By Tayyaba Anwar1, Heena Rais1, Saba Safdar1, Shaista Ehsan2
AFFILIATIONS:
- Department of Pediatrics Medicine, Ziauddin Hospital (Kemari Campus).
- Department of Pediatrics, Ziauddin Hospital (Clifton Campus), Karachi, Pakistan.
ABSTRACT
Background: Dengue is the commonest arboviral disease that is endemic in our country. Electrolyte imbalance is commonly encountered in this disease. There had been only a few worldwide research studies investigating at all the metabolic parameters of dengue infection. Therefore, the study aimed to assess the electrolyte imbalance and its correlation with the severity of dengue fever in pediatrics.
Methods: This cross-sectional study was carried out in the Pediatric Department of Ziauddin Hospital over 18 months. Diagnosed patients through detection of Dengue NS1 antigen or serology of dengue fever from 6 months to 18 years of age were enrolled and their history, hematological and electrolyte values (sodium, potassium, calcium, magnesium, and phosphate) were analyzed. Data was analyzed by SPSS and a Chi-squared test was used to compare the frequency of electrolyte disturbances between patients. A p-value <0.05 was considered statistically significant.
Results: A higher incidence of dengue fever was observed in the younger age group (81)54 %. The majority of the patients showed mild hyponatremia 82(54.6%), mild hypokalemia 63(42%) and hypocalcemia 96(64 %). Hypophosphatemia 98(65.3 %) (p-value 0.045) was found more compared to hypomagnesemia 22(14.6%). Fever was observed in 100% of patients along with body aches 90(60%), drowsiness 31(20.7%) and abdominal pain 16(10.7%). We also found leucopenia 48(32%) and thrombocytopenia 127(84.6%), whereas hematocrit 30(20 %) was also raised.
Conclusion: Majority of electrolytes (sodium, potassium, calcium and phosphate) were found decreased in dengue patients. However, hyponatremia (p=0.001) and hypophosphatemia (p=0.045) were significantly associated to the severity of dengue.
Keywords: Dengue; Severe Dengue; Electrolytes; Hyponatremia; Hypokalemia.
Corresponding Author:
Dr. Tayyaba Anwar
Department of Pediatric Medicine,
Ziauddin Hospital (Kemari Campus),
Karachi, Pakistan.
Email: [email protected]
Dengue is an arthropod borne viral infection transmitted by Aedes. Following malaria, it is the second most serious vector borne disease worldwide1. According to WHO, 50 million infections occur annually and more than 2.5 billion people living in endemic areas are at risk of acquiring infection2. Dengue fever is well known for its epidemics particularly in Southeast Asia and is one of the main sources of death in this locale. In Pakistan, the first case was reported in 1985and 52 485 cases including 91 deaths were reported in 2019 out of which the majority 41 of the deaths were from Sindh3,4. In recent times, National Institute of Health (NIH) issued a “high alert” in Pakistan as the monsoon season is considered as a period of high risk for the spread of dengue5. The spectrum of Dengue ranges from flu like illness to severe dengue with intense signs and symptoms of plasma leak progressing to shock, which contains a high threat of morbidity and mortality3. Dengue fever generally progresses to a severe disease commonly after secondary contamination with a disparate serotype.
Electrolyte imbalance is a frequent complication of dengue. Different electrolytes have variable prevalence in different parts of the world. The prevalence of hyponatremia in dengue is ranging from 11% to 58% globally6,7. Hypokalemia is reported in 11% 7 including case reports of acute hypokalemic quadriparesis complicated with hypomagnesemia8. The prevalence of hypocalcemia is stated to be 86.9% 9. In view of this variable data, it is high time to determine the trend of electrolyte imbalance in dengue in the pediatric population of the Pakistani community to improve outcome and better management in different settings. Therefore, this study aimed to evaluate the electrolyte imbalance in the patients and its correlation with the severity of dengue fever in pediatrics.
