By Inayat Ali Khan1, Irfan Lutfi2, Muhammad Ali3, Atiq Ahmed Khan4
AFFLIATIONS:
- Department of Neurosurgery, Ziauddin Medical University and Hospital (North), Karachi, Pakistan.
- Department of Interventional Radiology, Ziauddin Medical University and Hospital (North), Karachi, Pakistan.
- Department of Radiology, Ziauddin Medical University, Karachi, Pakistan.
- Department of Neurosurgery, Dow University of Health Sciences, Karachi, Pakistan.
ABSTRACT
Basilar tip aneurysms are the commonest aneurysms of the posterior circulation and constitute around 5-8% of all cerebral aneurysms. Ruptured basilar tip aneurysms may present with signs and symptoms of subarachnoid hemorrhage (SAH) with sudden, extremely severe headache, nausea and vomiting, stiff neck, blurred or double vision, sensitivity to light, seizure, drooping eyelid and loss of consciousness. At times, the hemorrhage could be fatal, reaching mortality beyond 20%. Basilar tip aneurysms have complex anatomy and have always been considered difficult to treat. Two well-known options to treat basilar tip aneurysms include the microsurgical approach and the endovascular approach. Endovascular treatment is now a cost-effective, preferred and logical rationale for the management of intracranial aneurysms. This case reports the first ever coiling procedure that was performed at Ziauddin Hospital (North Campus) for a basilar tip aneurysm and the other major challenge faced at our center was that the neck was wide, hence requiring a supporting balloon.
Keywords: Aneurysm; Subarachnoid Hemorrhage; Cerebral Aneurysms.
Basilar tip aneurysms constitute around 5-8% of all intracranial aneurysms1,2. Surgical clipping is a difficult and risky option with a high risk of increased morbidity3,4. The option of endovascular approach for the treatment of basilar tip aneurysms using detachable coils is a straightforward procedure and does not differ from that of aneurysms in other locations5,6. Coiling procedures do have disadvantages like coil migration or compaction of the coil mesh itself 7. Although the threat of reopening of the lumen may be there, still coiling especially with ballooning would always be the preferred choice8,9.
A 46-year-old male patient was brought to the emergency room (ER) of Ziauddin hospital (North campus) with a history of severe/splitting headache, vomiting, double vision and altered level of consciousness. There was no history of head trauma. The patient was stabilized in the ER and an urgent CT (Computerized tomography) scan of the brain was done which revealed diffuse subarachnoid hemorrhage (SAH) with severe brain edema (Figure 1a).
The family was counseled regarding the chances of a suspected aneurysmal bleed and necessitating an urgent cerebral angiography. Hence, a 4-vessel digital subtraction angiography (DSA) was done which revealed a large wide neck basilar tip aneurysm (Figure 1b and 1c).
The anatomic location and the relationship of the aneurysm to neighboring structures were taken into consideration and the possibilities of clipping versus endovascular coiling were considered. Both options with their relative risks and benefits were discussed with the family and the coiling option was accepted as the procedure of choice.
This was going to be the first ever coiling procedure for an aneurysm of the posterior circulation; hence, the interventional radiologist (IR) was wary of the challenge with the additional fact that this patient also needed a supporting device (balloon) for the wide neck without which the chances of successful coiling would not have been possible.
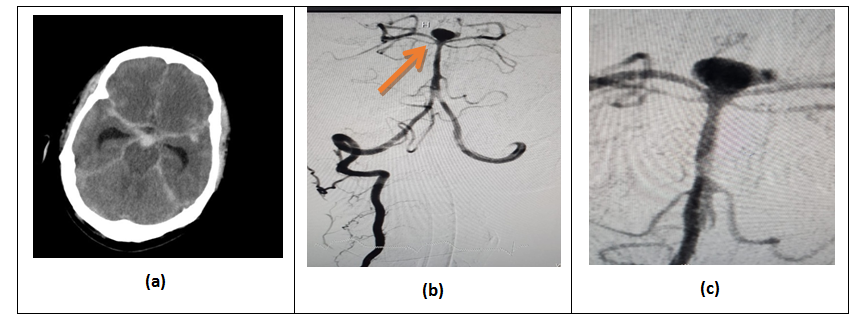
Figure 1a: CT brain showing diffuse subarachnoid hemorrhage (SAH); b: digital subtraction angiography (DSA) reveals a basilar tip aneurysm (arrow); c: A zoom in image of the aneurysm.
