By Shama Chaudhry, Hina Rajani, Rahima Rais, Habiba Sharaf Ali
AFFLIATIONS:
Department of Obstetrics and Gynecology, Ziauddin University Hospital, Karachi, Pakistan.
DOI: https://doi.org/10.36283/PJMD11-4/010
How to cite: Chaudhry S, Rajani H, Rais R, Ali HS. Efficacy and Safety of Misoprostol Administered Rectally Compared with Oxytocin for the Prevention of Postpartum Hemorrhage. Pak J Med Dent. 2022;11(4): 61-66. doi: 10.36283/PJMD11-4/010
Background: The foremost cause of maternal morbidity and mortality in third-world countries is Post-Partum Hemorrhage (PPH). To prevent PPH, often Misoprostol is used. This study aimed to find out the efficacy and safety profile of Misoprostol when administered rectally in comparison to oxytocin, to avoid the incidence of PPH.
Methods: This quasi-experimental study on n=72 patients were performed at Ziauddin University and Hospital Karachi for 6 months (2021). The patients were divided into two groups. Oxytocin (10 IU) was administered intramuscularly to Group A(n=36) while 400ug of Misoprostol was given to group B(n=36) rectally, at the time of delivery. The level of hemoglobin was checked at the time of admission and 24 hours after delivery and side effects were also monitored. Chi-square and t-test were applied between both groups and a p-value <0.05 was taken as significant.
Results: The average duration of the third stage of labor in the Misoprostol group was 5.3 minutes versus the Oxytocin (Syntocinon) group 3.75 minutes (p= 0.012). The decrease in the level of hemoglobin and the blood loss quantity was not significantly different in both groups (p=0.766, 0.203) respectively. The side effect of shivering was seen in group B in 4(11.1%) of the patients (p=0.04) and hyperthermia was observed in 2 (5.6%) (p=0.151).
Conclusion: Misoprostol proved to be efficacious oxytocin in PPH prevention. Therefore, Misoprostol can likely be of help during the third stage of labor, especially in countries with developing healthcare setups.
Keywords: Misoprostol; Postpartum Hemorrhage; Oxytocin; Maternal Mortality; Uterotonic.
Primary Post-partum Hemorrhage (PPH) is defined as the loss of over half a liter of blood within the first 24 hours after delivery in normal vaginal delivery or that of one liter of blood within the first 24 hours after a caesarian section1. In Pakistan, PPH is the root of maternal death. Of all the deliveries that occur, about thirteen percent may result in PPH with loss of blood more than 1000ml. Hemorrhage, which is threatening to life, however, takes place in 1 in 1000 deliveries. Its incidence is 11% globally among women in labor2. Emergency postpartum hysterectomy is often done for PPH that cannot be controlled by conventional methods3. It leads to an increase in maternal deaths, which are at least 200 times more prevalent in developing countries than in developed countries4. An atonic uterus is estimated to be observed in 70% of the cases leading to PPH5. Appropriate care of the third stage of labor is an excellent way to prevent PPH. Such measures include late clamping of the cord, sustained traction of the cord and using Oxytocin therapy6. PPH incidence has been reduced by using oxytocin (Syntocinon).
The active management of the third stage of labor lowers the rates of PPH as compared to the expectant management3. The World Health Organization (WHO) recommends delivering prophylactic oxytocin intramuscularly in the third stage of labor. A Cochrane systematic review shows that the use of oxytocin halves the risk of PPH4. There are, however, many issues with oxytocin use in developing countries, such as protecting it from light, the need to refrigerate and sterilization of syringes and needles for administration. Misoprostol, a protein uterotonic agent, has also been used in various settings for the prevention of PPH7. Misoprostol, a prostaglandin E1 analog, is resistant to heat and can be administered sublingually, orally, rectally, or vaginally. The rectal route is considered the best one to avoid gastrointestinal side effects such as diarrhea, vomiting and nausea5,8. Misoprostol is a methyl-ester of prostaglandin E1 and methylated at C-169. It consists of a minor amount of hydrogen castor oil7. The WHO and International Federation of Gynaecology and Obstetrics recommend a single dose of 600 µg misoprostol, oral or sublingual, for the prophylaxis of PPH5. Moreover, a dose of Misoprostol of up to 800ug does not cause high blood pressure. Therefore, this study aimed to find out the efficacy and safety profile of Misoprostol when administered rectally in comparison to oxytocin, to avoid the incidence of PPH.
