By Humera Nasim1, Madiha Ehtesham1, Saima Ambreen1, Muhammad Arif 1, Muhammad Kamran Khan1, Aqsa Naseer 2, Faizan Fazal 3, Tayyaba Saleem 3, Mohammad Ebad Ur Rehman3
- Department of Medicine, Holy Family Hospital, Rawalpindi, Pakistan.
- Department of Gastroenterology, Holy Family Hospital, Rawalpindi, Pakistan.
- Rawalpindi Medical University, Rawalpindi, Pakistan.
DOI: https://doi.org/10.36283/PJMD12-2/008
How to cite: Nasim H, Ehtesham M, Ambreen S, Arif M, Khan MK, Naseer A, et al. Risk Factors and Secondary Infections in Dengue Hemorrhagic Fever Patients. Pak J Med Dent. 2022;12(2): 43-49. doi: 10.36283/PJMD12-2/008
Background: Dengue hemorrhagic fever (DHF) is a fatal manifestation of dengue disease. DHF’s risk factors profile holds significance importance in the clinical practice and efficient care plan are required during dengue disease flare-up. The aim of this study was to investigate the risk factors for pathogenesis of dengue disease and dengue hemorrhagic fever.
Methods: In this descriptive cross-sectional study, data was obtained from 256 patients with diagnoses of Dengue hemorrhagic fever (DHF). Comprehensive history, physical assessment and biochemical estimations were recorded. Patients were followed to identify and assess the risk factors for DHF. The Statistical Package of Social Sciences for analysis of data. Stratification of residence and socioeconomic status to see effect of these on result variable by applying chi square test. p value of <0.05 was taken as significant.
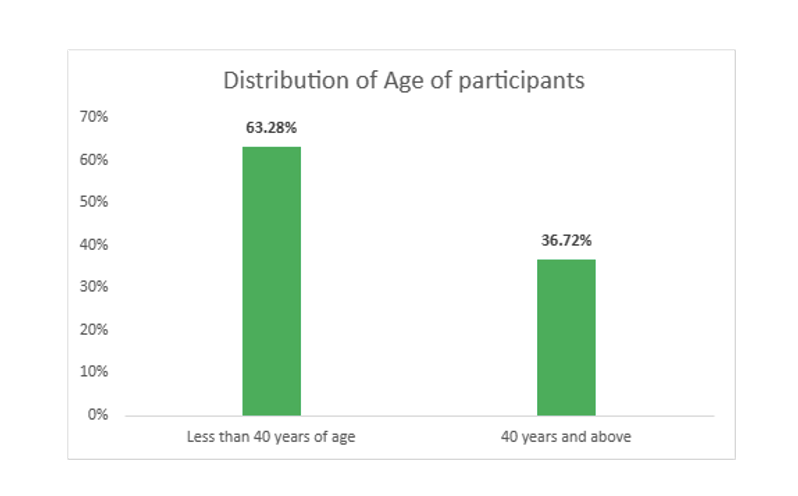
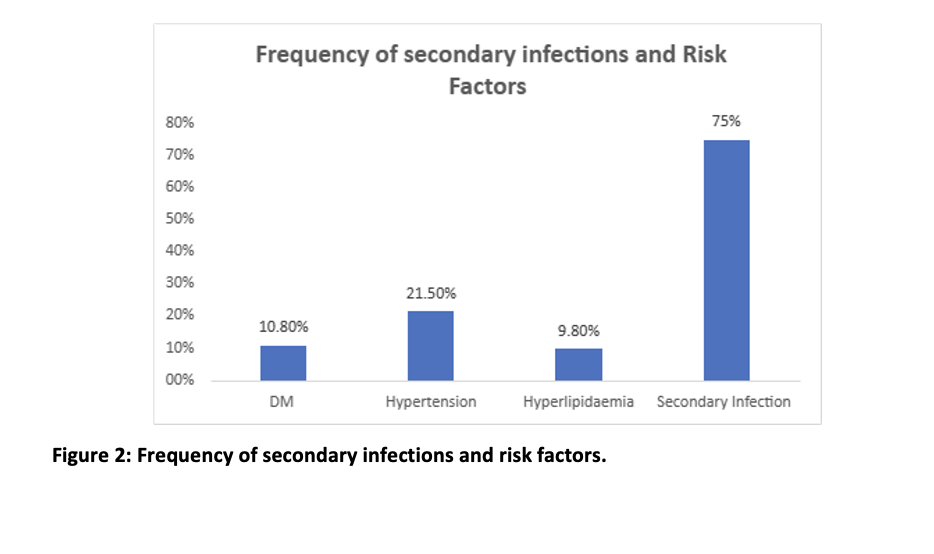
Results: Among the 256 patients, the mean age of the age (Mean±SD) of study population was 28.4±12.1 years, 162 (63.28%) were less than 40 years of age and 94 (36.72%) were ≥40 years. The males were 181 (70.70%) and females were 75 (29.30%). The frequency of risk factors was observed to be 26 (10.8%) patients had Diabetes Mellitus, 55(21.5%) hypertension, 25(9.8%) hyperlipidemia. Secondary infection occurred in 192 (75%) but results were insignificant (p>0.05). All diseases were common in participants who belonged to the urban area.
Conclusion: Secondary infection was most common risk factor in patients with DHF and found mostly in less than 40 age than older patients. Whereas, males were predominately affected more than the females (p<0.05).
Keywords: Severe Dengue, Dengue Hemorrhagic Fever, Risk Factor.