As is already known, coiling of basilar tip aneurysms is not new to the world of neurosurgery and interventional radiology. Coiling of wide neck aneurysms of the posterior circulation have always been a daunting task. Coiling of basilar tip aneurysms (BTAs) is a procedure, which is not new to the world of neurosurgery or the interventional radiologist in general. This procedure (Figure 2a and 2b) was performed for the first time at Ziauddin hospital (North campus); it was a bit more challenging because this aneurysm in particular had a wide neck.
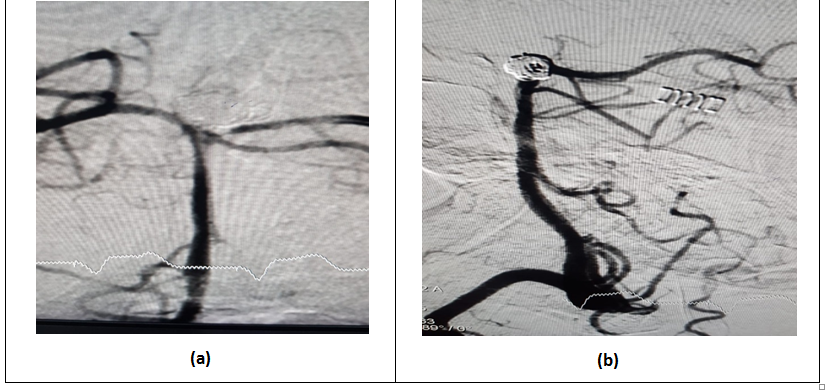
Figure 2a: DSA post-coiling image; b: oblique/lateral image-post coiling.
It was performed under general anesthesia with an infusion of systemic heparinisation. The objective was to densely pack the aneurysm with coiling such that not a single additional coil could be placed to obtain complete occlusion. Our patient was discharged home on the third post-coiling day in good health and with stable vitals. Hence, a breakthrough at Ziauddin hospital (North) was registered with the first ever coiling of a posterior circulation aneurysm (in this case a basilar tip with a wide neck). The patient is being followed up regularly in the outpatient, fully ambulant, conscious, no symptoms of headache, excellent appetite.
The general principles of commonality, risk factors and ruptures that apply to basilar tip aneurysms are similar to the rest of the cerebral aneurysms. The main risk factors for basilar tip aneurysms include sedentary life, high calorie diet, sleeplessness, obesity, hypertension, chronic obstructive pulmonary disease, high cholesterol and atherosclerosis10. Basilar tip aneurysms are the commonest aneurysms of the posterior circulation and account for at least 5-8% of all intracranial aneurysms. Clinical findings usually are those associated with SAH, although bitemporal hemianopsia or an oculomotor palsy may occur along with a low Glasgow coma score2.
Ruptured basilar aneurysms can at times be devastating as far as survival is concerned, they do however present with signs and symptoms of SAH. That may include sudden, extremely severe headache, which at times could be referred to as the “worst headaches of my life” by the patient, nausea and vomiting and blurred, or double vision sensitivity to light, seizure, drooping eyelid, loss of consciousness and confusion. 10% to 43% of patients with SAH report experiencing a sentinel headache in the 2 months preceding the rupture. Ruptured basilar tip aneurysms may result in fatal subarachnoid hemorrhage (SAH) and mortality could be as high as 23% 2.