A quasi-experimental study was conducted in the Department of Obstetrics and Gynecology of Ziauddin Hospital for six months (2021). The non-probability convenience sampling technique was used to collect the data. The sample size of n=36 per group was calculated by the WHO calculator keeping a 95% confidence interval with a prevalence of 20%. This study has been approved by the ethics review committee of the hospital. The proper informed consent from the participants who were admitted to the labor room was taken.
The study includes patients with all the delivery modes. However, those who had a lower segment cesarean section were anemic (hemoglobin less than 9gm/L), multiparous (more than 5 deliveries), with abnormalities of platelets including low platelet counts, or those with multiple gestations were excluded from the study. A concise history with relevant obstetric and past medical history was taken from each patient before delivery.
A relevant clinical examination was also performed. Patients who met the criteria were randomly incorporated into 2 groups. When it was time to deliver the anterior shoulder, Group A was given 10 IU of Oxytocin intramuscularly whereas the B group was given 400ug of misoprostol per rectally. A blood sample was drawn to find out the hemoglobin levels in those patients who had given consent before delivery. For blood absorption, a clean absorbent drape was kept under the buttock region of each woman. The women wore a pad additionally for over one hour. A measuring scale was used to measure the weight of each drape and pad with subtraction of the weight of the linen respectively. By approximation, as 1 ml of blood equals 1 gm, the additional grams were calculated as the loss of blood in ml. After measuring the hemoglobin levels, the effects were noted till 1 day after the delivery. A Performa was then made with the relevant data. The results included quantifying the patients who suffered from PPH, decreases in hemoglobin levels and the adverse effects that occurred.
Statistical Package for Social Science (SPSS) version – 20 was used to analyze the data. The use of percentages and frequencies was employed to present the various categorical variables such as a history of previous PPH, pregnancy-related side effects, primary post-partum side effects and past medical history. To compare the categorical variables between both groups, the Chi-square test was employed. The continuous variables such as age, length of the third stage of labor and hemoglobin were calculated as Mean + SD and compared by using an independent sample t-test between both groups. A p-value of less than 0.05 was taken as a significant value.
Among 72 participants in the study, the patients were divided into two equal groups. Both groups had 36 women. The mean age of women in the Misoprostol group was (27.08±4.83) years and in the oxytocin group (27.94±4.80) years. A statistical significance was seen in the duration of the third stage of labor between both groups with a p-value of 0.012. Table 1 showed the comparison of different parameters between each group.
Table 1: Comparison between Misoprostol and Oxytocin (Syntocinon).
| Parameters | Misoprostol
(n=36) |
Syntocinon
(n=36) |
p-Value |
| Age (years) | 27.08±4.83 | 27.94±4.80 | 0.451* |
| Gravida
1 – 3 4 – 7 |
26 (72.2%) 10 (27.8%) |
27 (75%) 9 (25%) |
0.789¥ |
| Duration of 3rd stage labor | 5.30±2.05 | 3.75±2.97 | 0.012* |
| Amount of blood lost | 128.47±89.37 | 165.27±146.64 | 0.203* |
| Pre-delivery Haemoglobin | 11.11±1.1 | 11.19±1.0 | 0.766* |
| Post-delivery Haemoglobin | 10.7±1.1 | 10.8±1.1 | 0.882* |
| History of PPH
Yes No |
1 (2.8%) 35 (97%) |
1 (2.8%) 35 (97%) |
1.00¥ |
| Complications during a previous pregnancy
Yes No |
1 (2.8%) 35 (97%) |
0 (0%) 36 (100%) |
0.314¥ |
| Complications during this pregnancy
Yes No |
9 (25%) 27 (95%) |
4 (11%) 32 (89%) |
0.126¥ |
*Independent sample t-test, ¥Chi-square test.
The Misoprostol group had side effects that included shivering which occurred in 4(11%) patients and hyperthermia in 2(5.6%) of the patients. In the Syntocinon group, side effects included nausea in 1(2.8%) of the patients and PPH in 3(8.4%) of the patients. Amongst these side effects, shivering was found to be statistically significant and was managed straightforwardly (Table 2). The absence of side effects with vs without the administration of Misoprostol and Oxytocin (Syntocinon) are also shown in Figure 1.
