By Saira Jahan1, Shumaila Parveen2, Sumbal Barnabas2, Ahyab Mehreen2
AFFLIATIONS:
- Riphah College of Rehabilitation and Allied Health Sciences, Riphah International University, Islamabad, Pakistan.
- Department of Physical Therapy, Railway General Hospital Rawalpindi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-4/013
ORCID iD: 0000-0002-0872-3372
How to cite: Jahan S, Parveen S, Barnabas S, Mehreen A. Restless Leg Syndrome and Sleep Quality in Diabetic Patients with and Without Neuropathy. Pak J Med Dent. 2022;11(4): 82-87. doi: 10.36283/PJMD11-4/013
Background: Restless legs syndrome (RLS), is a condition of uneasy feeling with an uncontrollable urge to move legs. This study was conducted to compare the frequencies of restless leg syndrome and sleep quality in diabetic patients with and without neuropathy.
Methods: The comparative cross-sectional was conducted from February to June 2021 at Riphah College of Rehabilitation and Allied health sciences in collaboration with Pakistan Railway Hospital, Rawalpindi. A total of 271 participants were taken after informed consent. Pittsburgh Sleep Quality Index and Restless Leg Syndrome-Disability Index scale were used for assessing the quality of sleep and RLS in all participants, respectively. The relationship between the quality of sleep in diabetic patients with and without neuropathy was assessed by one-way ANOVA.
Results: Out of 271 diagnosed cases of diabetes mellitus, 65 (23.9%) were males and 206 (76%) were females. A significant relation (p<0.05) between restless leg syndrome in diabetic patients with neuropathy (2.65±1.36) was observed compared to diabetic patients without neuropathy (1.20±1.44) with p< 0.01. A significant relationship was also found between the quality of sleep in diabetic patients with neuropathy (1.87±0.33).
Conclusion: Restless leg syndrome is common in diabetic patients (p<0.05) with neuropathy compared to diabetic patients without neuropathy and sleep quality equally deteriorated in diabetic patients regardless of neuropathy.
Keywords: Diabetes Mellitus; Neuropathy; Restless Leg Syndrome; Sleep Quality.
Restless leg syndrome (RLS) is a sensorimotor sleep-related movement disorder characterized by a strong desire to move one’s legs and an uncomfortable sensation in the lower extremities1. The prevalence of RLS in the general population is 5 to 15% 2,3. The unpleasant sensation in the legs improved with movement. Restlessness in the legs gets worse during sleep or at rest making sleep initiation or maintenance more difficult. Thus, sleep disturbances occur in persons who suffer from this illness, resulting in daytime exhaustion, poor energy, irritability, and depression4. RLS can have a substantial negative impact on one’s quality of life and everyday activities, as well as significant financial, social, and healthcare expenses5,6. RLS has been significantly associated with obesity, hypertension, diabetes and metabolic syndrome7, 8.
According to the most recent data from the World Health Organization (WHO) 422 million individuals worldwide have been diagnosed with diabetes mellitus9. Diabetes mellitus currently affects 240 million people worldwide, with the figure expected to rise to 380 million by 2025, with low- and middle-income nations bearing the brunt of the burden10. Pakistan is now ranked 6th among countries with the highest prevalence of diabetes mellitus11. Pakistan is in a high-prevalence area, with 6.9 million people currently affected and anticipated projections of 11.5 million people affected by 2025 12.
In type 2 DM diabetes-related Peripheral neuropathy is very frequent and called diabetic polyneuropathy. Routine Symptoms described by patients are tingling, uncomfortable sensation and ache in the lower extremities while walking. Diabetes-related eye ailment retinopathy, irregular and abnormal lipid quantity in the body, cardiovascular disorders, unemployed status and diabetes mellitus for more than 5 years are significantly associated with diabetic poly neuropathy13. When a high level of glucose in the blood and for a longer duration of time occurs, nerve ending of upper and lower extremities particularly the distal-most segments like hands and feet often experience neuropathic complications14,15.
Diabetes mellitus is a group of metabolic disorders in which blood glucose level increases because of abnormality in the secretion of insulin, its action, or both15. In type 2 diabetes mellitus, impaired glucose metabolism results in polyuria, polydipsia and physical impairment causing sleep disturbances. The association between RLS and diabetes has been reported previously16. This study was conducted to compare the frequencies of restless leg syndrome in diabetic patients with or without neuropathy and to compare the quality of sleep of diabetes patients with and without neuropathy.