Dengue is a mosquito spreader disease mostly found in tropical and sub-tropical locales of more than 100 nations1. Two-fifths of the total population or 2500 million individuals are presently in danger of dengue, and roughly 50 million new cases happen overall2. The worldwide commonness of dengue disease has expanded drastically in late decades, especially in America, Western Pacific, and Southeast Asia3.
Dengue hemorrhagic fever (DHF), a conceivably deadly appearance of dengue contamination, was first perceived during the 1950s during dengue disease in the Thailand and Philippines. Today, DHF in South Asia causes a critical number of deaths. The identification of danger variables of DHF has its suggestions for clinical practice4. It enables the doctors to organize care during a flare-up of dengue contamination. Furthermore, it offers a sign to the investigation of the pathogenesis of dengue contamination.
Epidemiological danger variables of dengue hemorrhagic fever, for example, age and gender were distinguished in some studies. Co-morbidities has reported as being a risk for DHF in several studies from dengue-affected areas and countries. The effect of age on dengue hemorrhagic fever infection studied by analysis showed that infants and children had higher chances of developing DHF. One study showed about 60% of patients were below 30 years5.
The male gender is also associated with a relatively greater risk of dengue hemorrhagic fever. One study showed that about 67.8% of the patients were males6. The secondary disease has been all around perceived as the more forceful type of dengue contamination. Wichmann et al. in their examination indicated that auxiliary dengue contamination was essentially connected with the improvement of DHF in grown-ups. Practically 87% of patients had auxiliary contamination7.
Co-morbidities, for example, hypertension, diabetes mellitus and hyperlipidemia are among the couple of driving reasons for mortality and dismalness in Asia. Notwithstanding, the pathophysiology behind diabetes prompting DHF results is not surely known at this point, even though various examinations have proposed that diabetes mellitus can bring about invulnerable and endothelial brokenness. One study has shown the prevalence of hypertension, diabetes and hyperlipidemia as 11.2%, 6.4% and 8.5% much more than their normal counterparts6.
Dengue hemorrhagic fever is a serious type of dengue. Different DHF peril factors had been proposed. Be that as it may, these dangerous elements may not be summed up to all populations. Distinguishing hazard factors for DHF can encourage early clinical, preventive and medical care assets for the executives. Therefore, this study aimed to investigate the risk factor for the pathogenesis of dengue disease and dengue hemorrhagic fever.