At our center, diagnostic imaging for suspected aneurysms included CT (computerized tomography) angiography (CTA) and digital subtraction angiography (DSA). Once a SAH is noted on a plain CT scan, DSA becomes the first diagnostic modality of choice. In this particular patient, CT brain was done in the emergency department and after a clear suspicion of SAH secondary to a basilar tip aneurysm rupture, we proceeded for a DSA. Basilar tip aneurysms pose a special challenge. For a long time clipping, the aneurysm surgically had been the only practical solution but came with a price of significant morbidity5. However, the introduction of detachable coils has brought new hope to our patients and it has significantly facilitated the management of basilar tip aneurysms11. Detachable coils became available in the 1990s and with the arrival of detachable coils, surgical treatment for the same has become almost negligible, the reason being that technically coiling of basilar tip aneurysms is usually not different from that of other locations10.
Owing to the proximity of the brainstem, difficulty in obtaining adequate exposure and crowding of arteries in this region, surgical clipping for basilar tip aneurysms remains a challenge and the procedure-related mortality and morbidity could be 9% and 19.4% 12. Surgical techniques (for large and giant aneurysms, even those with wide necks) such as direct clipping under hypothermia with circulatory arrest and bypass surgery are no more serious treatment alternatives for coiling at most centers around the globe8. Whenever we talk about a large neck or a wide neck aneurysm, it is obvious that the aneurysm is a giant aneurysm, which was the case in our patient under discussion. Wide necks are always considered as an unfavorable anatomic feature for the plain reason that it becomes even more difficult to obtain satisfactory occlusion. Incomplete occlusions always have the potential of loose packing which may not fully prevent blood flow into the aneurysmal residual sac. Hence coiling of such patients is very challenging because it is not only technically very difficult in fact; coil herniation later could be a possibility13.
The best way to overcome this difficulty would be to use supporting devices that would prevent the herniation of such coils. Supporting balloons have been available since the 1990s; the use of a supporting device may make the coiling process more complex, with a possibility of increased morbidity. The encouraging fact however is that studies have reported low morbidity for the same procedure when compared to basilar tip aneurysms of all sizes9. Still supporting balloons are the present day answer to this problem of imminent threat of coil herniation in the parent artery, the other option being intracranial stents14.
After successful coiling, a major threat would be rebleeding from a coiled aneurysm and another possibility would be reopening of the aneurysm15. Studies however generally show that the vast majority of coiled aneurysms that have been adequately occluded tend to remain adequately occluded even at 6 months follow-up angiography16. Now basilar tip aneurysms with a wide neck and a size ≥ 10 mm may reopen late (even after 6 months), to tackle this problem extended follow up imaging may be considered17.
Imaging follow-up is always an ongoing process. A follow-up imaging is recommended to be done at 6 months after the coiling procedure. This time is appropriate enough to catch up with an early coil herniation or reopening of the aneurysm. Besides the fact that an aneurysm may have been stable and completely occluded, reopening has still been reported after 8 years. Now instead of angiography, the patient can be followed up with a high resolution magnetic resonance angiography (MRA)18, 19.
Coiling of Basilar tip aneurysms is a very effective and safe procedure even with all the anatomic challenges. The major confrontation is when this aneurysm has a wide neck, which may allow coil migration. Hence ballooning, which helps to hold the coil in place is highly recommended. Balloon assisted coiling is very efficacious with a very low complication rate. Still, such patients need to be followed up by angiography to detect any reopening.
The authors fully acknowledge the entire team of the hospital that was involved in the special care of patient and facilitated us at all stages of patient management.
The authors declare no conflict of interest.
Detailed written (high-risk) consent was taken from the family of the patient (as the patient himself was on a ventilator) after fully counseling them about the risks and benefits of the procedure and the possible negative outcome that may follow.
All the authors fully contributed to the critical write-up of this case report.
- Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Eng J Med. 2006;355(9):928-939.