The comparative cross-section survey was conducted from February 2021 to June 2021 at Railway General Hospital Rawalpindi, Pakistan. After approval from the Riphah College of Rehabilitation and Allied Health Sciences’ ethics review committee (Ref # Riphah/RCRS/REC/00907) and the heads of the participating institution, the sample size was calculated as 271 keeping the 90% confidence interval, 5% margin of error and response distribution as 50% with 20000 population size by using Raosoft. Patients with diagnosed diabetes were subsequently recruited with no history of malignancy and any other hereditary or systemic illness. After getting informed consent from the participants, the restless leg syndrome-Disability Index scale was used for assessing restless leg syndrome and the Pittsburg Sleep Quality Index scale for quality of sleep in all the participants. Questionnaires were explained to respondents. The subjective sleep quality, sleep latency, sleep length, habitual sleep efficiency, sleep disruptions, usage of sleeping medications, and daytime dysfunction are the seven “component” scores that are generated from the 19 individual items.
Every questionnaire has been filled by researchers themselves from every diabetic patient. One overall score is produced by adding the scores for these seven components. The mean and standard deviation were calculated using descriptive analysis. Categorical variables were expressed as proportions and percentages while continuous variables were expressed in terms of Mean±SD. A Chi-square test was used to find the association of restless leg syndrome with quality of sleep and an independent t-test was used to a comparison of the restless leg syndrome and sleep quality in diabetic patients with and without neuropathy. To compare the relationship between quality of sleep in diabetic patients with and without neuropathy one-way ANOVA was applied. For statistical analysis of the data, SPSS 21 was used was p-value less than 0.05 was considered significant.
A total of 271 participants with diagnosed cases of diabetes mellitus were enrolled in this study. Among them, 83 cases (30.6%) were without diabetic neuropathy and [188(69.4%)] were with diabetic neuropathy. The percentage of female participants in this study is [76% (206)] and that of the male is [24% (65)] (Figure 1). Data was tested for normality using the Shapiro-Wilk test. A parametric test has been used to compare the RLS in diabetic patients with neuropathy and without neuropathy. There is a significant relation between restless leg syndrome in diabetic patients with neuropathy (Mean±SD=2.65±1.36) compared to diabetic patients without neuropathy (1.20±1.44) with p< 0.01 as shown in Table 1.
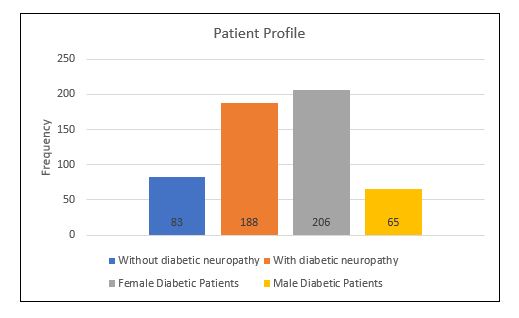
Figure 1: Patient profile concerning the frequency of male and female diabetic patients and individuals with diabetic neuropathy versus without diabetic neuropathy.
Table 1: Frequency of restless leg syndrome (RLS) in diabetic patients with and without neuropathy.
| Restless Leg Syndrome | With Neuropathy
(n=188) (%) |
Without Neuropathy
(n= 83) (%) |
p-Value |
| None | 30(11.07%) | 43(15.86%) | 0.05 |
| Mild RLS | 07(2.58%) | 08(2.95%) | |
| Moderate RLS | 17(6.27%) | 12(4.42%) | |
| Severe RLS | 78(28.78%) | 12(4.423%) | |
| Very Severe RLS | 56(20.66%) | 08(2.95%) |
There was a significant relationship found between quality of sleep in diabetic patients with neuropathy (1.87±0.33) compared to the diabetic patient without neuropathy (1.69±0.46) with a statistically significant result (p<0.001) shown in Table 2.