This Descriptive Cross-Sectional Study was held at the Department of irresistible illnesses, Holy Family emergency clinic, Rawalpindi between June 2016 to November 2016. Inclusion criteria were patients of both sexes diagnosed with Dengue hemorrhagic fever (DHF) over 14 years old and ≤ 70 years. The exclusion criteria for this study were patients diagnosed with dengue fever, not meeting the criteria of DHF and patients with known co-morbids like a renal disappointment (serum Cr> 3mg/dl), cardiovascular breakdown (EF < 30% on echocardiography) known danger (affirmed on biopsy report), cirrhosis of liver and hypoalbuminemia. The study was conducted after Ethical approval was obtained from the ethical reviewal board of the hospital. This examination was led after the endorsement from the Holy family clinic moral survey advisory group. The patients satisfying the inclusion criteria were chosen by successive inspecting techniques from the division of irresistible sicknesses of Holy family emergency clinic, Rawalpindi. Composed consent was taken from the infected. For the conclusion of various risk variables of DHF, a detailed pertinent history was obtained and a careful physical assessment was performed.
After history and examination, investigations were performed for each patient including hematocrit, total leukocyte count, platelets count, serum IgM, IgG for dengue, and ultrasound abdomen and chest.
The information regarding the patient’s presentation was collected on a structured self-made questionnaire to combine data for all the patients. All the information was entered and examined through the Statistical Package of Social Sciences (SPSS v 22). For age Mean and SD were determined. Recurrence and rates were determined for absolute factors like sexual orientation, age gathering, and presence or nonattendance of risk factors I-e optional contamination DM, HTN, and hyperlipidemia. Effect modifiers were controlled through stratification of residence and socioeconomic status to see the effect of these on the result variable by applying the chi-square test. A p-value of <0.05 was taken as noteworthy.
A total of 256 patients were investigated and the mean ± standard deviation of the age study population was 28.48+12.1 years. On analysis of the demographics profile, it was observed that 181 (70.70%) were males and 75 (29.30%) were females. According to the pattern of age distribution in this study, 162 (63.28%) were below 40 years of age and 94 (36.72%) were of age 40 years and above (Figure 1).
On analyzing the frequency of risk factors, it was observed that 26 (10.8%) patients had diabetes mellitus, 55 (21.5%) had hypertension, 25 (9.8%) had hyperlipidemia and 192 (75%) had a secondary infection. Secondary infection was the most common and significant risk factor observed in this study. This is shown in Figure 2.
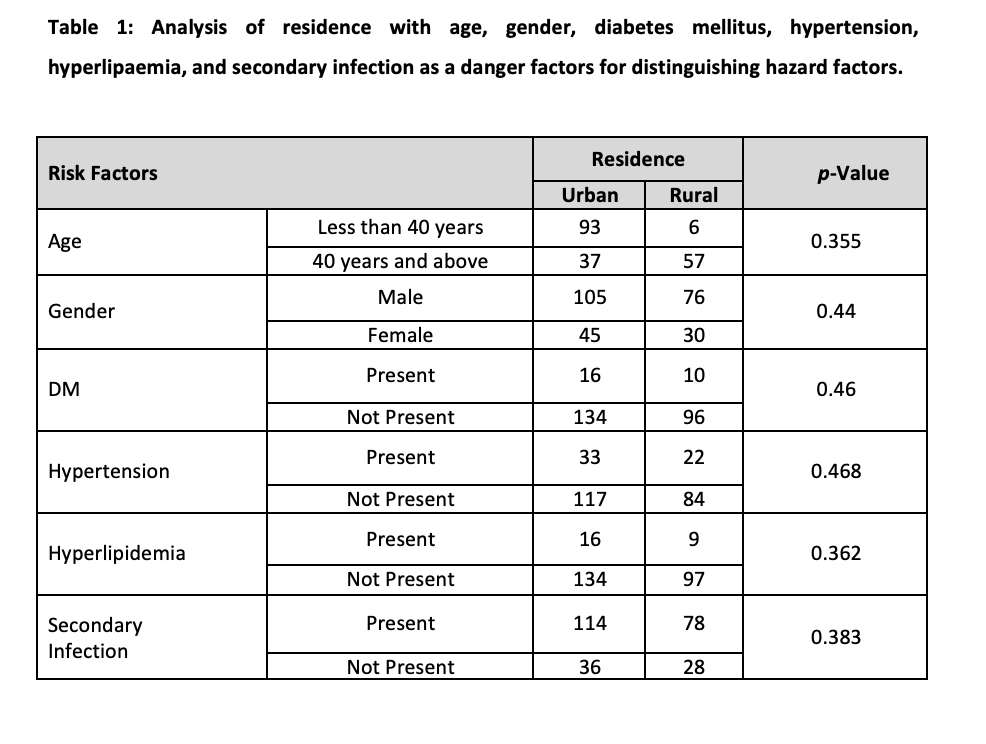
Analysis of residence with age, gender, diabetes mellitus (DM), hypertension, hyperlipaemia, and secondary infection as a danger factor for distinguishing hazard factors have been given in Table 1. According to this data, diabetes, hypertension, hyperlipidemia and secondary infection were more common in participants who belonged to the urban area.