This cross-sectional study was carried out in pediatric department of Ziauddin Hospital Karachi. Over the study period from April 2018 to August 2019, a total of 150 patients between 6 months to 18 years of age diagnosed with dengue fever by NS1 or IgM ELISA were included for analysis. All patients who satisfy our inclusion criteria went through clinical examination and investigations after informed consent was taken. The study was ethically approved by the institutional (ERC: 0230518HRPED). The exclusion criteria included children with vomiting and diarrhea, those who had signs of symptoms of rickets or with other concomitant chronic conditions like diabetes mellitus, Addison disease, renal tubular acidosis, barter syndrome, and diabetes insipidus or children with height and weight less than 5th centile according to age.
The data collection included the patient’s demographic details, clinical history, and blood investigations (hemoglobin, white blood cell count, platelet count and hematocrit) and serum level of electrolytes (sodium, potassium, calcium, magnesium and phosphorus) was also observed.
Hyponatremia was defined as serum sodium levels less than 135mEq/L; and hyponatremia was graded as Mild: between 130-134mEq/L; Moderate: between 125-129; mEq/L; Severe hyponatremia: less than 125 mEq/L while hypernatremia was classified as >145 mEq/L. Similarly, hypokalemia was defined as serum potassium levels less than 3.5 mEq/L; and graded as Mild hypokalemia: 3.1 to 3.4mEq/L; Moderate Hypokalemia: 2.50 to 3.0 mEq/L and Severe hypokalemia: less than 2.50 mEq/L. While, hyperkalemia reported as serum potassium level more than 5.0 mEq/L. Normal range of chloride was 96-105 mEq/L. Hypocalcemia was defined as <8.5 mEq/L and hypercalcemia as >10.5 mEq/L, hypomagnesemia as <1.5 mg/dL and hypermagnesemia as >2.5 mg/dL. Normal range of phosphorus was 4.5mg/dl to 6.5mg/dL10. Data were analyzed using SPSS version 22 and descriptive statistics were used to describe the results. A Chi-squared test was used to compare the frequency of electrolyte disturbances between patients with dengue fever and severe dengue. A p-value <0.05 was considered statistically significant.
A total of 150 patients diagnosed with dengue fever were included for analysis. Total, (91) 60.7% were dengue NS1 positive, (21) 14% showed IgM positive whereas (38) 25.3% were both IgM and IgG positive. Of the patients studied majority of the patients i.e. (81)54 % belonged to the age group of 1-5 years, (37)24.7 % 5-10 of years of age and (32)21.3 % of 10-18 years. As thrombocytopenia is a common clinical feature in dengue fever, we also observed the frequency of thrombocytopenia in different age groups. Thrombocytopenia was more frequently seen in the younger age compared to older patients (Figure 1).

Figure 1: Age categories of the patients in association with thrombocytopenia.
Out of 150 patients, 83 were males and 57 were females. Patients with dengue fever were assembled into two categories named dengue fever and severe dengue fever according to WHO guidelines11. Furthermore, 74% (111) of the patients belonged to dengue fever and 26% (39) had severe dengue fever. Fever was the most prominent clinical feature that was present in 100% of cases. Along with fever, most common symptoms encountered in our patients were body aches in 60% (90), lethargy, drowsiness in 20.7% (31) and abdominal pain in 10.7% (16), whereas muscle weakness and respiratory distress were seen only in 4.7% (7) and 4% (6) respectively.
Hemoglobin levels ranged between 4.5-15.3 g/dl and the mean was 11.2 g/dl. Leucopenia was observed in 32% (48) of patients. The majority of the patients had thrombocytopenia. Out of which 16 had a platelet count in the range of 20,000-50,000 and only two had severe thrombocytopenia of < 20,000. Hematocrit was raised in 20 % (30) of patients.