- Schievink WI, Wijdicks EF, Piepgras DG, Chu CP, O’Fallon WM, Whisnant JP. The poor prognosis of ruptured intracranial aneurysms of the posterior circulation. J Neurosurg. 1995;82(5):791-795.
- Ge H, Lv X, Jin H, Tian Z, Li Y, He H. The role of endovascular treatment in unruptured basilar tip aneurysms. Interv Neuroradiol. 2017; 23(1): 8-13.
- Ogilvy CS, Hoh BL, Singer RJ, Putman CM. Clinical and radiographic outcome in the management of posterior circulation aneurysms by use of direct surgical or endovascular techniques. Neurosurg. 2002;51(1):14-22.
- Lusseveld E, Brilstra EH, Nijssen PC, van Rooij WJ, Sluzewski M, Tulleken CA, et al. Endovascular coiling versus neurosurgical clipping in patients with a ruptured basilar tip aneurysm. J Neurol Neurosurg Psychiatry. 2002;73(5):591-593.
- Sluzewski M, Van Rooij WJ, Beute GN, Nijssen PC. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg. 2006;105(3):396-399.
- Sluzewski M, van Rooij WJ, Slob MJ, Bescós JO, Slump CH, Wijnalda D. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiol. 2004;231(3):653-658.
- Evans JJ, Sekhar LN, Rak R, Stimac D. Bypass grafting and revascularization in the management of posterior circulation aneurysms. Neurosurg. 2004;55(5):1036-1049.
- Van Rooij WJ, Sluzewski M. Coiling of very large and giant basilar tip aneurysms: midterm clinical and angiographic results. Am J Neuroradiol. 2007;28(7):1405-1408.
- International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms—risk of rupture and risks of surgical intervention. N Eng J Med. 1998;339(24):1725-1733.
- Lozier AP, Connolly Jr ES, Lavine SD, Solomon RA. Guglielmi detachable coil embolization of posterior circulation aneurysms: a systematic review of the literature. Stroke. 2002;33(10):2509-2518.
- Henkes H, Fischer S, Weber W, Miloslavski E, Felber S, Brew S, et al. Endovascular coil occlusion of 1811 intracranial aneurysms: early angiographic and clinical results. Neurosurg. 2004;54(2):268-285.
- Sluzewski M, Van Rooij WJ, Beute GN, Nijssen PC. Balloon-assisted coil embolization of intracranial aneurysms: incidence, complications, and angiography results. J Neurosurg. 2006;105(3):396-399.
- Kis B, Weber W, Berlit P, Kühne D. Elective treatment of saccular and broad-necked intracranial aneurysms using a closed-cell nitinol stent (Leo). Neurosurg. 2006;58:443-450.
- Ferns SP, Sprengers ME, van Rooij WJ, Rinkel GJ, van Rijn JC, Bipat S, et al. Coiling of intracranial aneurysms: a systematic review on initial occlusion and reopening and retreatment rates. Stroke.2009;40:523-529.
- Sluzewski M, Menovsky T, van Rooij WJ, Wijnalda D. Coiling of very large or giant cerebral aneurysms: long-term clinical and serial angiographic results. Am J Neuroradiol. 2003;24:257-262.
- Schaafsma JD, Sprengers ME, van Rooij WJ, Sluzewski M, Majoie CB, Wermer MJ, et al. Long-term recurrent subarachnoid hemorrhage after adequate coiling versus clipping of ruptured intracranial aneurysms. Stroke. 2009;40:1758-1763.
- Majoie CB, Sprengers ME, van Rooij WJ, Lavini C, Sluzewski M, van Rijn JC, et al. MR angiography at 3T versus digital subtraction angiography in the follow-up of intracranial aneurysms treated with detachable coils. Am J Neuroradiol. 2005;26(6):1349-1356.
- Raymond J, Guilbert F, Roy D. Neck-bridge device for endovascular treatment of wide-neck bifurcation aneurysms: initial experience. Radiol. 2001;221:318-326.
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