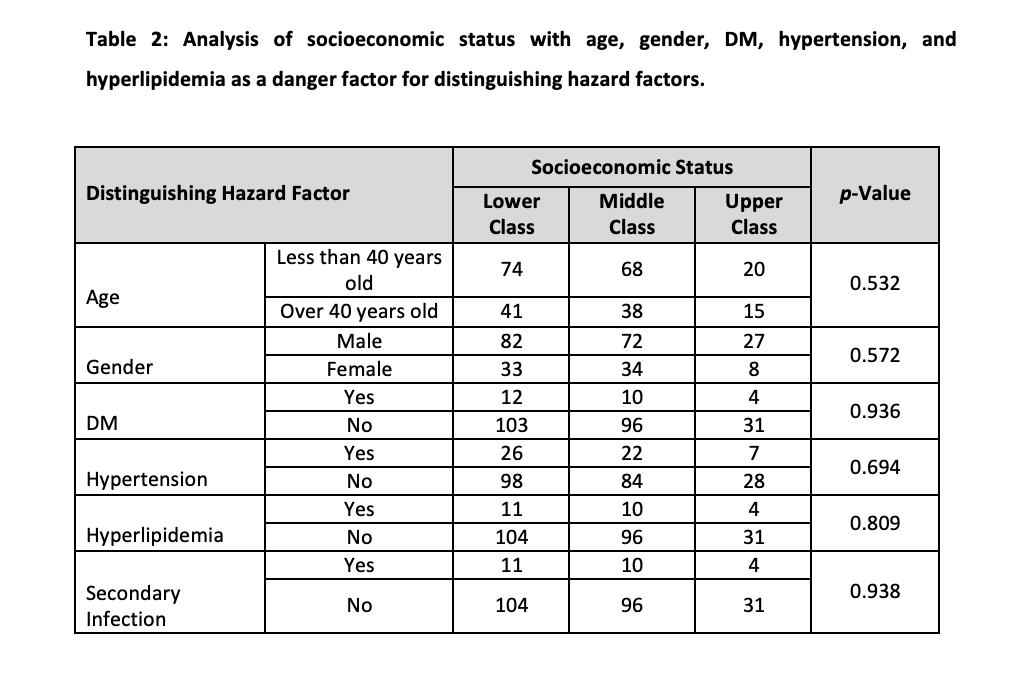
Analysis of socioeconomic status with age, gender, DM, hypertension, and hyperlipidemia as a danger factor for distinguishing hazard factors has been given in Table 2. Diabetes mellitus (DM), hypertension, hyperlipidemia and secondary infection were more common in participants who belonged to the lower socioeconomic status.