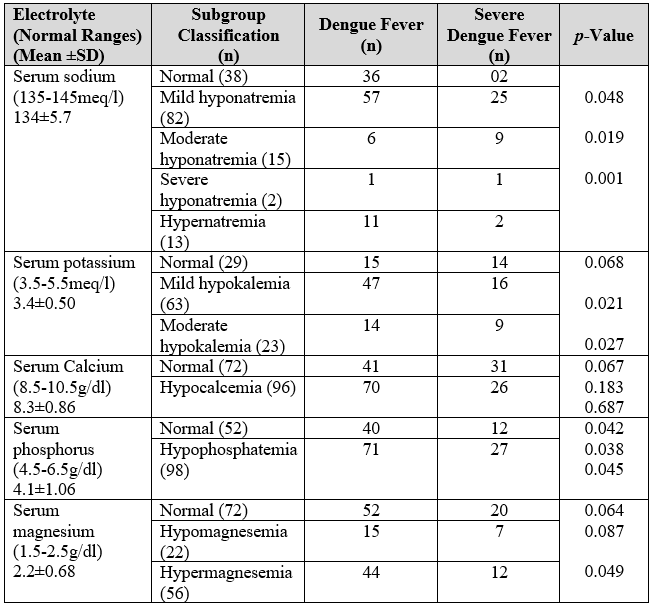
In our study, serum electrolyte levels were analyzed (Table 1). Mean value of sodium was 134.2 mEq/L. Hyponatremia was documented in 66% (99) of patients (p-value 0.001). Out of these 99 patients, 54% (82) had mild hyponatremia, 10% (15) had moderate hyponatremia and 1.3% (2) depicted severe hyponatremia. In addition, 57.3 % of the patients showed hypokalemia (p-value 0.027). Out of which 42% (63) had mild hypokalemia and only 15% (23) had moderate hypokalemia. None of the patients had severe hypokalemia. Further, 42.7% (64) of the patients had serum potassium levels within the normal range. Mean value of potassium was 3.4mEq/L. Serum chloride levels were normal in 100% of the patients.
Mild hyponatremia was predominant in dengue fever (p-value 0.048) whereas moderate hyponatremia was seen preeminently in severe dengue (p-value 0.0119). Hypokalemia (mild and moderate) was prevalent in dengue fever as compared to severe dengue (p-value 0.068 and 0.021 respectively). Since, 64% (96) of the patients had hypocalcemia (p-value 0.687) although the mean calcium level was 8.4mEq/l. Out of 96 patients 70 had dengue fever and 26 had severe dengue (p-value 0.067 and 0.183 respectively). The majority of the patients in our study showed hypophosphatemia (p-value 0.045), 71 in dengue fever (p-value 0.042) and 27 in severe dengue (0.038). Hypermagnesemia was predominant compared to hypomagnesemia. It was seen in 44 patients with dengue fever and 12 patients with severe dengue (p-value 0.064 and 0.087 respectively).
Table 1: Serum electrolytes level with respect to number of cases among dengue patients.
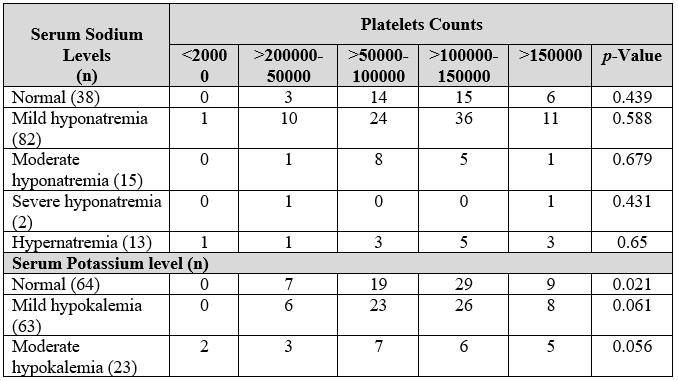
We also determined the relationship of thrombocytopenia (Table 2) with the most frequently found electrolyte imbalance i.e., sodium and potassium.