Table 2: Side effects of Misoprostol and Oxytocin (Syntocinon) drugs.
| Side Effects | Misoprostol (n=36) | Syntocinon (n=36) | p-Value | ||
| With | Without | With | Without | ||
| Nausea | 0 (0%) | 36 (100%) | 1 (2.8%) | 35 (97%) | 0.314 |
| Shivering | 4 (11%) | 32 (89%) | 0 (0%) | 36 (100%) | 0.04 |
| Hyperthermia | 2 (5.6%) | 34 (94.4%) | 0 (0%) | 36 (100%) | 0.151 |
| PPH | 0 (0%) | 36 (100%) | 3 (8.4%) | 33 (91.6%) | 0.077 |
Primary Post-partum Hemorrhage (PPH).
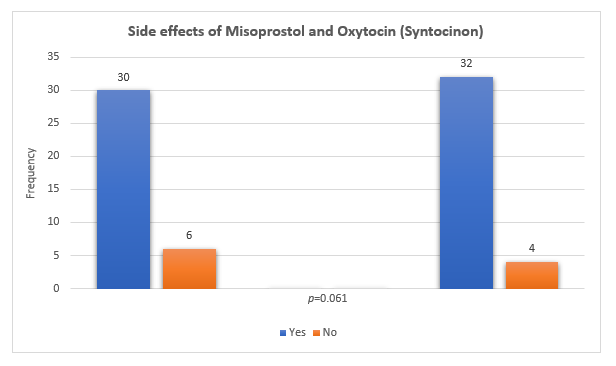
Figure 1: The absence of side effects with vs without the administration of Misoprostol and Oxytocin (Syntocinon).
Even to this date, more than 80% of deliveries, which occur in Pakistan, are at home10. The outcome of PPH aggravates because people are not able to gain access to trained personnel who can administer intravenous oxytocin. Moreover, delays in arriving at a hospital in due time can lead to damage, which is irreversible. There is an average interval of two hours starting from the onset of PPH leading to maternal demise. Significant reduction in PPH (up to 40%) after administrating an oxytocic drug in the third stage of labor is evident. This was observed in a sample of 22 women11.
A total of 70 patients in active labor, were made to divide into two groups with 35 patients each. Group 1 was given Oxytocin and group 2 was given Misoprostol. All outcome measures were analyzed. There was no major difference in Misoprostol administered orally and Oxytocin administered intramuscularly during the management of the final stage of labor. This study proves the advantage of misoprostol comparable to Oxytocin for PPH prevention. Misoprostol, therefore, can be used as a suitable alternative to the use of Oxytocin12. Furthermore, it was found that the per rectal route has fewer adverse effects, and can be prescribed by a general practitioner who is conducting the delivery and to those women experiencing nausea. The difference was observed to be not of any significance in the two groups in terms of PPH (which was calculated by the amount of blood lost).
A few reports on Misoprostol administration via the rectal route for the therapeutic purpose in the final stage of labor are also present. Chaudhuri et al. carried out a study in search of an alternative to Oxytocin to prevent the occurrence of PPH13. In that study, a comparison was carried out between orally administered misoprostol and I.V infusion oxytocin. In contrast, in our study, we administered Misoprostol rectally. The result was a significant decrease in blood loss in the Misoprostol group compared to the Oxytocin group. Secondary outcome parameters such as Hb levels and the requirement for blood transfusion were homogenous in both groups. Quibel et al. carried out a randomized control trial for the management of the final stage of labor, putting to test the efficacy of Oxytocin and misoprostol in the prevention of PPH14. The baseline characteristics were similar in both groups. Thus, 1,721 patients illustrated that misoprostol was not effective and exhibited more adverse effects. Adverse maternal events occurred with higher frequency in the misoprostol group (for fever 30.4% in the misoprostol group and 6.3% in the placebo group) 14.