The effect of age on DHF studied by previous workers showed that babies and kids were in higher danger of creating DHF8,9. Our study too showed that most of the patients were young. Guzman et al had shown a bipolar example of expanded mortality, whereby youthful newborn children and the old matured 50 years and more established had higher case casualty and hospitalization rates10. Dung and Cam announced in 2003 that over 90% of dengue dreariness was in people who matured somewhere in the range of 15 and 25 years11. This could be identified with contrasts in way of life, time spent outside close to vectors, resting without mosquito nets, or different parts of lacking infection counteraction among the youthful. Another clarification could be that the illness can make long-lasting insusceptibility for the individual, so more seasoned people who have been uncovered all the more regularly may have more opposition, diminishing the bleakness rate. This study found same results as previous studies in Cuba10 and in Singapore12 where children, 14 years old had a higher danger of creating DHF contrasted with youthful grown-ups matured 15 years or more noteworthy. The reason behind this distinction could be because of brought down group invulnerability and change in transmission design10,12.
The distinguishing proof of dangerous components of DHF/DSS has its suggestions for clinical practice. It enables the doctors to organize care during a flare-up of dengue disease. Additionally, it offers a hint to the investigation of the pathogenesis of dengue disease. This investigation demonstrated a noteworthy factual relationship between sex and seropositivity to dengue. The seroprevalence of dengue fever was discovered to be equivalent among guys and females as indicated by Duncombe et al 13. However according to a study by Montenegro et al14. there was a prevalence of male sexual orientation among the 14 patients being considered who passed on of dengue fever. This could be credited to little sample size.
Comorbidities were demonstrated to be related to extreme clinical appearances of a few irresistible ailments, for example, SARS15,16, pandemic flu H1N117, tuberculosis 18,19 and hepatitis C 20. Numerous investigations discovered a relationship between different co-morbidities and DHF results 21 however just one examination was completed with a multivariate investigation to change for potential confounders22.
Distinguishing hazard factors for DHF can control clinicians to emergency dengue patients for the correct site of care for nearer observing and early intercession with liquid revival. In a plague where medical services assets might be extended, hazard characteristics for DHF can be utilized to organize hospital admissions of dengue patients. In our research, we saw that secondary infection was the most common danger factor in DHF. In this study frequency of risk factors was observed, 26 (10.8%) patients had Diabetes Mellitus, 55 (21.5%) had hypertension, 25 (9.8%) had hyperlipidemia and 192 (75%) had secondary infection with insignificant results (p<0.05). All diseases were common in participants who belonged to the urban area.
The secondary disease has been all around perceived as the more forceful type of dengue contamination in the past22,23, especially with DEN 2 infection24. Our information relating the seriousness of sickness with the optional disease is in concurrence with past work Wichmann et al. 25 in their examination indicated that optional dengue contamination was altogether connected with the advancement of DHF in youngsters, yet not in grown-ups. Likewise, our information recognized a huge relationship between age and kinds of contamination concerning the development of DHF.
The presence of co-morbidities, for example, diabetes has been proposed as a danger variable of the infection26. Our study showed about 10% of the patients had DM. A case-control study directed in Singapore discovered patients having hypertension and diabetes are in more danger of DHF27.
The results of this study are quite comparable to similar studies conducted in other countries. Similar to the results found in this study, A study in Taiwan concluded that poor socioeconomic status is an independent risk factor for developing dengue hemorrhagic fever (DHF) 28. Another study in Taiwan found that the incidence of Dengue hemorrhagic fever is more in patients who are diabetic. This conclusion also coincides with the results of this study. Thus, it can be said with much confidence that risk factors associated with the development of dengue hemorrhagic fever are quite similar in different countries. Attention must be given to avoiding these risk factors so that dengue hemorrhagic fever can be prevented to happen especially in high-risk areas and regions.
Strategy creators can organize populace bunches at high danger of creating DHF, for example, youthful males, patients in age bunch under 20 years, furthermore, patients having diabetes with hypertension for immunization when dengue antibodies are accessible, especially in asset-restricted nations. Segment and comorbidity hazard components may help general well-being clinicians bring issues to light among high-hazard people to take steps and measures against dengue contaminations.