Table 2: Serum electrolytes level with respect to platelets count among dengue patients.
Electrolyte imbalance including hyponatremia along with hypokalemia, hypocalcemia and hypophosphatemia was found frequently in majority of our dengue patients. Sodium regulates the PH, osmotic equilibrium and blood pressure. There was a marked decrease in serum sodium levels of the current study patients which is a risk factor of developing convulsions in infants and young children12,13. There is 9.7 % increased risk of developing hyponatremia in dengue fever14. Hyponatremia was documented in 66% of our patients similar to Caroline et al.15 but it was much higher than Mekmullica et al. they found it to be 18 % 14. Reddy et al. found that there is a direct correlation of hyponatremia with complications of dengue fever and it can be used as a prognostic marker in such patients16. Serum sodium levels were significantly lower in severe dengue patients as compared to dengue fever patients (p-value 0.019 and 0.048 respectively)
Hypokalemia has also been reported in dengue fever probably because of decreased dietary consumption and release of potassium into extracellular compartment because of tissue breakdown17. Researchers like Kalita et al. reported many infectious diseases to show hypokalemia, especially Dengue fever18. Khandelwal et al.,7 and Poornima et al.19 reported hypokalemia in 42% and 39% of patients respectively. Our study also exhibits mild hypokalemia in 42 and moderate hypokalemia was reported in 15% of patients. Our study population failed to exhibit severe hypokalemia probably because most of the patients fell in the category of dengue fever although two of our patients presented initially with fever and body aches rapidly progressed to quadriparesis with significant hypokalemia and improved markedly after potassium administration. Hypokalemic quadriparesis complicated by hypomagnesemia has also been reported in the past8. Our study revealed hypomagnesemia in 14.7% of the patients however, hypermagnesemia was seen in 37.3%, which has never been reported in the past. As this is a new finding in dengue fever, further studies need to be done to know the exact incidence and cause of hypermagnesemia in dengue fever.
Hypocalcemia directly correlates with the severity of dengue fever20,21. Low serum calcium levels were found in 64 % of our study group with mean of 8.4meq/l. Adikari et al. reported hypocalcemia in 85% of patients which is much higher than our value22. Our study depicted 65.3% of population with significant hypophosphatemia (p=0.039). Yasri and Wiwanitkit reported case of myositis in dengue fever in which hypophosphatemia was suspected to be one of the causes of rhabdomyolysis23. We have limited data regarding hypophosphatemia as a predominant feature of dengue fever.
In our study demographic characteristics of the patients were also studied, which showed that dengue fever affected children of 1-5 yrs of age mostly and infants less than 1 year of age were least affected. According to WHO guidelines, 1997 Dengue is a disease of children in which Dengue hemorrhagic fever is more common under 15 years of age. As per WHO, revised guidelines 2009 Young children are more prone to develop severe dengue infection24. Expert groups have proposed that dengue is a disease with multiple clinical presentations, and that affected patients present with a wide range of clinical manifestations that vary according to age and severity of infection11. Some researchers suggested that fever, myalgia and abdominal pain were the presenting symptoms in the majority of the cases with other important features being headache retro-orbital pain, rashes and hepatomegaly25,26. Our study showed similar clinical presentations like lethargy, muscle weakness, abdominal pain and respiratory distress in dengue fever.
The first hematological variation from the norm is a continuous decline in WBC count in patients of dengue fever24. Ralapanawa et al. reported 70.9% of the patients had WBC count of <50000 in dengue fever27. On the contrary, leucopenia was observed in only 32% of the patients in our study, which was supported by the study of Khandelwal and colleague that the majority of the patients had WBC count within the normal range during the early febrile period of the disease and change in leukocyte count show progression towards severe disease28.