Bajwa et al. conducted a randomized prospective study to determine the most effective route for misoprostol administration, that showed the highest acceptability and compliance in the participants, decreased duration of the third stage of labor, and decreased side effects15. There were 300 healthy participants, divided randomly into three groups of 100 participants each, and were given misoprostol 400ug through the oral (0), rectal(R), and sublingual(S) routes, during the third stage of labor. Blood loss was estimated in terms of a decrease in hemoglobin, hematocrit, and packed cell volume (PCV) levels and the duration of the third stage of labor was compared. All routes had the same effectiveness in the management of the third stage of labor but rectally administered misoprostol showed better acceptability, comparable efficacy, and had an incidence of minimal side effects, like our results16,17.
The success of rectal misoprostol in the treatment of the third stage of labor or the prevention of PPH has been explained by various others as well7,18-20. Especially in settings where intravenous uterotonic agents are unavailable, Misoprostol is an acceptable indication for the prevention of PPH21. Regarding the side effects of misoprostol in the current study, we have noticed that shivering occurs significantly in women who were treated with rectal misoprostol when compared to women who were treated with oxytocin. This was an inevitable effect although it was self-limiting and responded to chlorphenermine22-25. The incidence of shivering and hyperthermia with misoprostol was very low in our study. It was observed in four and two patients respectively, however, it did not occur with Oxytocin. A study depicted that shivering was found in 11.8% of the mothers and hyperthermia was found in 4% of the mothers treated with misoprostol as compared with oxytocin (3.39% of the patients suffered from shivering and 1.4% from hyperthermia)14. These side effects were low in our study because we used 400ug of misoprostol per rectally as compared to the study by Sweed et al., in which 200ug of misoprostol was used20. Thereby concluding that the incidence of side effects was considerably low in our study and might be related to the limitation in route of administration as well as the dose administered.
Rectally administered Misoprostol is more effective the oxytocic drugs to prevent the occurrence of PPH. The adverse effects are fewer and there is a higher safety profile. Misoprostol is viable for effective management in the third stage of labor, particularly in those countries, which are developing and have rural majorities.
The authors would like to acknowledge the hospital administrative staff for their assistance in the research study.
There was no conflict of interest among the authors.
This study has been approved by the ethics review committee of the hospital.
Informed consent (written and verbal) was taken from all the parents included in the study.
All authors equally contributed in this research study.
- Gupta P, Sunita J, Shekhar C. Misoprostol versus oxytocin in prevention of postpartum hemorrhage. J Androl Gynaecol. 2016;4(1):1-4.
- Rajaei M, Karimi S, Shahboodaghi Z, Mahboobi H, Khorgoei T, Rajaei F. Safety and efficacy of misoprostol versus oxytocin for the prevention of postpartum hemorrhage. J Pregnancy. 2014;2014:1-4. doi: 10.1155/2014/713879
- Zhang Y, Yan J, Han Q, Yang T, Cai L, Fu Y, et al. Emergency obstetric hysterectomy for life-threatening postpartum hemorrhage: a 12-year review. Medicine. 2017;96(45):1-5. doi: 10.1097/MD.0000000000008443
- Ashigbie BP, Pharm B. Background Paper 6.16 Postpartum Haemorrhage. 20-22pp. Available from: https://pdf4pro.com/amp/view/background-paper-6-16-postpartum-haemorrhage-who-int-4cd74f.html
- Wormer KC, Bryant SB. Pregnancy, Acute Postpartum Hemorrhage. Stat Pearls-NCBI Bookshelf. 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499988/
- Gülmezoglu AM, Lumbiganon P, Landoulsi S, Widmer M, Abdel-Aleem H, Festin M, et al. Active management of the third stage of labour with and without controlled cord traction: a randomised, controlled, non-inferiority trial. Lancet. 2012;379(9827):1721-1727. doi: 10.1016/S0140-6736(12)60206-2