Secondary infection was the most common risk factor in patients with DHF. Patients younger than 40 were more common than older patients. Males were predominately affected than females.
The authors would like to acknowledge the cooperation of their fellow doctors and nurses working in the medical ward along with them.
The authors declare no conflict of interest.
Ethical approval for conducting this study was obtained from the ethics review board of our hospital.
Informed consent was taken from all patients before obtaining the data.
HN and ME were involved in the study conception, write-up, critical review and approval of the final version. SA, MA, MKH and AN contributed to the research write-up and critical review. FF, TS and MER critically review the write-up and approved the final version of the manuscript to be published.
- Murray NEA, Quam MB, Wilder-Smith A. Epidemiology of dengue: past, present and future prospects. Clin Epidemiol. 2013;5:299-309. doi: 10.2147/CLEP.S34440
- Teixeira RR, Pereira WL, Oliveira AFC da S, da Silva AM, de Oliveira AS, da Silva ML, et al. Natural products as source of potential dengue antivirals. Mol Basel Switz. 2014;19(6):8151-8176. doi: 10.3390/molecules19068151
- Mawson AR. Retinoids, race and the pathogenesis of dengue hemorrhagic fever. Med Hypotheses. 2013;81(6):1069-1074. doi: 10.1016/j.mehy.2013.08.004
- Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue hemorrhagic fever: a retrospective study. BMC Infect Dis. 2015;15:1-12. doi: 0.1186/s12879-015-1141-3
- Tee HP, How SH, Jamalludin AR, Safhan MNF, Sapian MM, Kuan YC, et al. Risk factors associated with development of dengue haemorrhagic fever or dengue shock syndrome in adults in Hospital Tengku Ampuan Afzan Kuantan. Med J Malaysia. 2009;64(4):316-320.
- Pang J, Salim A, Lee VJ, Hibberd ML, Chia KS, Leo YS, et al. Diabetes with hypertension as risk factors for adult dengue hemorrhagic fever in a predominantly dengue serotype 2 epidemic: a case control study. PLoS Negl Trop Dis. 2012;6(5):1-8. doi: 10.1371/journal.pntd.0001641
- Wichmann O, Hongsiriwon S, Bowonwatanuwong C, Chotivanich K, Sukthana Y, Pukrittayakamee S. Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Trop Med Int Health TM IH. 2004;9(9):1022-1029. doi: 10.1111/j.1365-3156.2004.01295.x
- Hammond SN, Balmaseda A, Perez L, Tellez Y, Saborío SI, Mercado JC, et al. Differences in dengue severity in infants, children and adults in a 3-year hospital-based study in Nicaragua. Am J Trop Med Hyg. 2005; 73: 1063-1070.
- Shah I, Deshpande GC, Tardeja PN. Outbreak of dengue in Mumbai and predictive markers for dengue shock syndrome. J Trop Pediatr. 2004; 50:301-305. doi: 10.1093/tropej/50.5.301
- Guzmán MG, Kouri G, Bravo J, Valdes L, Susana V, Halstead SB. Effect of age on outcome of secondary dengue 2 infections. Int J Infect Dis. 2002; 6: 118-124. doi: 10.1016/S1201-9712(02)90072-X
- Dung NT, Cam NN. Dengue fever/dengue hemorrhagic fever in Hanoi – 2003. J Vietnam Prev Med. 2005; 1: 73-77.
- Ooi EE, Goh KT, Wang DN. Effect of increasing age on the trend of dengue and dengue hemorrhagic fever in Singapore. Int J Infect Dis. 2003 7: 231-232.