Table 2: Sleep quality in diabetic patients with and without neuropathy.
| Variables | Good sleep quality
(n=48) (%) |
Poor sleep quality
(n=223) (%) |
Mean ±SD | p-Value |
| With neuropathy | 23 (47.9%) | 165 (73.9%) | 1.87 ± 0.32 | <0.01 |
| Without neuropathy | 25 (52.0%) | 58 (26.0%) | 1.69 ±0.46 |
No sleep quality was disturbed in 48 (17.71%) participants, in them, 25 participants reported no restless leg syndrome while the remaining 23 reported mild, moderate, severe and very severe RLS. Furthermore, a total of 223 (82.28%) participants reported sleep disturbance, 48 (17.7%) reported no RLS and 175 (64.5%) participants had RLS ranging from mild, moderate, severe and very severe RLS having p<0.01.
The results suggested that there was a strong relationship between RLS in the diabetic population with neuropathy. Diabetics may experience RLS and neuropathy as a result of common risk factors such as glucose intolerance, dyslipidemia, and obesity11. In a case-control study, RLS was found to be comorbidity in diabetics, with a prevalence of 22.4% 17. Multiple experimental and epidemiological studies have found that poor sleep quality is associated with a higher prevalence of fasting plasma glucose and HbA1c18-20. Diabetes has a significant impact on sleep and mood disturbances, along with autonomic regulation. As a result, these factors encourage the onset and development of RLS. Sleep and mood disturbances also harm pain processing and perception, contributing to the development of RLS symptoms. In diabetes patients, restless legs syndrome leads to poor sleep quality and reduces the overall quality of life. In patients with type 2 diabetes, poor sleep itself is a risk factor for uncontrolled glucose levels21.
RLS adds to a patient’s already significant healthcare, social, and financial burdens. The association between RLS and diabetes, on the other hand, has yet to be established in the Pakistani population. Research on pathways that contribute to the development of RLS and the implications of RLS could help the scientific community with the pathophysiology of RLS22. This may make it easier to develop preventive measures or improved management strategies for this complex disease23. Those without neuropathy showed a high percentage of No RLS in them. RLS causes creepy-crawly sensations in the legs and gets resolved by activity3. RLS causes an ant sensation in the legs, an irresistible urge to move the legs restlessness and fatigue. It gets worse when the person is resting. To treat RLS it is important to consider that we must treat the risk factors associated with RLS which are sleep disturbance and poor glycemic control. The study had 271 diagnosed cases of diabetes mellitus, and 188 of them were with neuropathy and 83 participants were without neuropathy.
Our study shows that the presence of RLS was more in diabetic neuropathic patients and there was also poor sleep quality in diabetic patients regardless of neuropathy. Modarresnia et al. conducted a study “restless leg syndrome in Iranian people with type 2 diabetes Mellitus” and concluded that Patients with restless leg syndrome (RLS) were almost three times as likely as patients without restless leg syndrome to have poor sleep quality5. Our study also showed a significant association between restless leg syndrome and quality of sleep, results stated that overall poor sleep quality in diabetic patients with the presence of restless leg syndrome. Results were like the studies of Pinheiro et al. and Azharuddin et al. have documented that the restless leg syndrome resulted in poor sleep quality24,25.
The current study’s result showed that restless leg syndrome was more prevalent among diabetic patients with neuropathy than without neuropathy, and a study by Mirghani has supported our results26. Also, this study has further confirmed our results that there is no specific association between age and RLS. A study conducted concluded that restless leg syndrome (RLS) occurred more in diabetics, their article fully supported the current study as out of a total of 271 diabetic patients 198 (73.0%) participants were either described as mild, moderate, severe, or very severe restless leg syndrome27. In an article, a case-control study was conducted on the prevalence of RLS in diabetes type 2 Mellitus. This article suggests that diabetes is a risk factor for RLS. Patients with diabetic neuropathy are more to develop RLS. Diabetic neuropathy occurs in about one-third of the population. It is seen that diabetes gets complicated with the development of neuropathy24.
A study by Afkhami-Ardekani et al. reported that Diabetes Mellitus (DM) was one of the most common metabolic disorders and restless leg syndrome (RLS) occurred more in diabetics27. Our study showed a significant association between restless leg syndrome and quality of sleep, results stated that overall poor sleep quality in diabetic patients with the presence of restless leg syndrome.
