of Covid-19 on doctors can be attributed to the higher level of responsibility on their shoulders but another reason could be the fact that doctors can express their opinions more freely than junior paramedical staff13. Despite the anonymity of the survey, many staff were worried that their dissatisfaction with hospital arrangements may reflect poorly on their commitment to their duties. Further studies can be done to remove possible confounding factors and strengthen the authenticity of the responses.
More than a third of our participants stated that their family and friends were avoiding them due to their Covid-19 exposure. This can take a heavy toll on the mental status of any individual, more so on someone who is undergoing physical and mental stress due to their daily job duties. This stigma associated with Covid-19 clinical staff takes a massive toll on the healthcare worker’s mental wellbeing and is not only in Pakistan but is seen globally. A study conducted in the US evaluated the stigma associated with healthcare workers and results showed that over a quarter of respondents believed that medical staff should have severe restrictions placed on their freedoms, such as being kept in isolation from their communities and their families14.
Therefore, it is the responsibility of the hospital administration to maintain the physical and mental wellbeing of their staff particularly the frontline healthcare workers. Appropriate working hours with timely breaks and sufficient personal protective equipment (PPE) provision will help them to overcome anxiety and depression because in our study these were the significant contributors.
Although healthcare workers are expected to risk their own lives while caring for infectious patients, it is essential to acknowledge the vulnerability of their mental health. Along with appreciation and recognition, psychological evaluation is necessary for medical professionals specifically in high-risk settings. Healthy discussions about anxiety and depression should be encouraged and healthcare workers must get maximum support.
The authors would like to acknowledge the medical and paramedical staff of Dr. Ziauddin Hospital, Clifton campus for their support in completing the study.
The authors declare no conflict of interest.
Ethics approval was obtained from the Institutional Review Committee with the ERC Reference code: 2230520UGMED.
Participants’ consents were obtained in both English and Urdu.
KAP content was conceptualized by UG and MORK whereas SA, and EM, collected the data. SA wrote the manuscript and SS contributed in statistical analysis and results interpretations. All authors have read and approved the final manuscript.
- Cox CL. ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. J Med Ethics. 2020;46(8):510-513.
- Cocker F, Joss N. Compassion fatigue among healthcare, emergency and community service workers: A systematic review. Int J Environ Res Public Health. 2016;13(6):1-18.
- Shah K, Chaudhari G, Kamrai D, Lail A, Patel RS. How essential is to focus on physician’s health and burnout in coronavirus (COVID-19) pandemic? Cureus. 2020;12(4)1-3.
- Husain N, Chaudhry N, Tomenson B, Jackson J, Gater R, Creed F. Depressive disorder and social stress in Pakistan compared to people of Pakistani origin in the UK. Soc Psychiatry Psychiatr Epidemiol. 2011;46(11):1153-1159.
- Nisar M, Mohammad RM, Fatima S, Shaikh PR, Rehman M. Perceptions pertaining to clinical depression in Karachi, Pakistan. Cureus. 2019;11(7)1-12.
- Ahmad W, Taggart F, Shafique MS, Muzafar Y, Abidi S, Ghani N, et al. Diet, exercise and mental-wellbeing of healthcare professionals (doctors, dentists and nurses) in Pakistan. Peer J. 2015;3:1-13.
- Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: Rapid review of the evidence. Curr Psychiatry Rep. 2020;22(8):1-22.
- Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020;148:1-7.
- Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-565.
- Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. 2020;66:1-8.
- Atif K, Khan HU, Ullah MZ, Shah FS, Latif A. Prevalence of anxiety and depression among doctors; the unscreened and undiagnosed clientele in Lahore, Pakistan. Pak J Med Sci. 2016;32(2):294-298.
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;92(2021):245-245.
- Song X, Fu W, Liu X, Luo Z, Wang R, Zhou N, et al. Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav Immun. 2020;88:60-65.
- Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJ. Fear and avoidance of healthcare workers: An important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. 2020;75:1-6.