- Khan RU, El-Refaey H, Sharma S, Sooranna D, Stafford M. Oral, rectal, and vaginal pharmacokinetics of misoprostol. Obstet Gynecol. 2004;103(5):866-870. doi: 10.1097/01.AOG.0000124783.38974.53
- Allen R, O’Brien BM. Uses of misoprostol in obstetrics and gynecology. Rev Obstet Gynecol. 2009; 2(3):159-168. doi: 10.3909/riog0055
- Javed SA, Anjum MD, Imran W, Haider A, Shiraz A, Shaheen F, et al. Correlates of preferences for home or hospital confinement in Pakistan: evidence from a national survey. BMC Pregnancy Childbirth. 2013;13(1):1-6. doi: 10.1186/1471-2393-13-137
- Frass KA. Postpartum hemorrhage is related to the hemoglobin levels at labor: Observational study. Alexandria J Med. 2015;51(4):333-337. doi: 10.1016/j.ajme.2014.12.002
- Westhoff G, Cotter AM, Tolosa JE. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database Syst Rev. 2013(10):1-10. doi: 10.1002/14651858.CD001808.pub2
- Lumbiganon P, Hofmeyr J, Gülmezoglu AM, Pinol A, Villar J, WHO Collaborative Trial of misoprostol in the management of the third stage of labour. Misoprostol dose‐related shivering and pyrexia in the third stage of labour. Int J Obstet Gynaecol. 1999;106(4):304-308. doi: 10.1111/j.1471-0528.1999.tb08266.x
- Chaudhuri P, Mandi S, Mazumdar A. Erratum. Rectally administrated misoprostol as an alternative to intravenous oxytocin infusion for preventing post-partum hemorrhage after cesarean delivery. J Obstet Gynaecol Res. 2015;41(6):995-995. doi: 10.1111/jog.12761
- Quibel T, Ghout I, Goffinet F, Salomon LJ, Fort J, Javoise S, et al. Active management of the third stage of labor with a combination of oxytocin and misoprostol to prevent postpartum hemorrhage. Obstet Gynecol. 2016;128(4):805-811. doi: 10.1097/AOG.0000000000001626
- Bajwa SK, Bajwa SJ, Kaur H, Goraya SP, Singh A, KaurIshar H. Management of third stage of labor with misoprostol: A comparison of three routes of administration. Perspect Clin Res. 2012; 3(3):102-108. doi: 10.4103/2229-3485.100666
- Bugalho A, Daniel A, Faundes A, Cunha M. Misoprostol for prevention of postpartum hemorrhage. Int J Gynecol Obstet. 2001;73(1):1-6. doi: 10.1016/S0020-7292(01)00346-0
- Gerstenfeld TS, Wing DA. Rectal misoprostol versus intravenous oxytocin for the prevention of postpartum hemorrhage after vaginal delivery. Am J Obstet Gynecol. 2001;185(4):878-882. doi: 10.1067/mob.2001.117360
- Mansouri HA, Alsahly N. Rectal versus oral misoprostol for active management of third stage of labor: a randomized controlled trial. Arch Gynecol Obstet. 2011;283(5):935-939. doi: 10.1007/s00404-010-1466-5
- Song J. Use of misoprostol in obstetrics and gynecology. Obstet Gynecol Surv. 2000;55(8):503-510.
- Sweed M, El‐Said M, Abou‐Gamrah A, Ali M. Comparison between 200, 400 and 600 microgram rectal misoprostol before cesarian section: A randomized clinical trial. J Obstet Gynaecol Res. 2019;45(3):585-591. doi: 1111/jog.13883
- Hemorrhage P. ACOG practice bulletin no. 76. American college of obstetricians and gynecologists. Obstet Gynecol. 2006;108(4):1039-1047. doi: 10.1097/00006250-200610000-00046
- Rogers J, Wood J, McCandlish R, Ayers S, Truesdale A, Elbourne D. Active versus expectant management of third stage of labour: the Hinchingbrooke randomised controlled trial. Lancet. 1998;351(9104):693-699. doi: 10.1016/S0140-6736(97)09409-9
- Salati JA, Leathersich SJ, Williams MJ, Cuthbert A, Tolosa JE. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database Syst Rev. 2019(4):1-26. doi: 10.1002/14651858.CD001808.pub3
- Cotter AM, Ness A, Tolosa JE. Prophylactic oxytocin for the third stage of labour. Cochrane Database Syst Rev. 2001(4):1-10. doi: 10.1002/14651858.CD001808
- World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. World Health Organization; 2012 [cited 2022 Jul 21]. Available from: https://apps.who.int/iris/bitstream/handle/10665/75411/97?sequence=1
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) 4.0 https://creativecommons.org/licenses/by/4.0/