The current study’s result showed that restless leg syndrome was more prevalent among diabetic patients with neuropathy than those without neuropathy. There is a significant association between sleep quality with RLS. People with diabetes who suffer from RLS develop poor sleep quality and sleep duration. Poor sleep and glycemic control have a direct relation with RLS. While the current study revealed that the presence of RLS is poor sleep quality in the diabetic patient with and without neuropathy. Our results reported that there was no difference in sleep quality between diabetic patients with or without neuropathy. Overall, the quality of sleep was equally disturbed in diabetic patients regardless of neuropathy and non-neuropathy. Our finding was not like the study of Radhakrishnan et al. that documented the significant impairments in sleep quality in the diabetic patient with neuropathy than without neuropathy28.
Restless leg syndrome is more common in diabetic patients with neuropathy as compared to diabetic patients without neuropathy. There is also no significant difference in the quality of sleep between diabetic patients with and without neuropathy, Sleep quality equally deteriorated in diabetic patients regardless of neuropathy.
The authors would like to thank the Pakistan Railway Hospital, Rawalpindi for the help in data collection.
The author(s) declared no conflicts of interest.
This study was approved by the ethics review committee of the Riphah College of Rehabilitation and Allied Health Sciences, Riphah International University, Islamabad (With Ref # Riphah/RCRS/REC/00907).
Verbal informed consent was obtained from all the patients regarding their participation in the study and publication of data while maintaining confidentiality and anonymity.
All authors contributed equally to the study.
- Kumar KH. Metabolic Complications Sleep disorders in Pregnancy: Glycaemic implications. J Pak Med Assoc. 2016;66(9):60-64
- Kwatra V, Khan MA, Quadri SA, Cook TS. Differential diagnosis and treatment of restless legs syndrome: a literature review. Cureus. 2018;10(9):1-7. doi: 10.7759/cureus.3297
- Hu S, He X, Zhang Y, Hu S, He F, Zhao F, et al. Effectiveness and safety of massage in the treatment of restless legs syndrome: A protocol for systematic review and meta analysis. Medicine (Baltimore). 2020;99(48):1-4. doi: 10.1097/MD.0000000000023239
- Salas RE, Gamaldo CE, Allen RP. Update in restless legs syndrome. Curr Opin Neurol. 2010; 23(4): 401-406. doi: 10.1097/WCO.0b013e32833bcdd8
- Modarresnia L, Golgiri F, Madani NH, Emami Z, Tanha K. Restless legs syndrome in Iranian people with type 2 diabetes mellitus: the role in quality of life and quality of sleep. J Clin Sleep Med. 2018;14(2):223-238. doi: 10.5664/jcsm.6938
- Cuellar NG, Dorn JM. Peripheral diabetic neuropathy or restless legs syndrome in persons with type 2 diabetes mellitus: differentiating diagnosis in practice. J Am Assoc Nurse Pract. 2015;27(12):671-675. doi: 10.1002/2327-6924.12311
- Trenkwalder C, Allen R, Högl B, Clemens S, Patton S, Schormair B, et al. Comorbidities, treatment, and pathophysiology in restless legs syndrome. Lancet Neurol. 2018;17(11):994-1005. doi: 10.1016/S1474-4422(18)30311-9
- Kalra S, Gupta A. Diabetic painful neuropathy and restless legs syndrome in diabetes. Diabetes Ther. 2018;9(2):441-447. doi: 10.1007/s13300-018-0376-6
- World Health Organization. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation [Internet]. Part 1, Diagnosis and classification of diabetes mellitus. World health organization; 1999 [cited 2022 Jun 16]. Available from: https://apps.who.int/iris/bitstream/handle/10665/66040/?sequence=1
- Qidwai W, Ashfaq T. Imminent epidemic of diabetes mellitus in Pakistan: issues and challenges for health care providers. J Liaquat Univ Med Health Sci. 2010; 9(3):112-113.