Researchers found thrombocytopenia to be the most prominent and consistent feature of dengue fever29,30. Since, 44.7% of the patients were reported to have a platelet count of <100000. The mean platelet count was also decreased 109.5 x 103 in this study. However, we also found that thrombocytopenia is also associated with the most frequently encountered electrolyte imbalance, Sodium and Potassium. Mild hyponatremia and mild hypokalemia were mostly found in dengue fever patients who had thrombocytopenia.
Besides hematological abnormalities, dengue is also associated with dyselectrolytemia. In this study most frequently encountered electrolyte imbalance was hyponatremia, hypokalemia, hypocalcemia and hypophosphatemia and these electrolyte abnormalities especially hyponatremia and hypophosphatemia were directly associated with the severity of dengue. Electrolyte abnormalities can be detected and managed at an early stage to prevent the progression of morbidity as well as mortality. As dengue is becoming endemic in our country and is more prevalent in the pediatric age group, so further studies should be done with specified control groups to provide results that are more relevant statistically.
The authors would like to thank Department of Pediatric Medicine (Kemari and Clifton campuses) and Department of Medicine (Kemari campus) for the assistance during the study specifically in data collection process.
The authors declare no conflict of interest.
Ethical approval was obtained from the institutional ERC (Reference code: 0230518HRPED).
Written patient/attendant consents were taken.
TA performed the literature search, manuscript writing and proof reading. HR performed the critical analysis and manuscript writing. SS performed the data collection, interpretation of data and data entry. SE also performed the data collection and literature search.
- Jing Q, Wang M. Dengue epidemiology. Glob Health J. 2019;3(2):37-45.
- Rehman FU, Omair SF, Memon F, Amin I, Rind BJ, Aziz S. Electrolyte imbalance at admission does not predict the length of stay or mortality in dengue-infected patients. Cureus. 2020;12(9):1-9.
- Syed S, Mahmood Z, Riaz M, Latif S, Majeed N, Rashid A. Elemental profile of blood serum of dengue fever patients from Faisalabad, Pakistan. Int J Biol Sci. 2014;6:34-37.
- World Health Organization. Infection prevention and control of epidemic-and pandemic-prone acute respiratory infections in health care. World Health Organization; 2014. Available from: https://www.who.int/publications/i/item/infection-prevention-and-control-of-epidemic-and-pandemic-prone-acute-respiratory-infections-in-health-care
- Butt MH, Ahmad A, Misbah S, Mallhi TH, Khan YH. Dengue fever and COVID-19 coinfection; a threat to public health for coepidemic in Pakistan. J Med Virol. 2021;93(2):671-672.
- Narasimhan D, Katragadda S. Retrospective analysis of biochemical profile of dengue infection in a tertiary care hospital. Int J Res Med Sci. 2017;5(12): 5218-5220.
- Khandelwal VG, Patil VC, Botre A, Patil R. Study of electrolyte disturbances in dengue infected patients. Int J Contemp Med Res. 2019;6(2)5-8.
- Pushkar D, Roy B, Chawla H, Ahmad T. Acute dengue hypokalemic paralysis complicated by hypomagensemia. J Acute Dis. 2018;7:262-264.
- Constantine GR, Rajapakse S, Ranasinghe P, Parththipan B, Wijewickrama A, Jayawardana P. Hypocalcemia is associated with disease severity in patients with dengue. J Infect Dev Ctries. 2014;8(9):1205-1209.
- Pagana KD, Pagana TJ. Mosby’s diagnostic and laboratory test reference-e-book. 11th Elsevier Health Sciences; 2012. 855 p.
- WHO | Dengue and severe dengue [Internet]. Media Centre World Health Organization; 2020 [cited 2021 Jan 31]. Available from: https://apps.who.int/mediacentre/factsheets/fs117/en/index.html
- Carod-Artal FJ, Wichmann O, Farrar J, Gascón J. Neurological complications of dengue virus infection. Lancet Neurol. 2013;12(9):906-919.