- Duncombe J, Lau C, Weinstein P, Aaskov J, Rourke M, Grant R, et al. Seroprevalence of dengue in American Samoa, 2010 [letter]. Emerg Infect Dis. 2013;19:324-326. doi: 10.3201/eid1902.120464
- Montenegro D, Lacerda HR, Lira TM, Oliveira DS, Lima AA, Guimarães MJ, et al. Clinical and epidemiological aspects of the dengue epidemic in Recife, PE, 2002. Rev Soc Bras Med Trop. 2006,39(1):9-13. doi: 10.1590/S0037-86822006000100002
- Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289(21): 2801-2809. doi: 10.1001/jama.289.21.JOC30885
- Lau EH, Hsiung CA, Cowling BJ, Chen CH, Ho LM, Tsang T, et al. A comparative epidemiologic analysis of SARS in Hong Kong, Beijing and Taiwan. BMC Infect Dis. 2010;10(1):1-9. doi: 10.1186/1471-2334-10-50
- Jain S, Kamimoto L, Bramley AM, Schmitz AM, Benoit SR, et al. Hospitalized patients with 2009 H1N1 influenza in the United States. N Engl J Med. 2009; 361(20): 1935-1944. doi: 10.1056/NEJMoa0906695
- Dooley KE, Chaisson RE. Tuberculosis and diabetes mellitus: Convergence of two epidemics. Lancet Infect Dis. 2009; 9(12): 737-744. doi: 10.1016/S1473-3099(09)70282-8
- Dooley KE, Tang T, Golub JE, Dorman SE, Cronin W. Impact of diabetes mellitus on treatment outcomes of patients with active tuberculosis. Am J Trop Med Hyg. 2009; 80(4): 634-640.
- Charlton MR, Pockros PJ, Harrison SA. Impact of obesity on treatment of chronic hepatitis C. Hepatology. 2006;43(6):1177-1186. doi: 10.1002/hep.21239
- Lee MS, Hwang KP, Chen TC, Lu PL, Chen TP. Clinical characteristics of dengue and dengue hemorrhagic fever in a medical center of southern Taiwan during the 2002 epidemic. J Microbiol Immunol Infect. 2006;39(2):121-129.
- Burke DS, Nisalak A, Johnson DE, Scott RM. A prospective study of dengue infections in Bangkok. Am J Trop Med Hyg. 1988;38(1):172-180. doi: 10.4269/ajtmh.1988.38.172
- Messer WB, Vitarana UT, Sivananthan K, Elvtigala J, Preethimala LD, Ramesh R, et al. Epidemiology of dengue in Sri Lanka before and after the emergence of epidemic dengue hemorrhagic fever. Am J Trop Med Hyg. 2002;66(6):765-773.
- Chow VT. The challenge of dengue–desperately seeking solutions. Singapore Med J. 1998;39(6):234-235.
- Wichmann O, Hongsiriwon S, Bowonwatanuwong C, Chotivanich K, Sukthana Y, Pukrittayakamee S. Risk factors and clinical features associated with severe dengue infection in adults and children during the 2001 epidemic in Chonburi, Thailand. Trop Med Int Health. 2004 ;9(9):1022-1029. doi: 10.1111/j.1365-3156.2004.01295.x
- Figueiredo MA, Rodrigues LC, Barreto ML, Lima JW, Costa MC, Morato V, et al. Allergies and diabetes as risk factors for dengue hemorrhagic fever: results of a case control study. PLoS Negl Trop Dis. 2010;4(6):1-6. doi: 10.1371/journal.pntd.0000699
- Pang J, Salim A, Lee VJ, Hibberd ML, Chia KS, Leo YS, et al. Diabetes with hypertension as risk factors for adult dengue hemorrhagic fever in a predominantly dengue serotype 2 epidemic: a case control study. PLoS Negl Trop Dis. 2012;6(5):1-8. doi: 10.1371/journal.pntd.0001641
- Lai YJ, Lai HH, Chen YY, Ko MC, Chen CC, Chuang PH, et al. Low socio-economic status associated with increased risk of dengue haemorrhagic fever in Taiwanese patients with dengue fever: a population-based cohort study. Trans R Soc Trop Med Hyg. 2020;114(2):115-120. doi: 10.1093/trstmh/trz103
This is an open-access article distributed under the terms of the CreativeCommons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