- Kiyani MM, Jahan S, Kiyani SK, Rehman H, Khan LG, Iqbal U. Erythrocyte sedimentation rate in diabetic and non-diabetic patients of cardiovascular disease. J Technol Lab. 2019;8(1):18-22. doi: 10.29238/teknolabjournal.v8i1.159
- Anwar SB, Asif N, Naqvi SA, Malik S. Evaluation of multiple risk factors involved in the development of diabetic retinopathy. Pak J Med Sci. 2019; 35(1): 156-160. doi: 10.12669/pjms.35.1.279
- Khawaja N, Abu-Shennar J, Saleh M, Dahbour SS, Khader YS, Ajlouni KM. The prevalence and risk factors of peripheral neuropathy among patients with type 2 diabetes mellitus; the case of Jordan. Diabetol Metab Syndr. 2018;10(1):1-10. doi: 10.1186/s13098-018-0309-6
- Brown JJ, Pribesh SL, Baskette KG, Vinik AI, Colberg SR. A comparison of screening tools for the early detection of peripheral neuropathy in adults with and without type 2 diabetes. J Diabetes Res. 2017;2017:1-12. doi: 10.1155/2017/1467213
- Mustafa M, Jahan S, Waseem M, Ramzan T, Latif D. Comparing fasting homocysteine levels among healthy adults, diabetic and non-diabetic cardiac patients. J Riphah Coll Rehab Sci. 2018; 6(2): 63-66. doi: 10.5455/JRCRS.2018060202
- Rajender A, Gaurav R, Kanwal K, Chaudhri RS, Deepa C, Choudhary P. Restless leg syndrome as co-morbidity in type 2 diabetes mellitus. Int J Adv Med. 2016;3:282-386. doi: 10.18203/2349-3933.ijam20161076
- Rajender A, Mathur S, Choudhary P, Upadhyay S, Rajender G, Bhargava R, et al. Restless leg syndrome a common undiagnosed comorbidity of clinical significance in cirrhosis. Gastroenterol Hepatol Bed Bench. 2019; 12(1):13-16.
- Bener A, Al-Hamaq AO, Ağan AF, Öztürk M, Ömer A. The prevalence of restless legs syndrome and comorbid condition among patient with type 2 diabetic mellitus visiting primary healthcare. J Family Med Prim Care. 2019; 8(12):3814-3820. doi: 10.4103/jfmpc.jfmpc_463_19
- Sabic A, Sinanovic O, Sabic D, Galic G. Restless legs syndrome in patients with hypertension and diabetes mellitus. Med Arch. 2016; 70(2):116-118. doi: 10.5455/medarh.2016.70.116-118
- Tsai YW, Kann NH, Tung TH, Chao YJ, Lin CJ, Chang KC, et al. Impact of subjective sleep quality on glycemic control in type 2 diabetes mellitus. Fam Pract. 2012;29(1):30-35. doi: 10.1093/fampra/cmr041
- Manik KA, PP SJ, Jagadal I. Blood pressure variation in night shift male security guards in north Kerala. National Journal of Physiology, Pharmacy and Pharmacology. 2021;11(1):47-50. doi: 10.5455/njppp.2021.10.07185202001092020
- Solanki JD, Makwana AH, Mehta HB, Gokhale PA, Shah CJ. Body composition in type 2 diabetes: Change in quality and not just quantity that matters. Int J Prev Med. 2015; 6: 1-5. doi: 10.4103/2008-7802.172376
- Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4
- Pinheiro T, Thomas T, Devaraj U, Ramachandran P, Krishnaswamy UM. Prevalence of restless legs syndrome and quality of sleep in type 2 diabetics. J Diabetes Complications. 2020;34(12):1-5. doi: 10.1016/j.jdiacomp.2020.107727
- Azharuddin M, Kapur P, Adil M, Ghosh P, Sharma M. The impact of sleep duration and sleep quality on glycaemic control in Asian population with type 2 diabetes mellitus: A systematic literature review and meta-analysis of observational studies. Clin Epidemiol Glob Health. 2020;8(3):967-975. doi: 10.1016/j.cegh.2020.03.006
- Mirghani H. Restless legs syndrome among Sudanese patients with type 2 diabetes mellitus: a case-control study. Cureus. 2020;12(8):1-6. doi: 10.7759/cureus.9635
- Afkhami-Ardekani A, Momayez-Sanat Z, Vahhabi Z, Vazirpanah T, Afkhami-Ardekani M. The Relationship between Frequency of Restless leg Syndrome and Type 2 diabetes. Iranian J Diabetes Obes. 2017;9(1):40-44.
- Radhakrishnan C, CR RR, Sreejith K, Anjusha UT. Comparison of cognitive function, depression, and sleep quality among type 2 diabetes mellitus patients with and without diabetic neuropathy. Diabetes. 2018;67: doi: 10.2337/db18-574-P
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