- Verma R, Sahu R, Holla V. Neurological manifestations of dengue infection: a review. J Neurol Sci. 2014;346(1-2):26-34.
- Mekmullica J, Suwanphatra A, Thienpaitoon H, Chansongsakul T, Cherdkiatkul T, Pancharoen C, et al. Serum and urine sodium levels in dengue patients. Southeast Asian J Trop Med Public Health. 2005;36(1):197-199.
- Caroline RJ, Palanisamy A, Vijayarani H. Electrolyte disturbance in dengue infected patients in Salem, Tamilnadu. Int J Adv Pharm Biol Chem. 2014; 3(4): 933-936.
- Reddy AA, Reddy TP, Pranam GM, Pranam U, Manjunathe GA. Serum sodium as a prognostic marker in dengue fever cases admitted to PICU in Navodaya hospital, Raichur, India. Int J Contemp Pediatr. 2017;4:222-225.
- Sarfraz M, Rabbani A, Manzoor MS, Zahid H. Electrolyte disturbances in patients with dengue fever. J Rawal Med Coll. 2018;22:96-98.
- Kalita J, Misra UK, Mahadevan A, Shankar SK. Acute pure motor quadriplegia: is it dengue myositis? Electromyogr Clin Neurophysiol. 2005;45(6):357-361.
- Poornima S, Nithya E, Kavya C. Study on electrolyte disturbances in dengue fever in a tertiary care centre. Int J Contemp Pediatrics. 2019;6(6): 2504-2508.
- Suresh SR, Srikanth AK, Sriharsha K, Harshith CS. Utility of serum free calcium as a predictor of severity in dengue fever. J Evol Med Dent Sci. 2018;7(39):5077-5082.
- Manjunath VG, Balla S, Kumar J. Serum ionic calcium levels and hypocalcemia in dengue fever in children and its correlation with its severity: Case control study. Int J Contemp Pediatrics. 2019;6(3):1-5.
- Adikari M, Perera C, Fernando M, Loeb M, Premawansa S. Prevalence of hypocalcemia and its potential value as a biochemical marker in patients with severe dengue infection. J Trop Dis. 2015;4(188):1-3.
- Yasri S, Wiwanitkit V. Afebrile dengue myositis. Ann Trop Med Public Health [serial online] 2016 [cited 2021 Mar 9]; 9:360. Available from: https://www.atmph.org/text.asp?2016/9/5/360/190204
- World Health Organization, special programme for research, training in tropical diseases, world health organization. Department of control of neglected tropical diseases, world health organization. epidemic, pandemic alert. Dengue: guidelines for diagnosis, treatment, prevention and control. World Health Organization; 2009. 89 p.
- Upadhyay N, Joshi H, Upadhyay C. Thrombo-cytopenia and raised hematocrit-predictor of dengue hemorrhagic fever. Int J Contemp Pediatrics. 2017;4:1322-1324.
- Raghu R, Manokaran C, Sathiyanarayanan J. Clinical profile of dengue fever in a tertiary hospital of rural south India – A retrospective study. Int J Trop Dis Health. 2020;60-69.
- Ralapanawa U, Alawattegama AT, Gunrathne M, Tennakoon S, Kularatne SA, Jayalath T. Value of peripheral blood count for dengue severity prediction. BMC Res Notes. 2018;11(1):1-6.
- Khandelwal RK, Khandelwal LM. Effect of dengue fever on the total leucocyte count and neutrophil count in children in early febrile period. Int J Pediatr Res. 2017;4:617-622.
- Rai A, Azad S, Nautiyal S, Acharya S. Correlation between hematological and serological parameters in dengue patients-an analysis of 2022 cases. Trop J Pathol Microbiol. 2019;5(8): 547-554.
- Yolanda N, Alfan H. Initial clinical and laboratory profiles to predict pediatric dengue infection severity. Paediatr Indones. 2017;57(6):303-309.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
